The laryngoscopy and tracheal intubation causes intense sympathetic stimulation and causes tachycardia and hypertension, albeit temporarily. This sympathetic stimulation also causes an increase in the central venous pressure, which in turn increases the IOP. The rise in IOP may cause disc ischaemia in patients who have glaucoma or open eye injury. Hence, the study was undertaken to assess the changes in IOP following tracheal intubation versus LMA insertion and to prove, whenever possible, to use a supraglottic airway device, with beneficial effects [1].
The endotracheal intubation can be stressful to the heart and the vasculature, but its effect on IOP is minimal and comparable to that of laryngeal mask airway. Hence in a patient who can tolerate the transient haemodynamic change, an endotracheal intubation should not be a contraindication [1]. Laryngoscopy and endotracheal intubation is a common method of securing the airway especially in patients who are posted for surgery under general anaesthesia, who are unable to maintain airway patency, who cannot protect the airway against aspiration, need of ventilation and oxygenation who are in respiratory or cardiac failure. However, intubation is associated with tachycardia and hypertension, which is transient. Insertion of LMA is an alternative to mask anaesthesia in the operating room, after failed intubation as a rescue device, acceptable device to endotracheal intubation especially in prehospital setting in cardiac arrest patients and as a conduit for intubation. Placement of an LMA requires neither the visualisation of cords nor the penetration of larynx, making the placement less stimulating than tracheal tube insertion and it may provoke less sympathetic response and catecholamine release [2,3]. This transient haemodynamic response has few consequences in healthy patients. However, in patients with previous myocardial infarction and those with history of Cerebral Vascular Accidents (CVA) and with aneurysm this transient response can be disastrous.
The mechanism of IOP rise is secondary to increased sympathetic activity. Adrenergic stimulation causes vasoconstriction and venoconstriction, and an increase in central venous pressure, which has a close relationship with IOP [4]. This transient increase in IOP usually does not cause any significant problems. However, in patients with glaucoma or open eye injury, this increase in IOP can cause changes in disc perfusion and cause it to reach a critical point beyond which it can lead to disc ischaemia [4].
IOP varies normally between 10 to 21.7 mmHg. Schiotz tonometer was used for measuring IOP. Schiotz tonometer is based on the principle of indentation tonometry. Indentation tonometry is based on the fact that a plunger will indent a soft eye more than a hard eye.
The present study aimed to compare the haemodynamic and IOP changes between endotracheal intubation with direct laryngoscopy and classic laryngeal mask airway insertion. The secondary objectives were to compare haemodynamic changes with endotracheal intubation and laryngeal mask airway insertion and to compare IOP changes with endotracheal tube and laryngeal mask airway insertion. An attempt was made to correlate the haemodynamic and IOP changes with endotracheal intubation or laryngeal mask airway insertion.
Materials and Methods
This was a single blind, randomised controlled trial conducted in tertiary hospitals of Kasturba Medical College, Attavar and Ambedkar circle. The duration of study was two years, from June 2014 to May 2016. After obtaining Human Institutional Ethics committee approval, sixty patients belonging to American Society of Anaesthesiologists (ASA) Grade I and II, aged between 18 to 60 years; of either sex posted for surgery under general anaesthesia were enrolled for the study. Informed and written consent was obtained from each patient.
Sample size was calculated using the following formula:
Where σ1=standard deviation of Group 1; σ2=standard deviation of Group 2; σ=average standard deviation;=the minimum difference in the values; Z(1-α/2): Z score for the alpha error chosen; 1-beta (power); Z(1-β): Z score for the power chosen.
All patients underwent a pre-operative evaluation and advised nil per oral for six hours. Each patient was premedicated with tablet diazepam 0.1-0.2 mg/kg based on patients weight two hours prior to surgery.
The patients with a known cardiovascular or respiratory disease, known diabetic or hypertensive, who were known to have glaucoma or suspected to have the same on history, those with a risk for aspiration, patients with suspected difficult airway or detected to have difficult airway during intubation, patients with ophthalmic infection or those with previous ophthalmic surgeries were excluded from the study. Also, the patients who needed the use of rapid sequence intubation technique or those with contraindication to LMA too were excluded.
Patients were allocated in one of the 2 groups. In Group 1 Classic laryngeal mask airway was used and in Group 2, patients were intubated with endotracheal tube. Patients were randomised using envelope method into either of the two groups. The patient was blinded to the group. The clinician was not blinded to the group allotted. On the day of surgery, after securing intravenous access, injection midazolam 0.02 mg/kg was given followed by injection fentanyl 2 mcg/kg. Preoxygenation was followed by induction with propofol 1-2 mg/kg in titrated dose until loss of verbal response and muscle relaxation with vecuronium (0.1 mg/kg). Using oxygen and isoflurane 1% mask ventilation was carried out by a single anaesthesiologist using appropriate face mask for three minutes. At the end of three minutes, readings of heart rate, systolic blood pressure, diastolic blood pressure, mean arterial blood pressure and IOP were taken (in right eye, using Schiotz tonometer). The Schiotz tonometer was pre-tested by the ophthalmology technician as per specifications. The eyelid of the patient was then opened and the tonometer placed at the centre of the cornea and the disc was lowered gently onto the corneal surface. The scale reading was noted and using a scale card, the noted scaled readings were converted and IOP recorded. These readings were considered as baseline as it would be uncomfortable for an awake patient when IOP is measured. Depending on the group allocated to the patient, either LMA insertion was performed (Group 1) or endotracheal tube was inserted (Group 2).
Heart rate, systolic blood pressure, diastolic blood pressure and IOP (in right eye) readings were taken at one minute, two minutes and three minutes after either tracheal intubation or LMA insertion. The change in heart rate, systolic pressure, diastolic pressure, mean pressure and IOP was calculated by subtracting the actual values from those obtained post induction.
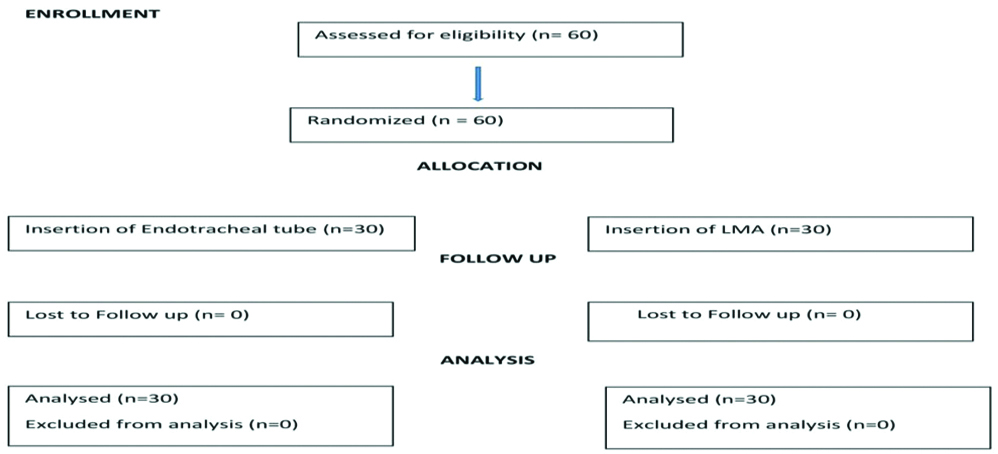
Anaesthesia was maintained with oxygen, nitrous oxide and isoflurane with intermittent vecuronium, and opioid supplementation as and when necessary. At end of surgery neuromuscular blockade was reversed with neostigmine (0.05 mg/kg) and glycopyrrolate (0.01 mg/kg). When the patient was fully awake trachea was extubated or LMA was removed whichever the case may be [Table/Fig-1].
Statistical Analysis
Statistical analysis was performed using the software IBM SPSS version 22.0, Armonk, NY: IBM Corp. Student’s unpaired t-test was done for heart rate, systolic blood pressure, diastolic blood pressure, mean blood pressure and IOP. A p-value <0.05 was considered statistically significant.
Results
Only ASA status 1 and 2 patients were included in the study. All the patients included in the study were considered. There were no rejections.
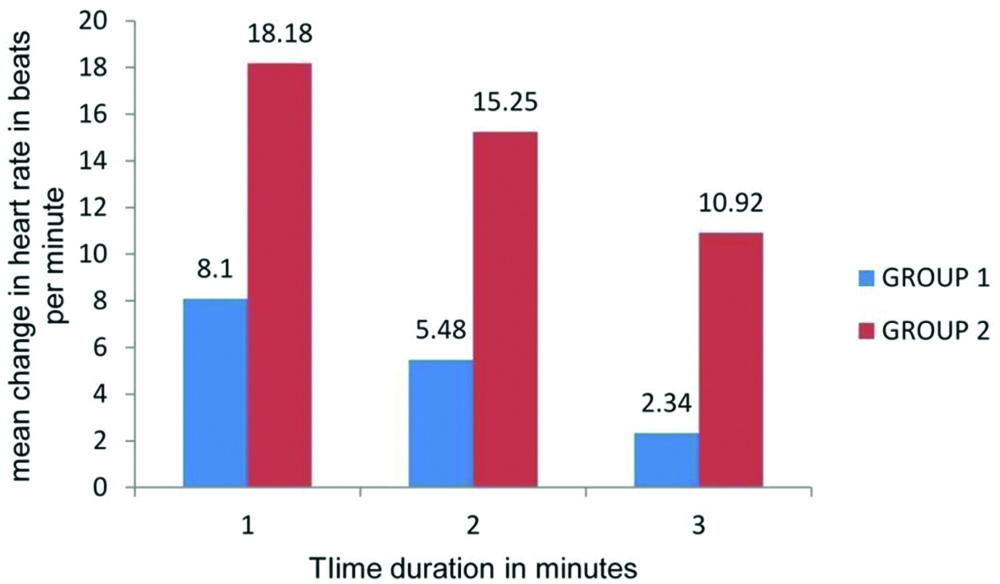
[Table/Fig-2] shows the mean distribution of age in the two groups, the mean age was comparable in both groups. [Table/Fig-3] shows the mean increase in heart rate at one minute, two minutes and three minutes from baseline. The increase is more in Group 2, with a mean of 18.18 beats per minute as compared to Group 1 which has an increase of 8.1 beats per minute. The increase is compared to the baseline for all the three minutes. The p-value comparing the change in heart rate before and after airway manipulation between the two groups at one minute is <0.001. A p-value at two minutes and three minutes was also <0.001. The 95% confidence interval for one minute, two minutes and three minutes in Group 1 are ±1.38 (range 6.72 to 9.48), ±1.47 (range 4.01 to 6.95) and ±2.09 (range 0.25 to 4.43) respectively. The 95% confidence interval for one minute, two minutes and three minutes in Group 2 are ±2.69 (range 15.49 to 20.87), ±2.76 (range 12.49 to 18.01) and ±2.52 (range 8.4 to 13.44) respectively.
| Groups | Age in years±S.D | p-value |
|---|
| Group 1 | 37.48±12.05 | 0.507 |
| Group 2 | 38.85±12.60 |
Data represented as mean±SD (Standard Deviation)
Changes in heart rate.
Data expressed as mean value; p<0.001
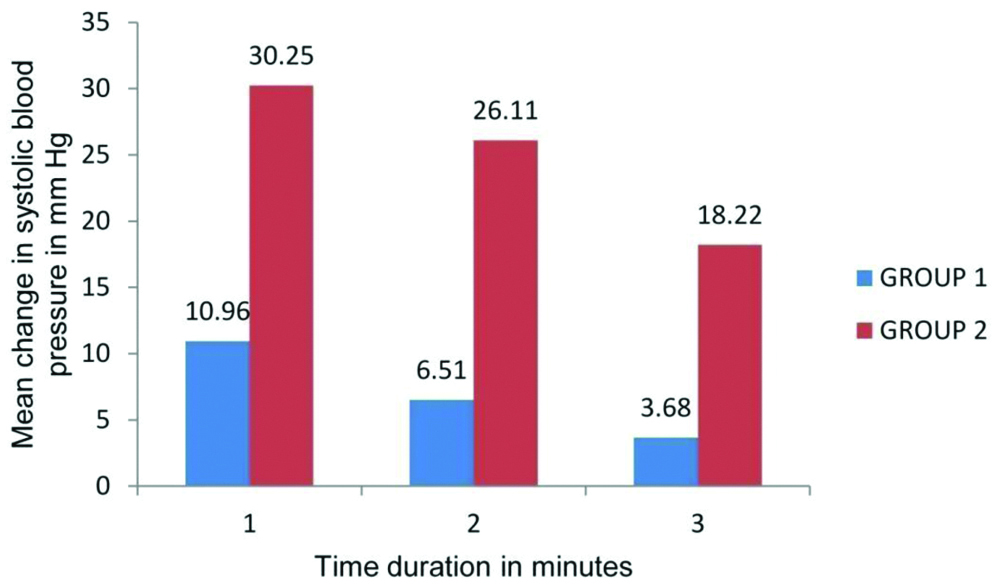
The [Table/Fig-4] shows mean change of systolic blood pressure in both groups. The increase at one minute, two minutes and three minutes in Group 1 is 10.96, 6.51 and 3.68 respectively as compared to 30.25, 26.11 and 18.22 mmHg in Group 2 (p-value, comparing the change in systolic blood pressure before and after airway manipulation between the two groups <0.001). The increase was compared to the baseline for all the three minutes. The 95% confidence interval for one minute, two minutes and three minutes in Group 1 are ±2.3 (range 8.66 to 13.26), ±3.51 (range 3.0 to 10.02) and ±2.95 (range 0.73 to 6.63) respectively. The 95% confidence interval for one minute, two minutes and three minutes in Group 2 are ±5.97 (range 24.28 to 36.22), ±4.77 (range 21.34 to 30.88) and ±3.83 (range 14.39 to 22.05) respectively.
Changes in systolic blood pressure.
Data expressed as mean value; p<0.001
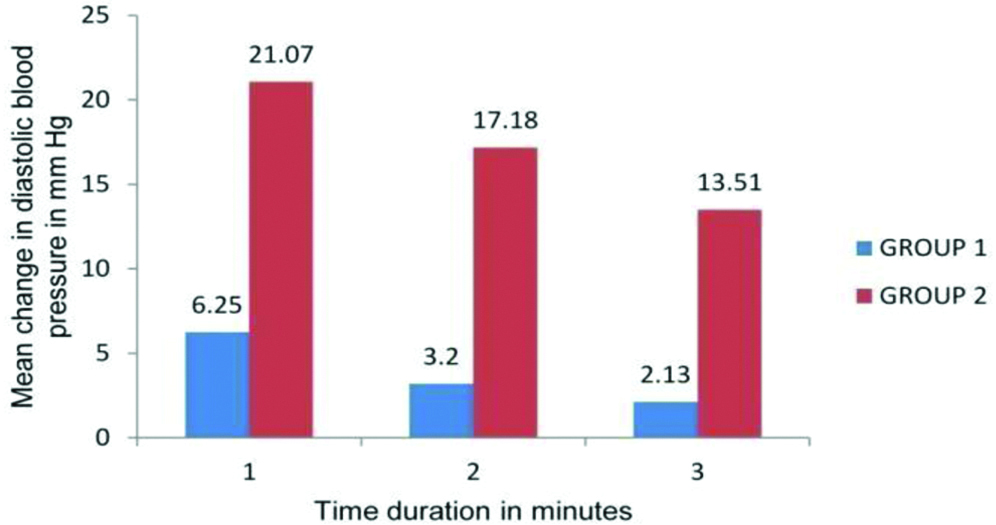
The [Table/Fig-5] shows the mean change of diastolic blood pressure in both groups. The increase at all the time the reading was taken, is more in Group 2 and was statistically significant with p-value comparing the change in diastolic blood pressure before and after airway manipulation between the two groups <0.001. The increase was compared to the baseline for all the three minutes. The 95% confidence interval for one minute, two minutes and three minutes in Group 1 were ±1.77 (range 4.48 to 8.02), ±2.97 (range 0.23 to 6.17) and ±3.1 (range -0.97 to 5.23) respectively. The 95% confidence interval for one minute, two minutes and three minutes in Group 2 were ±4.13 (range 16.94 to 25.2), ±3.57 (range 13.61 to 20.75) and ±3.42 (range 9.73 to 16.57) respectively.
Changes in diastolic blood pressure.
Data expressed as mean value; p<0.001
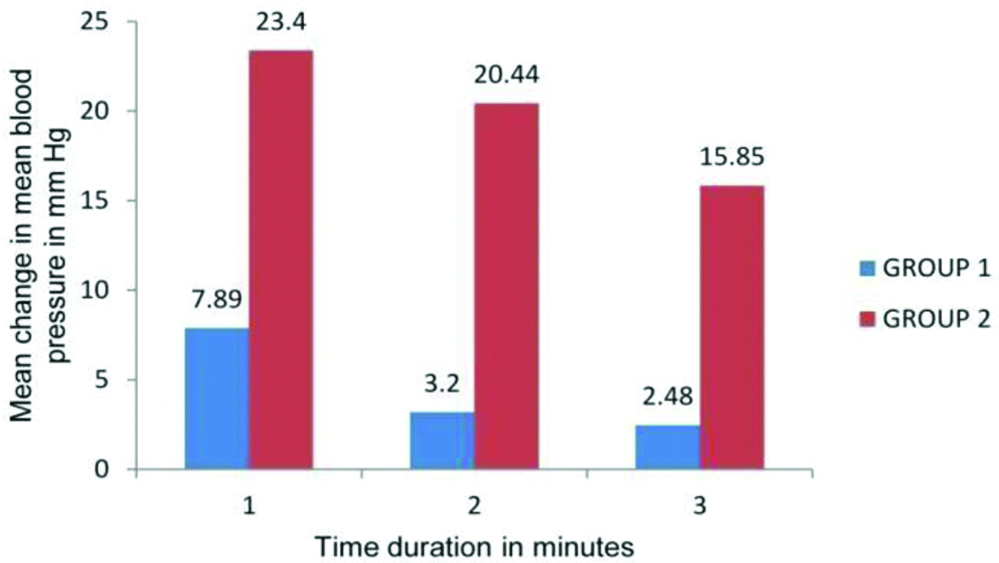
The [Table/Fig-6] shows the change of mean blood pressure in both groups. The increase was as predicted in systolic and diastolic blood pressure. The p-value, comparing the change in mean blood pressure before and after airway manipulation between the two groups, significant (p<0.001). The increase is compared to the baseline for all the three minutes. The 95% confidence interval for one minute, two minutes and three minutes in Group 1 were ±1.92 (range 5.97 to 9.81), ±3.34 (range -0.14 to 6.54) and ±3.14 (range -0.66 to 5.62) respectively. The 95% confidence interval for one minute, two minutes and three minutes in Group 2 are ±4.37 (range19.03 to 27.77), ±3.94 (range 16.5 to 24.38) and ±3.08 (range 12.77 to 18.93) respectively.
Mean blood pressure.
Data expressed as mean value; p<0.001
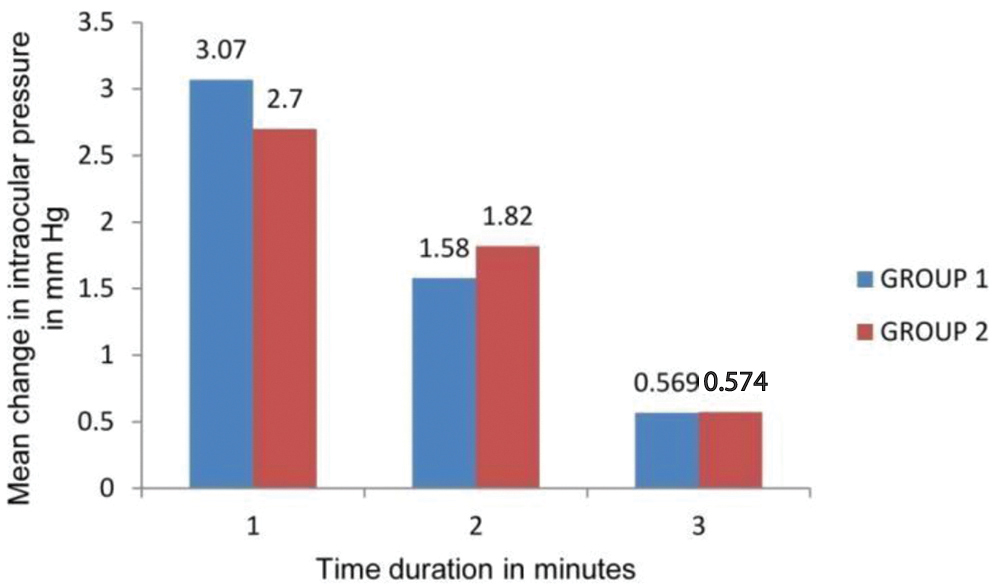
The [Table/Fig-7] shows the mean IOP change in both the groups. As opposed to change in haemodynamics the increase among two was similar and not statistically significant (p-value comparing the change in IOP before and after airway manipulation between the two groups >0.05). The increase in Group 1 at one minute, two minutes and three minutes was 3.07, 1.58 and 0.569 respectively and in Group 2 is 2.7, 1.82 and 0.574 mmHg respectively. The increase was compared to the baseline for all the three minutes. Changes in both the groups are comparable. The 95% confidence interval for one minute, two minutes and three minutes in Group 1 are ±0.62 (range 2.45 to 3.69), ±0.45 (range 1.13 to 2.03) and ±0.32 (range 0.29 to 0.94) respectively. The 95% confidence interval for one minute, two minutes and three minutes in Group 2 were ±0.53 (range 2.17 to 3.23), ±0.5 (range 1.32 to 2.32) and ±0.42 (range 0.23 to 1.06) respectively.
Changes in IOP.
Data expressed as mean value; p>0.05
Discussion
In the present study, we compared the haemodynamic and IOP changes that occur while either inserting a classical laryngeal mask airway or an endotracheal tube under direct laryngoscopic view. Authors found that the change in haemodynamic variables, heart rate, systolic blood pressure, diastolic blood pressure and mean arterial blood pressure was more in intubation group as compared to laryngeal mask airway group. Though there was increase in IOP in both the groups, the absolute value and the change from post induction value was comparable and hence statistically not significant (p>0.05). The IOP in both the groups remained within the normal range even after airway manipulation. Many studies [5-7] have been done to compare the effects on haemodynamics and IOP by using various airway manipulation techniques. Though almost all have favoured the LMA in terms of lesser haemodynamic changes, there have been conflicting results in terms of IOP. In a study that compared haemodynamic and IOP changes after endotracheal intubation and LMA insertion using propofol for induction, but without the use of muscle relaxants, they found that the mean arterial pressure and heart rate were significantly higher after endotracheal intubation compared to LMA group. But the changes in IOP were not statistically significant in both groups [6,7]. In two other similar studies [7,8], one study found that increase in both haemodynamics and IOP were more in intubation group while in the second study there was a similar smaller increase in heart rate, pressure changes, catecholamine release and IOP in LMA group. The results of the above two studies are in contradiction to the present results in terms of IOP changes but were similar in terms of haemodynamic changes. In both the above studies, thiopentone sodium was used. Hence it can be suggested that propofol used in a standard intubating dose can blunt the IOP change but not the haemodynamic changes, suggesting a different mechanism of IOP change with airway manipulation [8]. The present study was in contradiction to a study which used propofol and atracurium and found that IOP increase was statistically more in intubation group as compared to LMA group. However, in this study they measured IOP at 20 seconds post airway manipulation and at two minutes. Though they found that the mean IOP was higher at 20 seconds in endotracheal group but returned to baseline value at 2 minutes, and also did not record IOP at one minute. It has been postulated that certain drugs blunt the haemodynamic effects and IOP changes with airway manipulation [9]. Propofol and sevoflurane with a narcotic background have been shown to be effective. Balanced anaesthesia with sevoflurane and remifentanil have been found to blunt the IOP changes occurring with both endotracheal tube and laryngeal mask airway, though they did not study the haemodynamic parameters [9]. In a comparison study the control of IOP changes occurring with either sevoflurane or propofol during tracheal intubation it was found that propofol was better in blunting the IOP increase [10,11]. In the present study, authors found a similar result, propofol was able to blunt the IOP change occurring with airway manipulation, but was not effective in blunting the haemodynamic changes occurring with a laryngoscopy and endotracheal intubation. Sevoflurane was not used in the present study.
Thus the finding of present study showed that with the use of propofol haemodynamic changes with endotracheal group were much greater than the laryngeal mask airway group. However, the IOP change was comparable in both the groups.
Limitation
This study measures the change in IOP at one minute after airway manipulation. Some studies have shown that the IOP returns to baseline within one minute of airway manipulation. Hence, it is possible that IOP might have increased to statistically significant amount in the first one minute. However, since the minimum time gap between Non-Invasive Blood Pressure (NIBP) measurements on the monitor being one minute, hence IOP was also measured at one minute interval.
Conclusion
Endotracheal intubation produces a greater haemodynamic response as compared to a laryngeal mask airway insertion. However, the changes in IOP were comparable in both the groups and the increase is not statistically significant. Hence in a patient who can tolerate the transient haemodynamic change, an endotracheal intubation should not be a contraindication when minimal changes in IOP are desired. Hence though endotracheal intubation, when compared to laryngeal mask airway, can be stressful to the heart and the vasculature its effect on IOP is minimal and comparable to that of laryngeal mask airway. The changes in haemodynamic and IOP cannot be compared.
Data represented as mean±SD (Standard Deviation)