Radiation Dose Reduction and Cancer Risk Estimation Associated with Upper Limbs Radiographic Examination by using Optimal Projections: A Phantom Study
Mohamed M Abuzaid1, Wiam Elshami2, Zarmeena Noorajan3
1 Assistant Professor, Department of Medical Diagnostic Imaging, University of Sharjah, College of Health Sciences, Sharjah, United Arab Emirates.
2 Assistant Professor, Department of Medical Diagnostic Imaging, University of Sharjah, College of Health Sciences, Sharjah, United Arab Emirates.
3 Clinical Tutor, Department of Medical Diagnostic Imaging, University of Sharjah, College of Health Sciences, Sharjah, United Arab Emirates.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohamed M Abuzaid, Assistant Professor, Department of Medical Diagnostic Imaging, University of Sharjah, College of Health Sciences, Sharjah, United Arab Emirates.
E-mail: mabdelfatah@sharjah.ac.ae
Introduction
Ionising radiation used during medical imaging examinations should be monitored carefully to reduce the radiation harm and biological effects. In radiography, As Low As Reasonably Achievable (ALARA) principles should be applied during patient positioning by placing the patient sensitive organs away from the radiation beam.
Aim
To determine the Entrance Skin Dose (ESD), effective dose and Lifetime Attribute Risk (LAR) of cancer in eye and gonad area when positioning the patient facing towards the primary radiation beam and facing away from it.
Materials and Methods
An experimental study conducted using an X-ray phantom to simulate patient position during upper limb radiography. Radiation measurement was done by using TLD placed at the level of the eye and gonads and two different imaging orientations were used (standard and modified). The ESD, effective dose was calculated from TLD’s readings. The BEIRVII report was used to estimate the LAR of cancer.
Results
Results showed significant ESD, effective dose, and LAR reduction when the patient was sitting beside the table and not facing the radiation beam. Results indicate that there were significant differences in ESD and ED to the eye and gonads between the different patient orientations. In terms of eye dose, there is a dose difference of 12% between the two projections. For gonad gland doses there is a dose difference of 50% with p-value <0.001.
Conclusion
This study confirmed the relation between dose reduction and patient orientation and it aligns with the ALARA principle to ably all efforts to minimise unnecessary radiation exposure.
Cancer risk, Radiation protection, Radiography
Introduction
Radiology and medical imaging have earned a significant place in the medical field, and they have become the most efficient and crucial diagnostic tool. Patients having medical imaging examinations are exposed to harmful radiation that has detrimental biological effects. There is no doubt that an effort should be made to reduce the radiation dose for the patients based on the ALARA principle radiography is a necessary procedure in diagnosis and treatment of patients with dental problems [1-6]. According to the ALARA. ALARA is the responsibility of the radiographers and is attained by applying the standard patient positioning and selecting the appropriate exposure factors. Radiographers who use radiation for medical purposes must ensure that their patients are not exposed to any unnecessary doses of radiation, and any recurrent or repeated examinations that outweigh the harmful effects [6]. The procedure techniques should be accompanied by specific instructions to ensure production of high-quality images with minimum radiation dose. Radiographer should perform essential steps in term of positioning, exposure parameters, patient instruction, and radiation protection to obtained high diagnostic image quality. Radiographic position and projection must be made to ensure that the patient is comfortable and able to maintain the position during the exposure [7].
During radiographic positioning, it is recommended to ensure that the patient is not facing the primary radiation beam to protect the sensitive organs such as eyes, thyroid and gonads [7]. Special care to collimate the beam to the area of interest, avoiding the unnecessary irradiation and reducing scatter radiation. When more radiation-sensitive organs are located in the image-acquisition field, these should be excluded whenever possible, e.g., the modification of projections to reduce irradiation of the lens of the eye or the thyroid gland [8].
Based on the X-ray interaction with the matter, the Compton, and photoelectric effect, the photon flux decreases inside the body from the entry area of the beam towards the image receptor. Absorbed dose to the tissue and organs decreased while the photons pass through the body [9]. Organs and tissues located closest to the X-ray beam and at the primary beam field absorb highest radiation dose. The International Commission on Radiological Protection (ICRP), sets tissue weighting factors for each organ to determine the organ radiation sensitivity, it uses to determine the contribution of individual tissues and organs to the overall radiation detriment from genetic effects and stochastic effects like cancer [10].
The present study aimed to determine the ESD, effective dose and LAR of cancer in eye and gonad area when positioning the patient facing towards the primary radiation beam and facing away from it.
Materials and Methods
This is an experimental study conducted at University of Sharjah, Medical Imaging Laboratory between January-February 2018. For the objective of this investigation institutional ethics committee approval was not required. The experiment was performed using Philips X-ray unit with total filtration 2.5 mm Aluminum equivalent. X-ray unit was calibrated, and quality assurance measures were performed on regular basis as well as before the experiment according to IPEM 91 report, and the results fell within an acceptable range [11]. The images obtained using digital radiography system by Agfa HealthCare Instant DR solution, which includes the NX image acquisition software with MUSICA processing and detector.
Radiographic Procedures
The experiment included radiographic examinations of three body parts (hand, wrist and elbow). An adult phantom was used to simulate the patient position and orientation during hand, wrist and elbow radiographic procedure. The radiographic technique, positioning, centring point, collimation, exposure parameter, SID, set according to Merrill’s Atlas of Radiographic Positioning and Procedures [12]. Exposure parameters were peak tube potential 60 kVp, mAs were set at 2, 2.5 and 3.2 for hand, wrist and elbow accordingly, 100 cm SID, no tube angulation, no grid and fine focal spot. FOV was adjusted in order to include the desired region of interest.
Dose Measurements
Thermo Luminescence Dosimetry (TLD) is an essential tool in clinical, personal and environmental monitoring of Ionising radiation. The TLD-100 card was of Harshaw™ design, (LiF: Mg, Ti) used to obtain radiation dose to the eye and gonads. The Lithium Fluoride (LiF) is near tissue equivalent, provide excellent energy response and not sensitive to light, it is suitable for research and clinical with linear range 10 mGy-1Gy. The TLD dosimeter processed using Harshaw TLD card reader Model 6600 plus, it is able to measure photon energy >5 keV, Neutrons from thermal to fast, Beta, energy >70 keV [13].
Data Collection
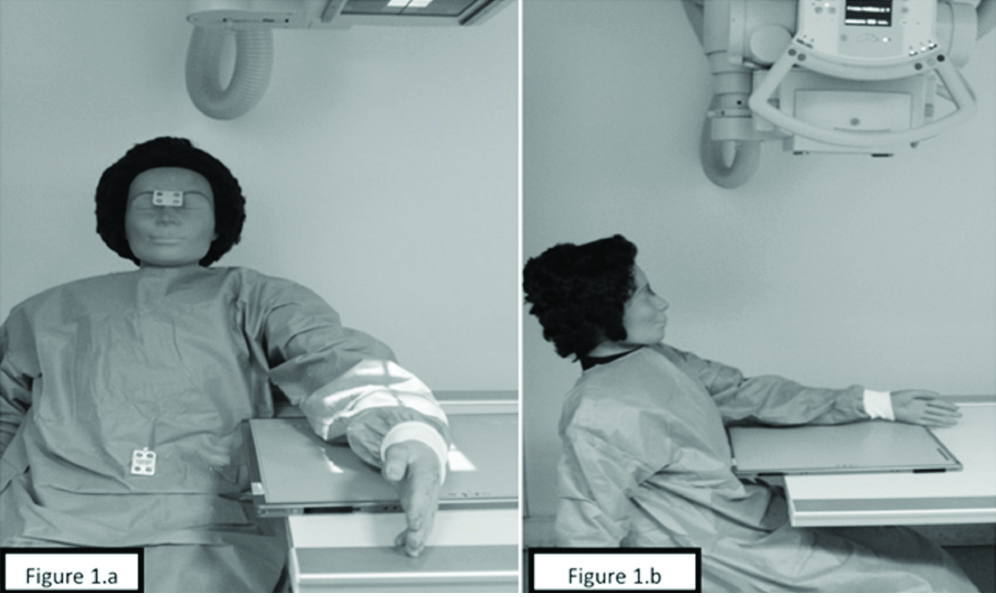
Two patient orientations were simulated: (i) standard sitting position; where the gonad and eye were positioned away from the radiation beam direction and the leg beside the table [Table/Fig-1a]; and (ii) modified sitting position whereas patient facing the radiation beam and leg positioned under the table [Table/Fig-1b]. TLD’s were placed at the eye level and gonad area. Twenty radiographic examinations were performed for each body part including standard and modified positions. Following the exposure, the ESD, effective dose was calculated from TLD’s readings and average ESD and average effective dose were used for LAR estimation.
a) Standard patient orientation; b) Modified patient orientation.
Calculation of Estimated Cancer Risk
BEIRVII report was used to estimate the LAR of cancer due to radiation dose [14,15]. The report is based on a 100 mSv equivalent dose for different age, sex, and organ. For the phantom used in the study, linear interpolation was performed from the nearest two ages (30 and 40). The LAR calculation based on the dose received by the patient and measured by the TLD. For example, using BEIR VII model the LAR to calculate prostatic cancer for a male 35-year-old who received 100 mSv is 35 cases per 100,000. Therefore, the LAR from 6.5 mSv received during modified upper limbs patient orientation is (6.5/100)×(35/100,000)=0.0023%. The whole body LAR was estimated by summing organ-specific LARs. The using of BEIR VII methods employed in this study were used before in a similar study [16].
Statistical Analysis
Statistical packages for the Social Sciences software (SPSS, version 23.0, by the SPSS, USA) used for data analysis. A t-test was used to compare different data obtained for each pair orientations. The differences were statically significant, if p-value was <0.05.
Results
Radiographic exposure was performed for the phantom simulating the two patient orientation. A total of 20 exposures for each projection performed followed by the collection of ESK, ED and LAR calculation. Kolmogorov-Smirnov Test of normality was conducted to examine if the data to be tested had a normal distribution. The test of normality between patient position and radiation dose resulted in a normal distribution (p>0.05). The main difference between the two positions (standard-position and modified position) ED, ESD for the eye and testes is tested using two-way ANOVA, mean and Standard Deviation (SD). Results indicate that there were difference between the radiation dose received by the eyes and gonads in different patient orientation. [Table/Fig-2] showed the comparisons of effective doses (mSv), ESD of the eye and tests for each patient orientation. The ESK reduced by 12% and 50% and the ED dose reduce by 50% for the eyes and gonads respectively. Results showed significant ESD, effective dose, and LAR reduction when the patient was sitting beside the table and not facing the radiation beam [Table/Fig-3].
Comparisons of ESD and ED of the eye and the testes for each orientation.
| Projection | ESD (mGy) (EYE) | ±SD | ESD Reduction% | ESD (mGy) Testes | ±SD | ESD Reduction% | ED (mSv) | ±SD | ED Reduction% | p-value |
| Modified orientation | 3.3 | 0.6 | 12% | 6 | 1.3 | 50% | 6.5 | 1 | 49% | <0.001 |
| Standard orientation | 2.9 | 0.5 | 3 | 0.7 | 3.3 | 0.8 |
Organ Specific LAR for radiation dose received during each patient orientation.
| Variables | Organ-Specific LAR for radiation dose received (%) | Reduction % |
|---|
| Modified orientation | Standard orientation |
|---|
| Stomach | 0.0018 | 0.0009 | 50.0 |
| Colon | 0.0080 | 0.0041 | 51.3 |
| Liver | 0.0014 | 0.0007 | 50.0 |
| Lung | 0.0068 | 0.0034 | 50.0 |
| Prostate | 0.0023 | 0.0012 | 52.2 |
| Bladder | 0.0051 | 0.0026 | 51.0 |
| Other | 0.0120 | 0.0061 | 50.8 |
| Thyroid | 0.0004 | 0.0002 | 50.0 |
| All solid | 0.0379 | 0.0192 | 50.7 |
| Leukemia | 0.0055 | 0.0028 | 50.9 |
Discussion
The results of this study highlighted the importance of applying the proper patient positions during radiographic examination examinations of upper limbs to reduce the stochastic harm of Ionising radiation. Diagnostic imaging modalities will keep on giving considerable advantages to modern healthcare. In spite of the fact that the benefit the patient receives from an adequately conducted radiological exam outweighs the risks, quantification of such risks is vital. Consideration should be made to reduce the entrance surface dose to the sensitive organs during upper limbs projection. Patient doses can be reduced significantly by the use of common ALARA principle, which includes most proper distance from the source of radiation and application of protective lead shielding as well as applying the appropriate patient positioning, exposure factor, and SID. In this study, the ESD, effective dose, LAR for cancer risk was estimated for an adult 32 years who underwent upper limbs radiography. The main reason for conducting this study is to ensure appropriate positions are adopted during medical imaging procedures. It is noticed that in some practices, the patient orientation facing the radiation beam and legs positioned under the table during exposure, such methods increase the radiation harm to the patients from Ionising radiation. The ESD at the level of the eyes and testes were measured in both orientations for comparison of the radiation effects in different projections. Many studies were conducted on other radiographic projection such as the lumbar spine, abdomen, pelvis, and clavicle had been done to compare between the effect of different patient orientation and projection on the amount of radiation dose the patient receives [17,18].
The [Table/Fig-2] shows a reduction of the effective dose 49% (P<0.001) when the patient does not face the radiation beam as well as reduction of the ESD to the eye and testes by 12% and 49% respectively. This reduction associated with the decrease in the LAR risk by 50.7%. Measuring the dose received by the testes can be used to estimate the genetic risk arising from radiation for men and women in reproductive age and this fact has also been confirmed in the recent report of ICRP (ICRP 121). The LAR for the prostate cancer in this study reduced by 48%. The current study demonstrated consistent significant dose-reductions to the thyroid and gonads when patients are seated either on the right or left side of the table rather than placing the lower limb under the table.
Limitation
Although the modified projection is used during radiography practice, it is not possible to apply the same experiments on real patients. The experimental context of the study provide a simulated situation that uses an average patient but it may not fully represent the real-life circumstances as other factors such as patient size, weight and height might affect the patient radiation dose.
Conclusion
Although the recommended projection is based on patient’s co-operation, conditions, and anatomical part, it is critical to ensure image quality and radiation dose. In some other body parts and projections, there were no significant differences in image quality, i.e., the image quality dose not degraded or improved in the chosen projection. The orientation and projection of the radiation beam do not affect the patient comfort because the patient responses will not change whether the patient is facing or sitting beside the table. This study confirmed the relation between dose reduction and patient orientation and it aligns with the ALARA principle to apply all efforts to minimise unnecessary radiation exposure.
[1]. Toossi MTB, Akbari F, Roodi SB, Radiation exposure to critical organs in panoramic dental examinationActa Med Iran 2012 50(12):809-13. [Google Scholar]
[2]. Jibiri NN, Adewale AA, Estimation of radiation dose to the lens of eyes of patients undergoing cranial computed tomography in a teaching hospital in Osun state, NigeriaInt J Radiat Res 2014 12(1):53-60. [Google Scholar]
[3]. Mokhtari-Dizaji M, Sharafi AA, Larijani B, Mokhlesian N, Hasanzadeh H, Estimating the absorbed dose to critical organs during dual X-ray absorptiometryKorean J Radiol 2008 9(2):102-10.10.3348/kjr.2008.9.2.10218385556 [Google Scholar] [CrossRef] [PubMed]
[4]. Kandaiya S, Lim TH, Chumiran SH, Preliminary study on the trend of patient dose arising from diagnostic X-ray examination in Penang, MalaysiaJ Appl Sci Res 2010 6(12):2257-63. [Google Scholar]
[5]. Aliasgharzadeh A, Mihandoost E, Masoumbeigi M, Salimian M, Mohseni M, Measurement of entrance skin dose and calculation of effective dose for common diagnostic X-Ray examinations in Kashan, IranGlob J Health Sci 2015 7(5):202-07.10.5539/gjhs.v7n5p20226156930 [Google Scholar] [CrossRef] [PubMed]
[6]. Olgar T, Bor D, Berkmen G, Yazar T, Patient and staff doses for some complex X-ray examinationsJ Radiol Prot 2009 29(3):393-407.10.1088/0952-4746/29/3/00419690354 [Google Scholar] [CrossRef] [PubMed]
[7]. Whitley S, Sloane C, Hoadley G ADM, Clark’s positioning in radiography 2016 CRC Press10.1201/b13534 [Google Scholar] [CrossRef]
[8]. Sulieman A, Elzaki M, Alkhorayef M, Babikir E, Abuzaid M, Dalton A, Assessment of patient dose and radiogenic risks during endoscopic retrograde cholangiopancreatographyAppl Radiat Isot [Internet] 2016 117:65-69.Available from: http://dx.doi.org/10.1016/j.apradiso.2016.03.01010.1016/j.apradiso.2016.03.01026994755 [Google Scholar] [CrossRef] [PubMed]
[9]. Dietze G, Streffer C, Alberts CMW, Balonov M, Berkovski V, Bouville A, Basis for dosimetric quantities used in radiological protectionInternational commission on radiological protection committee 2005 [Google Scholar]
[10]. ICRP. The 2007 Recommendations of the International Commission on Radiological Protection. Vol. 37, ICRP, 2007. ICRP Publication 103. 2007 [Google Scholar]
[11]. Scally AJ, Recommended Standards for the Routine Performance Testing of Diagnostic X-Ray Imaging SystemsIPEM Report 91 2005 [Google Scholar]
[12]. Philip W, Ballinger EDFMerrill’s atlas of radiographic positions and radiologic procedures 1999 3:131-73. [Google Scholar]
[13]. Abuzaid MM, Elshami W, Steelman C, Measurements of radiation exposure of radiography students during their clinical training using thermoluminescent dosimetryRadiat Prot Dosimetry 2018 179(3):1-4.10.1093/rpd/ncx26129186490 [Google Scholar] [CrossRef] [PubMed]
[14]. Calabrese EJ, O’Connor MK, Estimating Risk of Low Radiation Doses - A Critical Review of the BEIR VII Report and its Use of the Linear No-Threshold (LNT) HypothesisRadiat Res 2014 182(5):463-74.10.1667/RR13829.125329961 [Google Scholar] [CrossRef] [PubMed]
[15]. De Gonzalez AB, Iulian Apostoaei A, Veiga LHS, Rajaraman P, Thomas BA, Owen Hoffman F, RadRAT: A radiation risk assessment tool for lifetime cancer risk projectionJ Radiol Prot 2012 32(3):205-22.10.1088/0952-4746/32/3/20522810503 [Google Scholar] [CrossRef] [PubMed]
[16]. Tarin TV, Sonn G, Shinghal R, Estimating the risk of cancer associated with imaging related radiation during surveillance for stage I testicular cancer using computerized tomographyJ Urol 2009 181(2):627-33.10.1016/j.juro.2008.10.00519091344 [Google Scholar] [CrossRef] [PubMed]
[17]. Chaparian A, Kanani A, Baghbanian M, Reduction of radiation risks in patients undergoing some X-ray examinations by using optimal projections: A Monte Carlo program-based mathematical calculationJ Med Phys 2014 39(1):3210.4103/0971-6203.12550024600170 [Google Scholar] [CrossRef] [PubMed]
[18]. Gialousis GI, Yakoumakis EN, Papadopoulou DI, Makri TK, Yakoumakis NE, Dimitriou PA, Differences in effective dose and energy imparted estimation from PA-AP, RLAT-LLAT projections in pediatric full spine X-ray examination using the Monte Carlo techniquePhys Med Biol 2006 51(2):287-97.10.1088/0031-9155/51/2/00716394339 [Google Scholar] [CrossRef] [PubMed]