Subcutaneous Basidiobolomycosis in an Immunocompetent Child
Kiran Aggarwal1, Aruna Chhikara2, Taru Garg3
1 Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
2 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
3 Professor, Department of Dermatology, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aruna Chhikara, Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi-110001, India.
E-mail: arunachhikara123@gmail.com
Basidiobolus ranarum is a fungus belonging to Basidiobolus genera, Entomophthorales order and Zygomycetes class. It is present in soil, decaying vegetable matter, intestines of amphibians, reptiles, fish and insectivorous bats. In humans, it presents generally as a subcutaneous infection involving trunk and limbs in immunocompetent hosts from endemic areas. We present a case of a two-year-old male who presented with two hard subcutaneous swellings since one month. Fine Needle Aspiration Cytology (FNAC) smears from the swellings showed granulomatous inflammation with many eosinophils. However, no fungal elements were identified. Incisional biopsy was done and on histopathological examination, many fungal hyphae were identified which were broad, thin-walled with sparse septations and surrounded by many granulomas along with presence of giant cells, eosinophils, lymphocytes and plasma cells in the subcutis. Splendore-Hoeppli phenomenon was also seen in subcutis. Periodic Acid Schiff (PAS) stain and Silver Methanamine (SM) stain for fungus were positive. Fungal culture was negative. A final diagnosis of basidiobolomycosis was made. Subcutaneous basidiobolomycosis, is an emerging infection that leads to diagnostic confusion, morbidity and mortality. Diagnosis requires a high index of suspicion and awareness of histomorphology of this rare fungal infection.
Fungal infection, Nodule, Skin
Case Report
A two-year-old male presented with two hard subcutaneous swellings one on right gluteal region [Table/Fig-1] and other on right inguinal region for one month duration. The lesion on the right gluteal region measured 8×4 cm and that on the right inguinal region measured 4×3 cm. The swellings were free from underlying bone. The child had no history of trauma or fever or intramuscular injections. He had a history of incision and drainage of swellings at the same sites three months back. On examination right inguinal lymphadenopathy was noticed with presence of three discrete non tender lymphnodes measuring 1.5 to 2 cm. Rest of the systemic examination was normal. The haematological findings showed mild leucocytosis (17,000/μL) with eosinophilia (Absolute Eosinophil Count 1500/μL). Erythrocyte sedimentation rate was 54 mm in 1st hour. The total and conjugated serum bilirubin, liver enzymes, serum urea, creatinine and electrolytes were within normal limits. The workup for fever was negative.
Two hard subcutaneous nodules with discolouration seen in the right gluteal region.

FNAC was performed from both the sites. The smears from the swellings showed similar morphological picture comprising of granulomatous inflammation with many eosinophils. However, no fungal elements were identified.
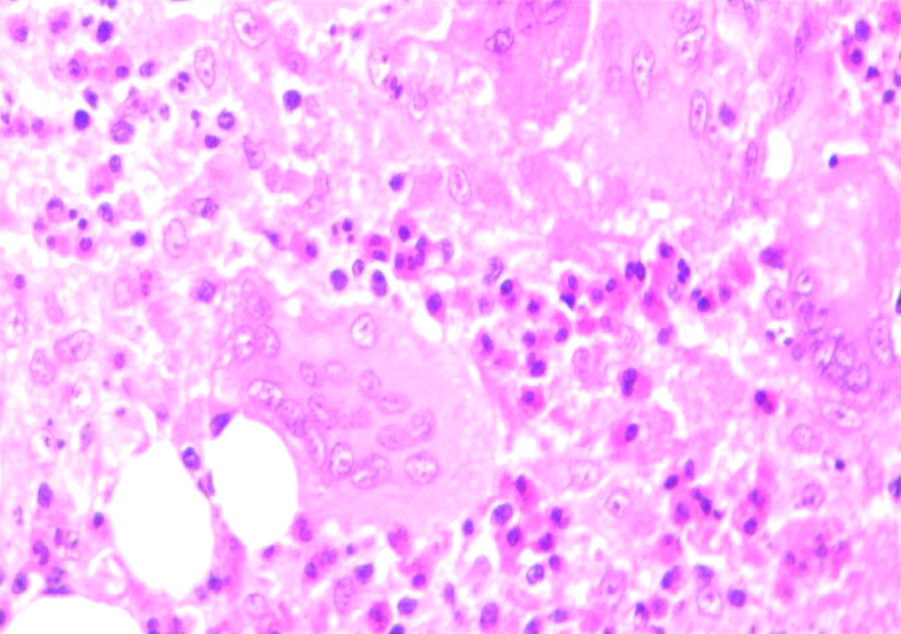
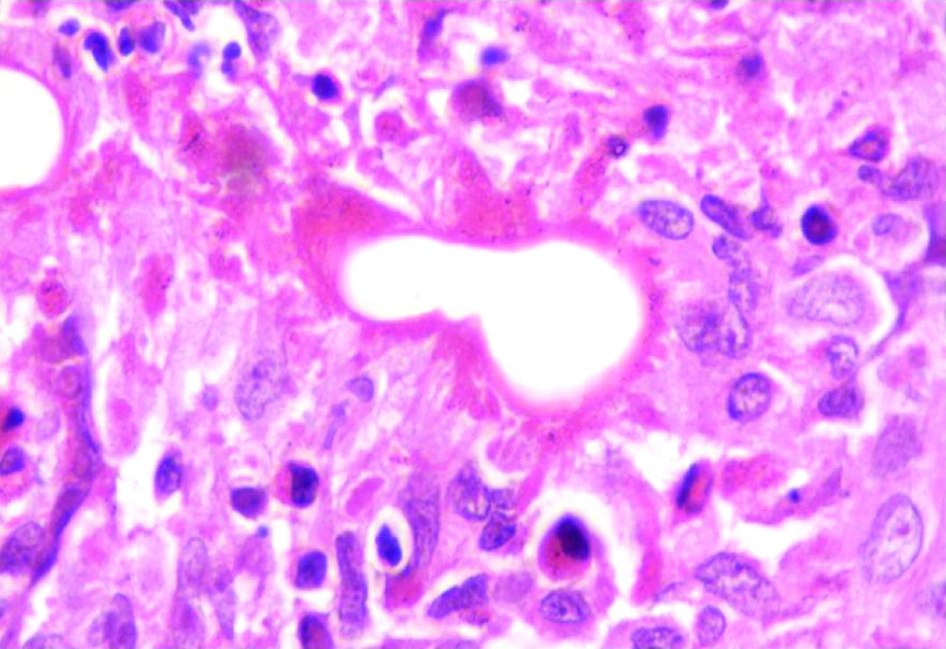
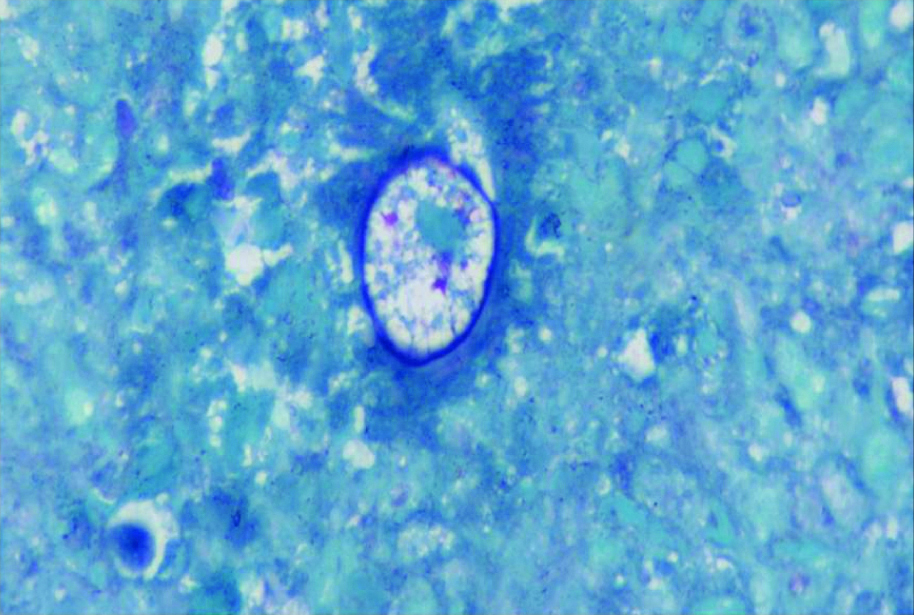
Incisional biopsy was done from both the sites. We received two skin covered tissue bits measuring 0.5 cm each. The histopathological sections showed many fungal hyphae in the subcutis. The hyphae were broad, thin-walled with sparse septations. Around the hyphae marked granulomatous reaction with presence of giant cells, eosinophils, lymphocytes and plasma cells was noticed. At few of the places the fungal hyphae showed presence of eosinophilic material around them (Splendore-Hoeppli phenomenon) [Table/Fig-2a,b and c]. Periodic Acid Schiff (PAS) stain and Silver Methanamine (SM) stain [Table/Fig-2d] for fungus were positive. Fungal culture was negative. Based on histomorphological features a final diagnosis of basidiobolomycosis was made. The complete workup of patient failed to reveal any immunocompromised state. The patient was started on oral itraconozole 200 mg daily and asked to come for follow up at one, four and six months. The patient is treated completely and doing well at the time of publication of this article.
Granulomas showing giant cells eosinophils, lymphocytes and plasma cells (H&E 100X).
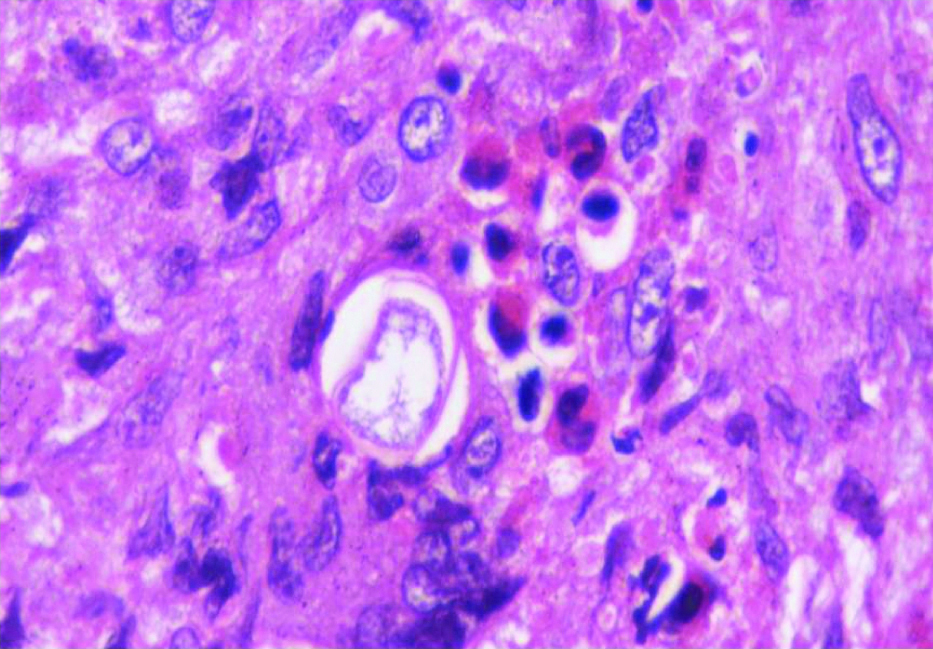
Splendore-Hoeppli phenomenon (H&E 400X).
Gomori’s methamine silver 400X hyphae are PAS positive.
Discussion
Basidiobolus are the group of fungi from the order Entomophthorales. These fungi are known to cause subcutaneous infections in healthy individuals [1]. This is an endemic fungus in Uganda and coastal areas of Africa and India [2]. These fungi grow commonly in moist soil and decaying vegetative matter. Certain organisms like amphibians, reptiles, fish and bats also harbor them in their gastrointestinal tracts [3]. Joe L et al., reported first human case of subcutaneous mycosis from Indonesia in 1956 [4]. Few authors report subcutaneous forms of this fungal infection in tropical Africa. Isolated case reports have also been reported from Asia, Australia, and South America [5]. Endemic and occasional submucosal forms have also been reported from South East India [6].
The fungi B. ranarum is known to cause chronic infection of the subcutaneous tissue, especially in the thighs and buttocks regions [7]. The lesions are mostly noted as an isolated hardened nodule, which often expands and spreads to the surrounding areas. Gradually the nodule grows and the overlying skin ulcerates. However, dissemination usually does not occur. The fungal infection has slow progressive course, even without treatment, sometimes spontaneous healing is reported. As this group of fungus is thermotolerant, they are capable of growth at 37°C. This thermotolerant capability of this fungus plays a very important role in its virulence.
The Entomophthorales are capable of infecting immunocompetent hosts. The mode of acquisition of infection by this fungus is not well known. Skin is generally the portal of entry. The fungus enters the body via skin following insect bites, scratches, and minor cuts. It is the most common skin and subcutaneous infection, in young children, especially in the thighs and buttock region [1]. Histopathological examination and fungal culture of the biopsy specimen often help to arrive at a correct diagnosis. The classical histopathological features include the presence of thin-walled, broad aseptate hyphae or hyphal fragments. These are surrounded by an eosinophilic material (Splendore-Hoeppli phenomenon). This complex is often seen phagocytosed within the giant cells. The surrounding tissue shows eosinophilic infiltrate [2,3]. On culture, the characteristic zygospore with a thick wall and pair of conical projection (tubular protuberances) are seen [3]. In 50% of the cases the fungal culture may even be negative [8]. A specific immunodiffusion test for diagnosis of this fungal disease is available only at few centers [2,3]. In the case presented, the diagnosis of subcutaneous basidiobolomycosis was based on its distinctive morphology on hematoxylin and eosin slides as well as special stains performed to demonstrate fungal hyphae.
The histological differential diagnosis of this fungal organism includes other fungi like Conidiobolus and Pythium. But these organisms are generally associated with head and neck infections in immunocompetent adults [9].
Conclusion
The present case had typical histomorphological features with negative fungal cultures. The patient was immunocompetent and resident of north India. The patient was treated with itraconozole and is doing fine at the publication of this report.
Pharmaceutical agents that used for treating Basidiobolus infections include Potassium Iodide (KI), trimethoprim-sulfamethoxazole, amphotericin B, oral azoles, or KI combined with oral azoles. The treatment of Basidiobolus is not always successful, and no single drug is effective in the treatment of all cases of basidiobolomycosis.
[1]. Zavasky DM, Samowitz W, Loftus T, Segal H, Carroll K, Gastrointestinal zygomycotic infection caused by Basidiobolus ranarum: Case report and reviewClin Infect Dis 1999 28:1244-48.10.1086/51478110451160 [Google Scholar] [CrossRef] [PubMed]
[2]. Ribes JA, Vanover-Sams CL, Baker DJ, Zygomycetes in human diseaseClin Microbiol Rev 2000 13:236-301.10.1128/CMR.13.2.23610756000 [Google Scholar] [CrossRef] [PubMed]
[3]. Gugnani HC, A review of zygomycosis due to Basidiobolus ranarumEur J Epidemiol 1999 15:923-29.10.1023/A:100765681803810669127 [Google Scholar] [CrossRef] [PubMed]
[4]. Kian Joe L, Pohan A, Tjoei Eng NI, Van Der Meulen H, Basidiobolus ranarum as a cause of subcutaneous mycosis in IndonesiaArch Dermatol 1956 74:378-83.10.1001/archderm.1956.01550100046008 [Google Scholar] [CrossRef]
[5]. Lyon MG, Smilack JD, Komatsu KK, Pasha TM, Leighton JA, Guarner J, Gastrointestinal basidiobolomycosis in Arizona: Clinical and epidemiological characteristics and review of the literatureClin Infect Dis 2001 32:1448-55.10.1086/32016111317246 [Google Scholar] [CrossRef] [PubMed]
[6]. Singh R, Xess I, Ramavat AS, Arora R, Basidobolomycosis: A rare case reportIndian J Med Microbiol 2008 26(3):265-79.10.4103/0255-0857.4204418695330 [Google Scholar] [CrossRef] [PubMed]
[7]. Jagadish Chander, Ch 25-ZygomycosisIn: Jagadish Chander Textbook of Medical Mycology 2009 3rd edIndia-New DelhiMehta publishers:378-79. [Google Scholar]
[8]. Geramizadeh B, Heidari M, Shekarkhar G, Gastrointestinal basidiobolomycosis, a rare and under-diagnosed fungal infection in immunocompetent hosts: A review articleIran J Med Sci March 2015 40(2):90-97. [Google Scholar]
[9]. Mathurvaishya VS, Tiwari N, Sekaran AS, Rao GV, Pradeep R, Basidiobolomycosis-A rare and underdiagnosed fungal infection mimicking eosinophilic colitisJ Clin Diagn Res 2017 11(10):PD13-PD15.10.7860/JCDR/2017/29890.10795 [Google Scholar] [CrossRef]