Dental Implant Rehabilitation in a Young Patient with Generalised Aggressive Periodontitis
Mhd Ammar Kouki1, Majd Othman2, Ali Abou Sulaiman3
1 MSc, Department of Periodontology, Damascus University, Damascus, Syria.
2 PhD, Department of Periodontology, Damascus University, Damascus, Syria.
3 PhD, Department of Periodontology, Damascus University, Damascus, Syria.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mhd Ammar Kouki, Department of Periodontology, Faculty of Dental Medicine, Damascus University, Mazzeh Highway, Damascus, Syria.
E-mail: koukyammar@gmail.com
Generalised aggressive periodontitis is a disease that manifests in young patients and causes progressive damage to the periodontium. This report describes the treatment plan of a young patient aged 34 years with generalised aggressive periodontitis. Two implants in each jaw were placed two months after the extraction of all the teeth. After a healing period, an implant-retained prosthesis was fabricated and installed. The patient showed a high level of satisfaction with the provided treatment. Implant-retained denture is an adequate and relatively cheap treatment option for the rehabilitation of edentulous young adults with generalised aggressive periodontitis.
Denture, Edentulism, Implantation
Case Report
A 34-year-old healthy Syrian male patient was referred to the Department of Periodontology at Damascus University with a chief complaint of generalised teeth mobility and bleeding gums. Complete medical and dental history was obtained, and a thorough oral examination was performed. A full periodontal chart was recorded including all clinical periodontal parameters: Plaque Index (PI), Bleeding On Probing (BOP), Recession, Tooth Mobility (TM), Furcation Involvement (FI), Probing Pocket Depth (PPD), and Clinical Attachment Level (CAL).
The patient showed a general dissatisfaction with the oral condition both aesthetically and functionally, and reported that his mouth condition had worsened over the past three years.
The periodontal chart revealed that teeth number 11, 12, 13, 18, 22, 24, 31, 47, 48 were missing, a grade III mobility in all teeth except teeth 26 and 36 that showed grade II mobility. The presence of generalised heavy plaque and calculus accumulation indicated poor oral hygiene practice, bleeding index of 92% with deep probing pocket depth varying from 3-6 and severe CAL >8 mm was found in the majority of the patient’s teeth.
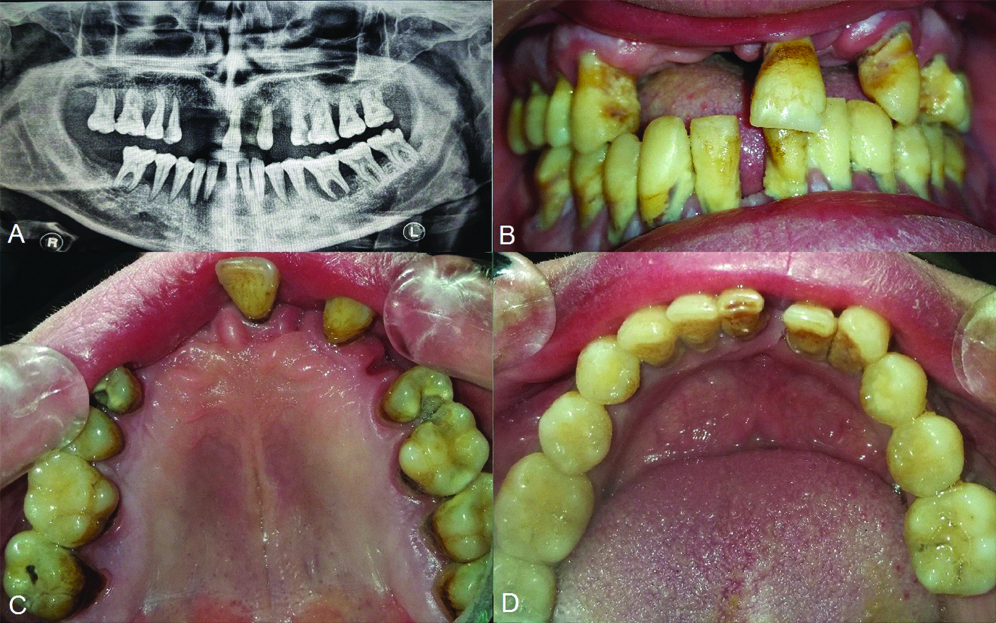
The clinical findings and radiographic examination were in accordance with criteria for Generalised Aggressive Periodontitis (GAgP) [Table/Fig-1] [1].
(A) Pre-operative panoramic radiograph demonstrating the bone level around the remaining teeth; (B) Frontal view showing the accumulation of plaque and calculus; (C) Clinical view of the remaining teeth in the upper jaw; (D) Clinical view of the lower jaw showing the remaining teeth.
The initial treatment phase included a two-staged extraction approach. All teeth were extracted except for the upper and lower left third molars, and the upper and lower right first molars. The extraction of these teeth was delayed in order to preserve the vertical width and facilitate the fabrication of a provisional denture. The remaining teeth were extracted and the provisional denture was installed. Two months later, Cone Beam Computed Tomography (CBCT) was done and bone measurements were calculated and suitable implant sites were determined.
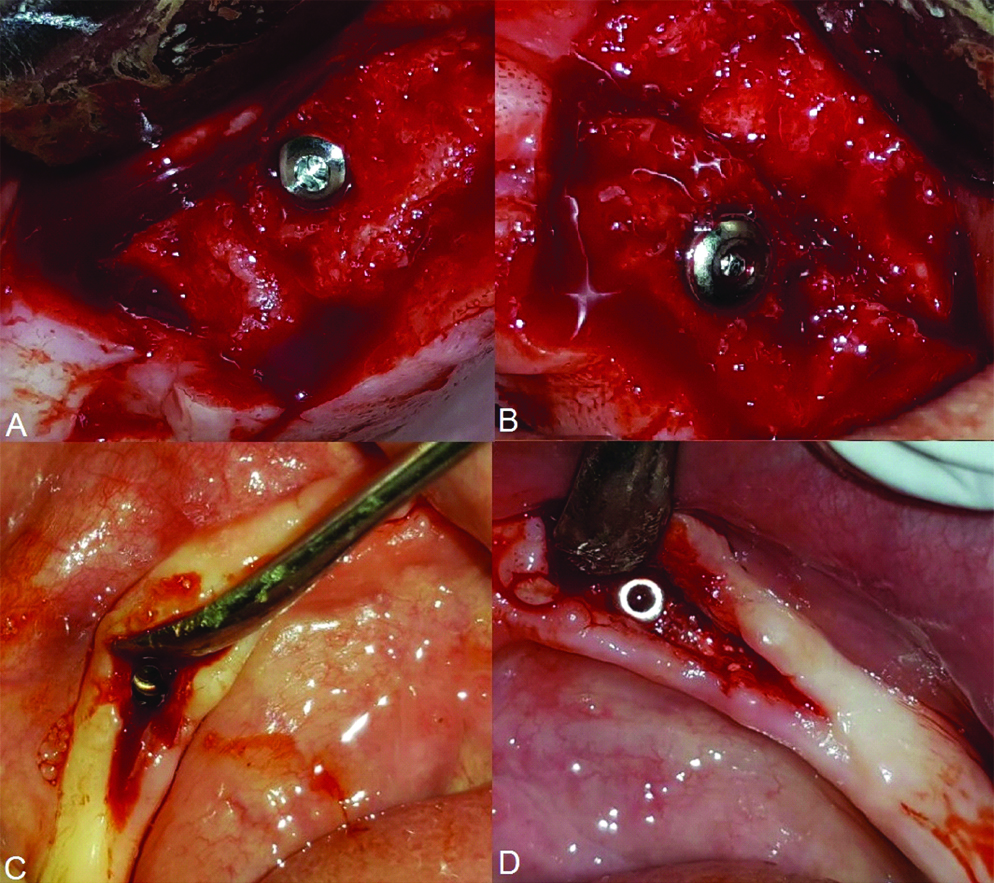
The second phase of the treatment plan included the placement of four implants (One Q system, Dentis, Seoul, South Korea). Firstly, two implants were placed in the anterior maxilla [Table/Fig-2]. Subsequently, after two weeks, two additional implants were placed in the anterior mandible. All implants were placed in an approach torque and no post-surgical complications were observed [Table/Fig-2].
(A) Placement of 4.2*12 implant in the right side of the maxilla; (B) Placement of 3.7*12 implant in the left side of the maxilla; (C) Placement of 3.7*12 implant in the left side of the mandible; (D) Placement of a 3.3*12 implant in the right side of the mandible.
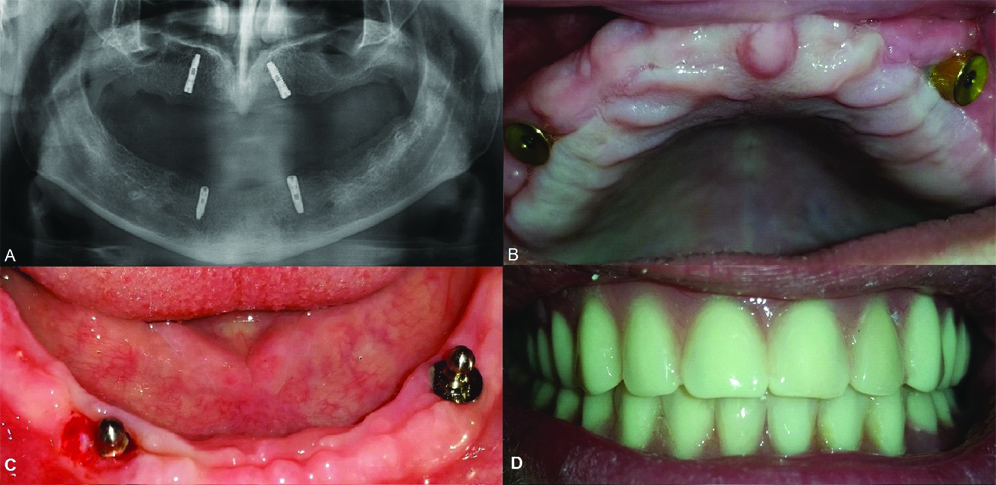
Healing abutments were mounted after three months healing period for mandibular implants and four months for maxillary implants. Two weeks later, the restorative process started and ball abutments were the preferred choice for the denture support in the mandibluar implants, whilst magnetic abutments were preferred in the maxilla [Table/Fig-3].
(A) Panoramic radiograph post implantation; (B) Installing the abutments and screws in the maxilla to be assembled with the magnets in the prosthesis; (C) Installing ball abutments in the mandible to be assembled with the metal cap in the prosthesis; (D) Clinical view of the final prosthesis after being mounted on the implants.
Standard prosthodontics concepts were applied to produce a definitive cast, which involved a polyether impression, and maxillomandibular relationship was recorded.
After mounting the ball abutments and the keeper abutments (abutment and screw), we used acrylic resin to attach the metal caps that contain the O rings to the base of the lower denture and the magnet to the base of the upper denture. This process was done intraorally.
Recall visits were planned at six and twelve month’s intervals after the installation of the denture. At both time points, the patient demonstrated good oral hygiene. The O rings were replaced at the second recall visit. During these maintenance appointments, the tissues around the implants looked normal with no inflammation and the probing depths were within normal levels. Nonetheless, oral hygiene instructions were reinforced.
Discussion
Aggressive Periodontitis (AgP) represents one of the most challenging conditions that dentists encounter despite being less prevalent than chronic periodontitis [2]. Studies have reported that even with good oral hygiene and maintenance visits there is a chance that GAgP could relapse [3]. GAgP is characterised by rapid progressive tissue destruction encompassing both soft and hard tissue that eventually renders the teeth hopeless and poses a challenge for making a proper treatment plan that ensures both aesthetic and functional rehabilitation [3]. Individuals with GAgP may experience edentulism at a very young age, affecting mastication, aesthetics, and pronunciation and enunciation [3]. Hence, a successful treatment plan for edentulous patients should focus on these aspects while still taking into account the cost of treatment for the patient [4]. A recent study has shown that the impact of such diseases on the quality of life is more prominent in young adults [5]. This could be attributed to the fact that older adults consider tooth loss as a normal outcome to ageing [5]. The negative effect on the quality of life is an accompanying outcome to generalised aggressive or chronic periodontitis compared to the localised form. This effect could be noticed as a psychological or physical annoyance [6]. On a parallel note, another study has concluded that psychological stress plays a crucial role in provoking the inflammatory process in aggressive and chronic periodontitis [7].
Treatment options might include: conventional removable complete dentures, implant-retained dentures and implant-supported dentures. The conventional removable complete dentures may not be the best choice for young patients due to the lack of retention that happens because of the massive bone loss. On the other hand, the implant-retained dentures seem to be a good choice compared to the conventional one since it requires two to four implants in each jaw to provide a fair retention to the denture. Implant-supported dentures provide the best retention with a greater capacity when it comes to the load the denture can handle. However, implant-supported dentures require four to six implants to support the denture which cannot be achieved in all cases of aggressive periodontitis [8]. Prosthesis designed as denture that uses tissue and implant support is likely to be the better choice when an excessive cantilever to obtain occlusal contact is required. Conversely, implant retained dentures could be unfavorable for patients who have sensitive mucosa or knife-edged ridges [4]. A comprehensive discussion regarding the advantages and disadvantages of the three aforementioned treatments was held with the patient. Owing to the patient preference and his financial status, implant-retained denture was chosen as the optimal option.
In the present case, we decided to extract all the teeth using staged-extraction approach which makes the fabrication of the temporary denture easier. After two months, the second phase of the treatment started which is the implantation stage. In the Implantation stage, we chose to place two implants in each jaw due to the restricted resources of the patient and the lack of good bone width and height. And after a four-month healing period, the third phase of the treatment plan started which is the fabrication of implant-retained complete denture. Five weeks post-installation of the denture and its daily usage by the patient, significant improvement was noticed in the psychological state of the patient. A remarkable change in his attitude and behaviour was observed as he was no longer covering his mouth while speaking and was more confident and outgoing during social activities. Likewise, the patient reported a high level of satisfaction with his ability to chew and articulate. The final assessment of the patient’s overall status revealed a better quality of life. He reported increased satisfaction towards the treatment benefits in both function and aesthetics.
While there are limited studies in literature that have evaluated the success rate of implant placement in AgP patients, a publication by Monje A et al., has demonstrated that implantation in patients with GAgP is a reliable option and that the implant survival rates are close to the ones in healthy patients [9]. Similarly, Alqutaibi AY and Algabri RS suggested that the risk of implant failure in patients with AgP is four times the failure in healthy patients. The study reported that the survival rate of the implants in individuals with AgP were compatible with those of healthy patients at (83.3-100% and 100%), respectively [10]. The need for conducting longitudinal research to investigate the reliability and efficiency of implantation in GAgP patients is highly required. Additionally, exploring a variety of successful treatment plans in dealing with such diseases is an essential step towards providing GAgP patients with a better quality of life.
Conclusion
This case report demonstrates that implant-retained denture might be a suitable option for young patients with GAgP since it requires two implants in each jaw to provide a fair amount of retention for the denture. This could be achievable given it is relatively cheap and can be utilised when massive bone loss has occurred compared to other treatment plans that involve full mouth implantation.
[1]. Armitage GC, Development of a classification system for periodontal diseases and conditionsAnnals of Periodontology 1999 4(1):1-6.10.1902/annals.1999.4.1.110863370 [Google Scholar] [CrossRef] [PubMed]
[2]. Demmer RT, Papapanou PN, Epidemiologic patterns of chronic and aggressive periodontitisPeriodontology 2000 2010 53:28-44.10.1111/j.1600-0757.2009.00326.x20403103 [Google Scholar] [CrossRef] [PubMed]
[3]. Wim T, Rutger D, Christel D, Marc Q, Treatment of aggressive periodontitisPeriodontology 2000 2014 65(1):107-33.10.1111/prd.1202024738589 [Google Scholar] [CrossRef] [PubMed]
[4]. Sadowsky SJ, The implant-supported prosthesis for the edentulous arch: design considerationsThe Journal of Prosthetic Dentistry 1997 78(1):28-33.10.1016/S0022-3913(97)70084-2 [Google Scholar] [CrossRef]
[5]. Haag D, Peres K, Balasubramanian M, Brennan D, Oral conditions and health-related quality of life: a systematic reviewJournal of Dental Research 2017 96(8):864-74.10.1177/002203451770973728581891 [Google Scholar] [CrossRef] [PubMed]
[6]. Llanos AH, Silva CGB, Ichimura KT, Rebeis ES, Giudicissi M, Romano MM, Impact of aggressive periodontitis and chronic periodontitis on oral health-related quality of lifeBrazilian Oral Research 2018 32:e00610.1590/1807-3107bor-2018.vol32.000629451591 [Google Scholar] [CrossRef] [PubMed]
[7]. MousaviJazi M, Naderan A, Ebrahimpoor M, Sadeghipoor M, Association between psychological stress and stimulation of inflammatory responses in periodontal diseaseJournal of dentistry (Tehran, Iran) 2013 10(1):103 [Google Scholar]
[8]. Misch CE, Prosthetic options in implant dentistryContemporary Implant Dentistry 2008 126 [Google Scholar]
[9]. Monje A, Alcoforado G, Padial-Molina M, Suarez F, Lin GH, Wang HL, Generalized aggressive periodontitis as a risk factor for dental implant failure: a systematic review and meta-analysisJournal of periodontology 2014 85(10):1398-407.10.1902/jop.2014.14013524835415 [Google Scholar] [CrossRef] [PubMed]
[10]. Alqutaibi AY, Algabri RS, Limited Evidence Suggests high risk of implant failure rates among people with generalized aggressive periodontitisThe journal of Evidence-Based Dental Practice 2015 15(4):187-89.10.1016/j.jebdp.2015.10.00626698006 [Google Scholar] [CrossRef] [PubMed]