Prostate Specific Antigen: A Diagnostic Marker in Polycystic Ovarian Syndrome
Kiran Bhat1, Meena Bhandari2, Vaishali Garg3
1 Associate Professor, Department of Biochemistry, Shri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun, Uttarakhand, India.
2 Student, Department of Biochemistry, Shri Mahant Indiresh Hospital, Dehradun, Uttarakhand, India.
3 Professor and Head, Department of Biochemistry, Sai Institute of Paramedical and Allied Sciences, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kiran Bhat, Department of Biochemistry, Shri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun-248001, Uttarakhand, India.
E-mail: kirsad@yahoo.co.in
Introduction
Polycystic Ovarian Syndrome (PCOS) is a common condition affecting females in the reproductive age group. Its diagnosis rests on clinical features like obesity, hirsutism, irregular menstrual flow, polycystic ovarian morphology on ultrasonography and laboratory investigations like serum estimation of Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), prolactin, dehydroepiandrosterone. The Prostate Specific Antigen (PSA) has been found to be raised in hyperandrogenic states and therefore can be used as a marker for diagnosis of PCOS.
Aim
The study was undertaken to evaluate serum PSA levels in patients of PCOS and its possible use in diagnosis of PCOS.
Materials and Methods
The case-control study included 40 women with PCOS and 40 age matched healthy women as controls. Serum PSA, LH, FSH and Prolactin levels were measured using immunometric technique. The data so obtained was statistically analysed using Student’s t-test. Pearson correlation was used to test the correlation between LH, FSH, Prolactin and total PSA (tPSA).
Results
Mean value of serum PSA was significantly higher in women with PCOS (0.03 ng/mL) as compared to control group (0.01 ng/mL). Serum PSA level of >0.01 ng/mL showed 100% sensitivity and specificity. Serum PSA levels had a positive correlation with serum LH levels (p-value 0.001) and serum prolactin levels (p-value 0.03). However, no correlation between PSA and FSH (p-value 0.042) was observed. LH/FSH ratio was raised in 32 out of 40 cases and reversed in remaining eight cases.
Conclusion
The serum PSA level with cut-off value >0.01 ng/mL can be used to detect hyperandrogenism in women and therefore can be used as a diagnostic marker for diagnosis of PCOS.
Follicle stimulating hormone, Hyperandrogenism, Luteinizing hormone, Obesity, Polycystic ovary
Introduction
PCOS is a common disorder amongst females of reproductive age group. It is diagnosed by clinical evaluation, laboratory studies and imaging modalities, the commonest of which is ultrasonography. The diagnosis cannot be made with a single criterion since multiple manifestations characterise the syndrome [1].
PSA is a single chain glycoprotein weighing 33 kDa. It is a serine protease with chymotrypsin like enzymatic activity [2]. It was initially thought to be present only in males, produced exclusively by the prostate gland and used as a marker for diseases of prostate gland especially prostatic carcinoma [3,4]. Introduction of more sensitive assays revealed its presence in females [5]. Initially, PSA was believed to be completely absent from all female tissues but now it has been shown to be produced by many normal tissues in females including breast, parotid gland, endometrial tissue and periurethral glands [6-8]. It is also produced by some tumours including breast, colonic, ovarian, adrenal and parotid tumours [9,10]. PSA levels increase in women with androgen excess. The presence of PSA in these female tissues seems to be associated with steroid hormone regulation especially androgens, progestins and glucocorticoids.
Elevated serum PSA in females with hyperandrogenism including those with PCOS, has become a subject of clinical interest with PSA being suggested as a marker of hyperandrogenic state. Androgens are thought to upregulate the PSA gene in certain tissues leading to increased production of PSA [11-14]. Since PCOS is the most common cause of hyperandrogenism in females, PSA has been suggested as a marker for the same [15]. PSA level is under the regulation of steroid hormones especially androgens and progestins. This relationship between PSA production and androgen regulation may be the marker of androgen action in women. The exact pathophysiology of PCOS is very complex and remains largely unknown. There are many suggested aetiologies for the development of PCOS but none have full experimental support. The underlying cause seems to be combination of increased androgens and effect of insulin resistance [16]. The present study was taken up to evaluate serum PSA levels in patients with PCOS to establish a cut-off value which would be useful in diagnosis of PCOS.
Materials and Methods
This case-control study conducted at Biochemistry Department of Central Laboratory, Shri Mahant Indiresh Hospital, Dehradun, Uttarakhand, India, from January 2017 to December 2017. The study was approved by the institutional ethics committee (Reg no. ECR/710/Institute/UK/2015 and vide letter no. SGRR/IEC/8/17). The patients with polycystic ovaries checked by ultrasound attending the Obstetrics and Gynaecology OPD for hirsutism, obesity and irregular menstrual flow were enrolled in the study group (n=40). Equal number of females of age-matched student and staff women with normal ovaries on ultrasound and regular menstrual cycle were recruited as controls. Both the PCOS and control subjects were in the age group of 18-45 years. Informed consent was obtained from all the participants under study. Women on steroids and those who were smokers were excluded from the study. Women with idiopathic hirsutism and androgen secreting adrenal and ovarian tumours were also excluded.
Overnight fasting early morning blood sample of three mL in yellow-top vacutainers was collected from each subject in early follicular phase (day 2-4 of menstrual cycle). The samples were processed within an hour of collection and serum Luteinizing Hormone (LH), Follicle Stimulating Hormone (FSH), prolactin and total PSA (tPSA) were measured.
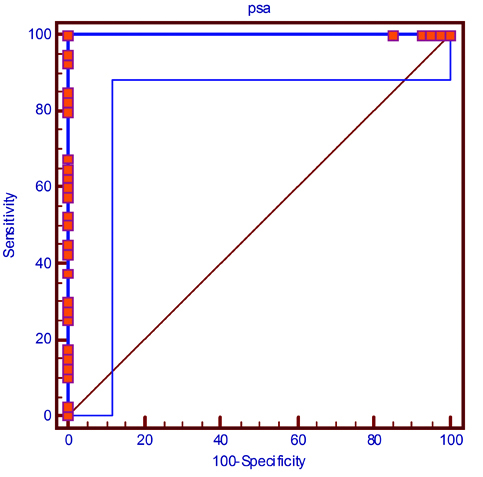
The blood samples were assayed by immunometric technique based on antigen antibody complex formation using Vitros 5600 fully automated analyser (Ortho Diagnostics). The data thus obtained was processed by Statistical Package for Social Science (SPSS) 21 version. The continuous variables were expressed as mean±SD. These means were compared using Student’s t-test. Pearson correlation was used to find the correlation between LH, FSH, Prolactin and tPSA. The p-value of <0.05 was considered statistically significant. ROC curve was plotted and used to determine the cut-off level of tPSA for diagnosis of PCOS. The sensitivity and specificity of the cut-off values was also calculated.
Results
The age of subjects in both control and cases groups ranged between 18 to 45 years. The mean age of study group was 28.5±6.15 years and the mean age of control group was 29.2±5.54 years which was comparable.
The serum tPSA level of women with PCOS was between 0.012-0.039 ng/mL with mean of 0.03 ng/mL. The serum tPSA levels in control group were ≤0.01 ng/mL. The serum tPSA levels were significantly elevated in study group as compared to the control group (p-value <0.001). Elevated levels of LH, FSH and prolactin were also observed in women with PCOS as compared to control group (p-value <0.0005; [Table/Fig-1]).
Serum levels of LH, FSH, Prolactin and tPSA in the PCOS cases and control group.
| Parameter | Mean±SD | t-value | p-value* |
|---|
| Study group (n=40) | Control group (n=40) |
|---|
| Serum LH (mIU/mL) | 18.51±14.45 | 6.32±3.48 | 5.1871 | <0.0001 |
| Serum FSH (mIU/mL) | 10.94±15.82 | 5.60±2.4 | 2.1101 | 0.038 |
| Serum Prolactin (mIU/L) | 347.48±154.78 | 250.33±68.14 | 3.6632 | 0.0005 |
| tPSA (ng/mL) | 0.030±.015 | 0.009±0.001 | 6.3246 | <0.0001 |
p-value is significant at p<0.05* FSH: Follicle stimulating hormone, LH: Luteinizing hormone, PCOS: Polycystic ovarian syndrome, tPSA: Total prostate specific antigen, mIU: Milli international units, ng: Nano gram, mL: Milli litre
In the study group LH: FSH ratio was elevated in 32 subjects and reversed in eight subjects. Positive predictive value is 100%, negative predictive value is 100% and area under the curve is 1.00 [Table/Fig-2]. Pearson correlation between tPSA and LH is 0.44 (p-value 0.001), between tPSA and FSH is 0.092 (p-value 0.42) and between tPSA and prolactin is 0.23 (p-value 0.03) [Table/Fig-3].
 |
| Youden index | 1.00 |
| Associated criterion | >0.01 |
| Sensitivity | 100% (91.2%-100%) |
| Specificity | 100% (91.2%-100%) |
Pearson correlation between PSA and other variables.
| Variable | Pearson correlation | p-value |
|---|
| LH | 0.44 | 0.001* |
| FSH | 0.092 | 0.42 |
| Prolactin | 0.23 | 0.03* |
*Significant at 95% CI (2 Tailed)
Discussion
PCOS was originally described by Stein and Leventhal in 1935 as a triad of amenorrhea, hirsutism, and obesity in women who had multiple cysts in their ovaries. PCOS also known as functional ovarian hyperandrogenism, is a complex disorder that begins during puberty and affects women in reproductive age group [17]. It is characterised by increased ovarian and adrenal androgen secretion [18]. PCOS is a combination of chronic anovulation or oligomenorrhea and biochemical or clinical hyperandrogenism and ovarian polycystic changes observed by ultrasound and affects 6-8% of the population [19,20]. Elevated levels of LH and subsequent influences on the thecal compartment of ovary may play an additional role in the establishment of clinically apparent hyperandrogenism.
In the present study PSA levels in patients of PCOS were between 0.012-0.039 ng/mL while in the control group the levels were below 0.01 ng/mL. These findings were similar to work of Vural B et al., which showed elevated PSA levels in patients of PCOS (0.026±0.023 ng/mL) as compared to controls (0.009±0.008 ng/mL) [21].
Mardanian F et al., also reported elevated PSA levels in the patients with PCOS. In their study cut-off levels of PSA for diagnosis of PCOS was established as 0.07 ng/mL with sensitivity of 91%, specificity of 81.2%, positive predictive value of 81% and negative predictive value of 85% [22]. Ukinc K et al., suggested a cut-off level of PSA of >10 pg/mL (0.01 ng/mL) for diagnosis of PCOS. They also evaluated the levels of free PSA (fPSA) in these patients and suggested a cut-off levels of fPSA of >2.1 pg/mL (0.0021 ng/mL) for the diagnosis of PCOS [23]. Diamandis PE et al., studied complexed and fPSA levels in women and concluded that both are raised threefold in women with PCOS [24].
Urinary PSA levels have been demonstrated to be higher in patients with PCOS. However if urine samples are taken following sexual intercourse the elevated levels can be because of seminal contamination. If this contamination can be excluded, urinary PSA can also serve as a marker for PCOS [25].
Certain important facts about PSA in females have been elucidated. Burelli A et al., showed raised serum PSA levels in patients of PCOS and noted that the PSA levels are not affected by the stage of menstrual cycle or menopause [26]. PSA levels were reported to be higher in pregnant women compared to non pregnant women. Thus PSA can serve as a better marker compared to hormones which show variation in various phases of menstruation. Melegos DN et al., found a negative correlation between PSA and age [15]. Flutamide which is an anti-androgen used for treatment of hyperandrogenism in women has been shown to decrease PSA levels [27].
We also studied the serum LH, FSH and prolactin levels. All of these were found to be significantly elevated in patients of PCOS as compared to control group. LH levels are increased in PCOS because of fast gonadotropin releasing hormone (GnRH) pulse, while as estrogen stimulates production of prolactin [28]. Persistently elevated estradiol levels are found in women with PCOS. In our study LH: FSH ratio was not found to be increased in all patients and was in fact lowered in eight patients. We therefore suggest LH: FSH ratio should not be considered as a parameter for the diagnosis of hyperandogenism. These findings could further be justified by the Rotterdam ESHRE/ASRM guidelines (2004), which state that the measurement of LH should not be considered necessary for clinical diagnosis of PCOS [1].
Large studies are required to establish the normal range in females and establishing the cut-off values for diagnosis of PCOS. However in association with other features of PCOS, serum PSA levels can be important marker of PCOS.
Conclusion
PSA levels were significantly increased in patients of PCOS. The cut-off level for PCOS was established to be higher than 0.012 ng/mL with sensitivity and specificity of 100% which can be used for the diagnosis of hyperandrogenism in women.
p-value is significant at p<0.05* FSH: Follicle stimulating hormone, LH: Luteinizing hormone, PCOS: Polycystic ovarian syndrome, tPSA: Total prostate specific antigen, mIU: Milli international units, ng: Nano gram, mL: Milli litre
*Significant at 95% CI (2 Tailed)
[1]. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS)Hum Reprod 2004 19(1):41-47.10.1093/humrep/deh09814688154 [Google Scholar] [CrossRef] [PubMed]
[2]. Hara M, Koyanagi Y, Inoue T, Fukuyama T, Some physicochemical characteristics of gamma-seminoprotein; an antigenic component specific for human seminal plasmaJpn J Legal Med 1971 25:322-24. [Google Scholar]
[3]. Wang MC, Valenzuela LA, Murphy GP, Chu TM, Purification of a human prostate specific antigenInvest Urol 1979 17(2):159-63.[PubMed: 89106] [Google Scholar]
[4]. Papsidero LD, Wang MC, Valenzuela LA, Murphy GP, Chu TM, A prostate antigen in sera of prostate cancer patientsCancer Res 1980 40:2428-33. [Google Scholar]
[5]. Diamandis EP, Yu H, New biological functions of prostate specific antigen?J Clin Endocrinol Metab 1995 80:1515-17.10.1210/jc.80.5.1515 [Google Scholar] [CrossRef]
[6]. Clements A, Mukhtar A, Glandular kallikreins and prostate specific antigen are expressed in the human endometriumJ Clin Endocrinol Metab 1994 78:1536-39.10.1210/jcem.78.6.75153927515392 [Google Scholar] [CrossRef] [PubMed]
[7]. Wemert N, Albrech M, Sesterhenn I, Goebbels R, Bonkoff H, Sietz G, The ‘female urostate.’ Location, morphology, immunohistochemical characteristics and significanceEur Urol 1992 22:64-69.10.1159/000474724 [Google Scholar] [CrossRef]
[8]. Yu H, Diamandis EP, Prostate specific antigen in milk of lactating womenClin Chem 1995 41:54-60. [Google Scholar]
[9]. Levesque M, Yu H, D’Costa M, Diamandis EP, Prostate specific antigen expression by various tumorsJ Clin Lab Anal 1995 9:123-28.10.1002/jcla.18600902097536238 [Google Scholar] [CrossRef] [PubMed]
[10]. Yu H, Diamandis EP, Sutherland DJA, Immunoreactive prostate specific antigen levels in female and male breast tumors and its association with steroid hormone receptors and patient ageClin Biochem 1994 27:75-79.10.1016/0009-9120(94)90015-9 [Google Scholar] [CrossRef]
[11]. Yu H, Diamandis EP, Zarghami N, Grass L, Induction of prostate specific antigen production by steroids and tamoxifen in breast cancer cell linesBreast Cancer Res Treat 1994 32:291-300.10.1007/BF00666006 [Google Scholar] [CrossRef]
[12]. Cleutjens KB, van der Korput HA, van Eekelen CC, van Rooij HC, Faber PW, Trapman J, An androgen response element in a far upstream enhancer region is essential for high, androgen-regulated activity of the prostate-specific antigen promoterMol Endocrinol 1997 11:148-61.10.1210/mend.11.2.98839013762 [Google Scholar] [CrossRef] [PubMed]
[13]. Cleutjens KB, van Eekelen CC, van der Korput HA, Brinkmann AO, Trapman J, Two androgen response regions cooperate in steroid hormone regulated activity of the prostate-specific antigen promoterJ Biol Chem 1996 271:6379-88.10.1074/jbc.271.11.63798626436 [Google Scholar] [CrossRef] [PubMed]
[14]. Yu H, Diamandis EP, Monne M, Croce CM, Oral contraceptive-induced expression of prostate-specific antigen in the female breastJ Biol Chem 1995 270:6615-18.[PubMed: 7534765]10.1074/jbc.270.12.66157534765 [Google Scholar] [CrossRef] [PubMed]
[15]. Melegos DN, Yu H, Ashok M, Wang C, Stanczyk F, Diamandis EP, Prostate-specific antigen in female serum, a potential new marker of androgen excessJ Clin Endocrinol Metab 1997 82(3):777-80.[PubMed: 9062481]10.1210/jcem.82.3.37929062481 [Google Scholar] [CrossRef] [PubMed]
[16]. Garad R, Teede H, Moran L, An evidence-based guideline for polycystic ovary syndromeAust Nurs J 2011 19(4):30-33. [Google Scholar]
[17]. Swetha N, Vyshnavi R, Modagan P, Rajagopalan B, A correlative study of biochemical parameters in polycystic ovarian syndromeInt J Biol Med Res 2013 4(2):3148-54. [Google Scholar]
[18]. Kalra A, Nair S, Rai L, Association of obesity and insulin resistance with dyslipidemia in Indian women with polycystic ovarian syndromeIndian J Med Sci 2006 60(11):447-53.10.4103/0019-5359.2797117090865 [Google Scholar] [CrossRef] [PubMed]
[19]. Diamanti-Kandarakis E, Polycystic ovarian syndrome: pathophysiology, molecular aspects and clinical implicationsExpert Rev Mol Med 2008 30:1010.1017/S146239940800059818230193 [Google Scholar] [CrossRef] [PubMed]
[20]. Rudnicka E, Radowicki S, Suchta K, Prostate specific antigen (PSA) in diagnosis of polycystic ovarian syndrome-a new insightGynecol Endocrinol 2016 32(11):931-35.10.1080/09513590.2016.120055227426018 [Google Scholar] [CrossRef] [PubMed]
[21]. Vural B, Ozkan S, Bodur H, Is prostate-specific antigen a potential new marker of androgen excess in polycystic ovary syndrome?J Obstet Gynaecol Res 2007 33(2):166-73.[PubMed: 17441890]10.1111/j.1447-0756.2007.00507.x17441890 [Google Scholar] [CrossRef] [PubMed]
[22]. Mardanian F, Heidari N, Diagnostic value of prostate specific antigen in women with polycystic ovary syndromeJournal of Research in Medical Sciences 2011 16(8):999-1005. [Google Scholar]
[23]. Ukinc K, Ersoz HO, Erem C, Hacihasanoglu AB, Diagnostic value of prostate-specific antigen (PSA) and free prostate specific antigen (fPSA) in women with ovulatory and anovulatory polycystic ovary syndromeEndocrine 2009 35(1):123-29.[PubMed: 19009369]10.1007/s12020-008-9130-619009369 [Google Scholar] [CrossRef] [PubMed]
[24]. Diamandis PE, Stanczyk FZ, Wheeler S, Mathew A, Stengelin M, Galina Nikolenko G, Serum complexed and free prostate specific antigen (PSA) for the diagnosis of the Polycystic Ovarian Syndrome (PCOS)Clin Chem Lab Med 2017 55(11):1789-97.10.1515/cclm-2016-112428361781 [Google Scholar] [CrossRef] [PubMed]
[25]. Obiezu CV, Scorilas A, Magklara A, Thornton MH, Wang CY, Stanczyk FZ, Prostate-specific antigen and human glandular kallikrein 2 are markedly elevated in urine of patients with polycystic ovary syndromeJ Clin Endocrinol Metab 2001 86:1558-61.[PubMed: 11297583]10.1210/jcem.86.4.737811297583 [Google Scholar] [CrossRef] [PubMed]
[26]. Burelli A, Rineladi E, Cionini R, Benelli E, Pinchera A, Pucci E, Serum levels of PSA do not change in healthy premenopausal and in menopausal women, but are increased in subjects with Polycystic Ovary Syndrome (PCOS)Endocrine Abstracts 2006 11:685 [Google Scholar]
[27]. Bahceci M, Bilge M, Tuzcu A, Tuzcu S, Bahceci S, Serum prostate specific antigen levels in women with polycystic ovary syndrome and the effect of flutamide+desogestrel/ethinyl estradiol combination. J Endocrinol Invest 2004 27:353-56.[PubMed: 15233555]10.1007/BF0335106115233555 [Google Scholar] [CrossRef] [PubMed]
[28]. Szosland K, Pawlowicz P, Lewiński A, Prolactin secretion in Polycystic Ovary Syndrome (PCOS)Neuro Endocrinol Lett 2015 36(1):53-58. [Google Scholar]