Split Hand/Foot Malformation: A Case Report and Review of Literature
Divya Chauhan1, Alpana Singh2
1 Senior Resident, Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Alpana Singh, Associate Professor, Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi-110095, India.
E-mail: dralpanasingh@gmail.com
Split Hand/Foot Malformation (SHFM) is a rare genetic disorder. It is also known as ectrodactyly. In this disorder, the central rays of the hand and feet are affected leading to various malformations of the hands and feet. Any number of limbs can be affected. It can present in isolation affecting only the limbs or it can be associated with the syndrome. The prevalence of this malformation is 0.06 per 1000 total births. Here, authors report a case in which a pregnant patient had SHFM and the fetus also suffered the same anomaly. The anomaly was detected on ultrasound and medical termination of pregnancy was done.
Congenital, Ectrodactyly, Fetus
Case Report
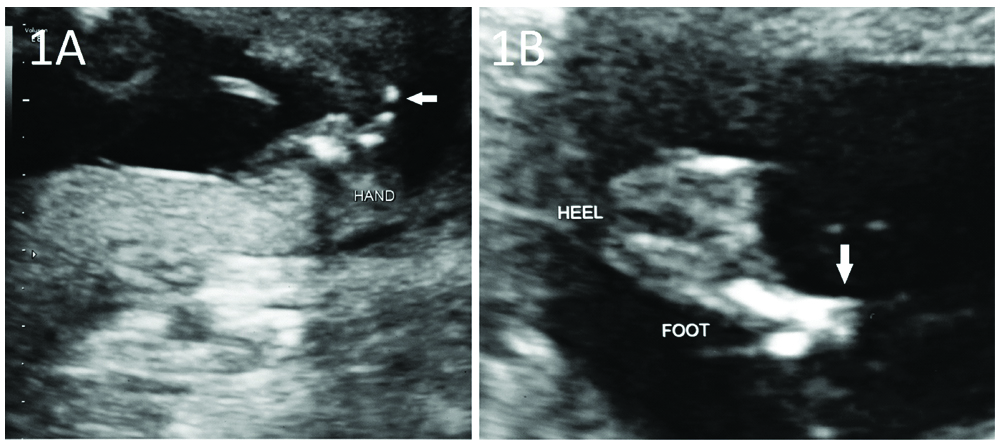
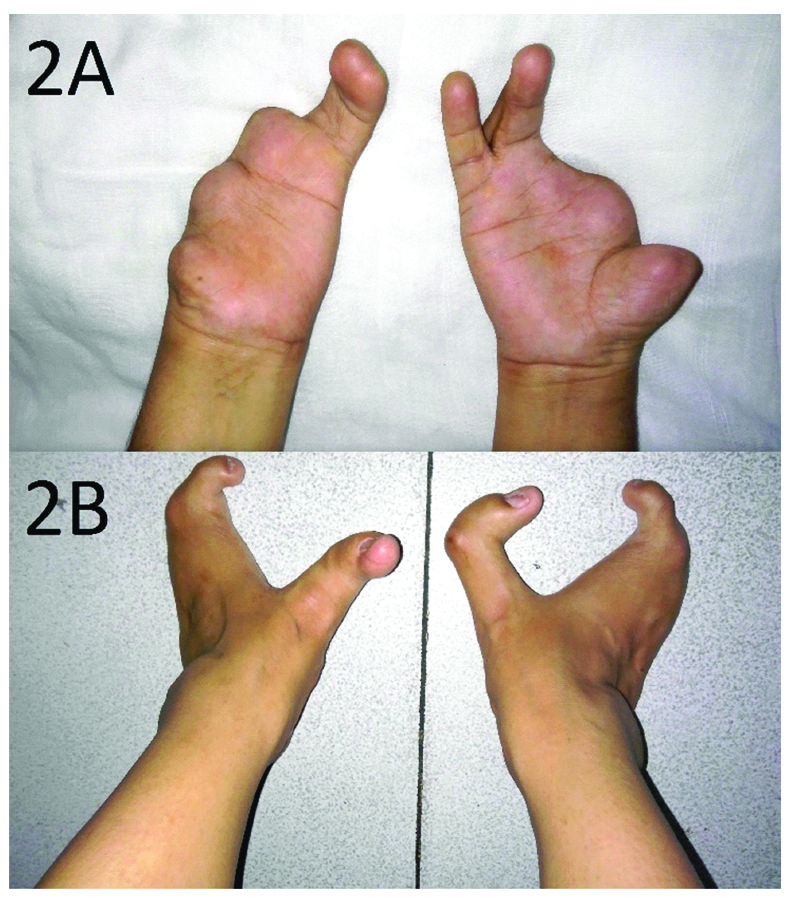
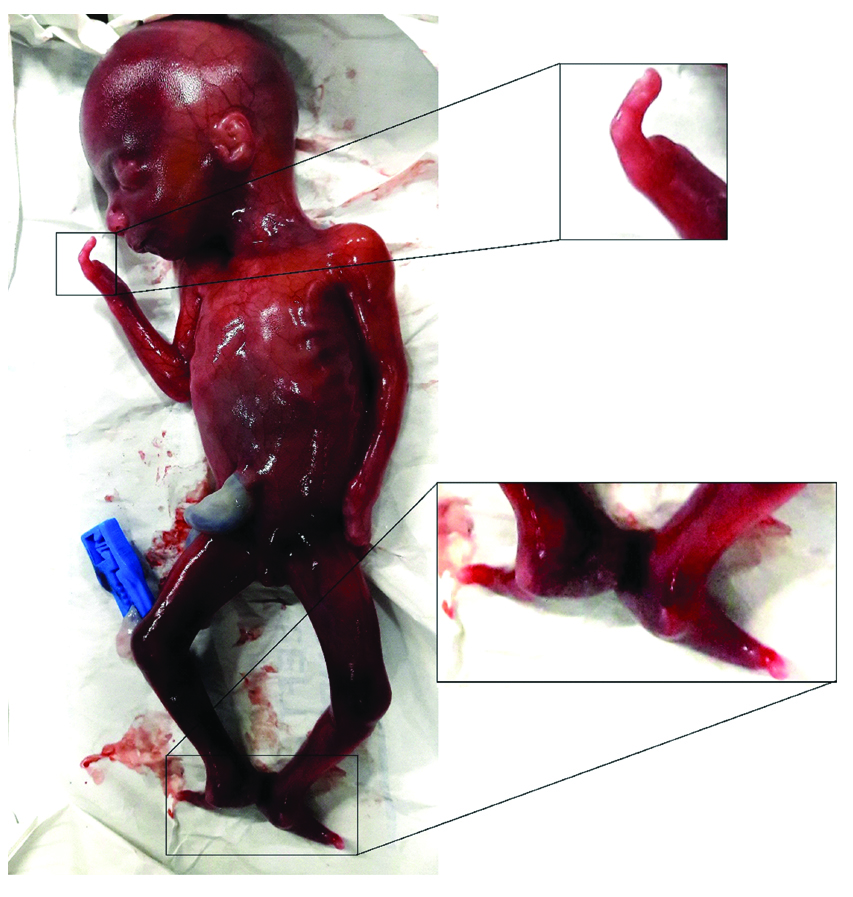
A 27-year-old primigravida at 19-weeks of gestation came to gynaecology outpatient department of our hospital with an obstetric ultrasound showing presence of only one digit in the hands and feet of the fetus [Table/Fig-1a,b]. She had no exposure to any teratogenic drugs during the antenatal period. She also had congenital deformities in her limbs-absent first, second and third digits and syndactyly of fourth and fifth digits in the left hand and under-developed first digit and absent second and third digits in right hand. Both her feet had median cleft [Table/Fig-2(a,b)]. No other anomalies, which are commonly associated with the syndrome such as cleft lip/palate, hearing loss, mental retardation and eye, nasal, heart or urogenital defects, were present. There was no history of consanguineous marriage. Her husband was normal. Besides her sister, there were no other family members who suffered from the same deformity including her parents and grandparents. She wanted medical termination of pregnancy in view of the physical abnormalities in the fetus. The abortus was having similar malformations, with hands and feet as shown in [Table/Fig-3].
(a) Antenatal ultrasonograph showing single digit in hand of fetus (horizontal arrow). (b) Antenatal ultrasonograph showing single digit in foot of fetus (vertical arrow).
Upper and lower limbs of the patient showing: a) Left hand with absent first, second and third digits and syndactyly of fourth and fifth digits and right hand with under-developed first digit and absent second and third digits. b) Left and right feet with median cleft.
Abortus with single digit in both hands and feet.
Discussion
SHFM is a congenital limb malformation affecting the central rays of the hand and/or foot. Any number of limbs can be affected. It is also known as ectrodactyly, giving “lobster claw” appearance [1]. The prevalence of this malformation is 0.06 per 1000 total births [2]. Sporadic SHFM is more common than familial form. Autosomal dominant inheritance is most common with variable expressivity. Seven chromosomal loci are associated with isolated SHFM. They are SHFM 1 to 6 and SHFM/SHFLD. The autosomal dominant mode of inheritance is associated with SHFM1, SHFM3, SHFM4 and SHFM5. Autosomal recessive and X-linked inheritance is rarely seen [3].
Mutations in 7q21.3-q22.1 chromosomal region cause Type 1 SHFM, inherited in an autosomal dominant fashion with variable expression. SHFM Type 1 can be either associated with isolated limb malformation or with the syndrome. About 35% of these patients have associated sensorineural hearing loss. SHFM2 locus has been mapped to Xq26. The locus for SHFM3 maps to chromosome 10 q24 and the causative rearrangement involves a submicroscopic tandem duplication spanning a region of 325-570 kb. Duplications of the SHFM3 locus are the most frequent cause of SHFM in human beings and accounts for approximately 20% of cases. SHFM4 locus maps to 3q27 region and is associated with TP63 gene mutations. Chromosome 2q31 region deletions encompassing the HOXD gene cluster have been linked with SHFM5. Homozygous mutations in WNT10B, a gene located within the SHFM6 locus causes autosomal recessive SHFM [3].
The developing limb bud consists of mesenchymal cells covered by ectodermal cells. Three specialised cell groups produce signalling molecules which mediate the formation of limb bud. These cell groups include the Apical Ectodermal Ridge (AER), the Progress Zone (PZ) and the Zone of Polarizing Activity (ZPA). These three cell groups interact to determine the pattern of limb development in proximo-distal, anteroposterior and dorso-ventral dimensions. Various signalling molecules and transcription factors produced by AER cause proliferation of mesenchymal cells, giving rise to PZ. Constant proliferation of cells of PZ determines the polarity of limb bud in the proximo-distal dimension. Thus, failure in maintaining the AER ultimately leads to the development of SHFM. Any environmental factors that affect the AER can also cause SHFM [3].
SHFM has varied clinical presentations. Clinical variability is not only seen between patients, but also between limbs of a single patient. It may present with median clefts of the hands and feet, syndactyly, aplasia and/or hypoplasia of phalanges, metacarpals and metatarsals. In severe cases of SHFM, the hands and feet have lobster claw-like appearance [4].
Ectrodactyly occurs either as an isolated malformation or may co-exist with other congenital anomalies. It has been shown to be associated with cleft lip or cleft palate, ectodermal dysplasia or developmental delay. In addition, it also occurs as a part of various syndromes such as EEC syndrome (ectrodactyly-ectodermal dysplasia-cleft lip/palate syndrome), EEC syndrome without cleft lip/palate, LADD syndrome (lacrimo-auriculo-dento-digital syndrome), ADULT syndrome (acro-dermato-ungual-lacrimal-tooth syndrome), CHARGE syndrome (coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth and/or development, genital and/or urinary abnormalities, and ear abnormalities and deafness) or VACTERL syndrome (vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities) [3].
Another case of a 26-year-old healthy pregnant woman was reported where antenatal ultrasonography at 22 weeks period of gestation detected V-shaped cleft in both feet of the fetus. Her first child also had median cleft in both feet [6]. A similar co-existence of SHFM in siblings has been reported by Ashi M et al., [7]. Lévy J et al., reported a case of triplet pregnancy in a 31-year-old healthy primigravida where one fetus was detected to have ectrodactyly and radial agenesis on ultrasonography at 10 weeks’ gestation. The abnormal fetus was selected for fetal reduction [8].
A retrospective review of sonographic studies was done at two fetal care centres in United States of America and China from 2002 to 2012. Ten pregnant women were identified with ultrasonography showing abnormalities in the fetus consistent with SHFM. The gestational age of the fetuses ranged from 15 to 29 weeks. Seven pregnancies were electively terminated due to the malformations, whereas three women had delivery at term [9].
A number of genetic tests are available these days, which can be used to predict the possible outcomes of a current or future pregnancy. Prenatal diagnosis can be made by performing antenatal ultrasonography. Accordingly, the decision to continue or terminate the pregnancy can be made.
Pre-Implantation Genetic Diagnosis (PGD) is an alternative to prenatal diagnosis. Only embryos that do not carry the disease-causing mutation are chosen for implantation. In most of the cases, the disease-causing mutation must be identified in an affected relative before PGD can be performed.
Till date, no appropriate non-surgical treatment is available for split hand foot malformation. Prostheses can be used for cosmetic purposes. The surgical management must be individualised. Primary goal of surgery should be good pinch and grasp, with cosmetic appearance being secondary. Surgical team should guide the parents and patient regarding the surgical options, timing and sequence of surgery [10].
Conclusion
Split Hand/Foot Malformation (SHFM) encompasses a wide variety of malformations of the hands and feet. Any number of limbs can be affected. It can also be associated with other syndromes. Antenatally, it can be diagnosed on ultrasonography. Detailed examination of hands and feet of the fetus on ultrasonography should be done, especially when the mother herself is suffering from the disorder or there is a family history of this malformation. If diagnosed early, medical termination of pregnancy can help in preventing the birth of babies afflicted with such debilitating malformation. When this anomaly is detected, prenatal counselling should be offered and genetic screening should be performed for all couples for present and possible future pregnancies. The disease-causing mutation must be identified in an affected relative. Pre-implantation genetic diagnosis should be offered so that only embryos that do not carry the disease-causing mutation are chosen for implantation.
[1]. Temtamy SA, McKusick VA, The genetics of hand malformationsBirth Defects 1978 14:53-71. [Google Scholar]
[2]. Czeizel A, Vitez M, Kodaj I, Lenz W, Birth prevalence of different congenital limb deficiency types in a population based revised Hungarian material 1975-1984Acta Morphol Hung 1991 39:229-37. [Google Scholar]
[3]. Sowinska-Seidler A, Socha M, Jamsheer A, Split-hand/foot malformation-molecular cause and implications in genetic counselingJ Appl Genet 2014 55:105-15.10.1007/s13353-013-0178-5 [Google Scholar] [CrossRef]
[4]. Duijf PH, van Bokhoven H, Brunner HG, Pathogenesis of split-hand/split foot malformationHum Mol Genet 2003 12:R51-R60.10.1093/hmg/ddg09012668597 [Google Scholar] [CrossRef] [PubMed]
[5]. Lapaire O, Schiesser M, Peukert R, Holzgreve W, Tercanli S, Split hand and foot malformation: ultrasound detection in the first trimesterUltrasound Obstet Gynecol 2002 20:511-12.10.1046/j.1469-0705.2002.00827.x12423492 [Google Scholar] [CrossRef] [PubMed]
[6]. Durmaz MS, Demirtaç H, Hattapoğlu S, Kara T, Göya C, Adin ME, Bilateral cleft foot: Radiographic and prenatal ultrasound features of two siblings with a review of literatureMedicina (Kaunas) 2016 52:257-61.10.1016/j.medici.2016.07.00327515833 [Google Scholar] [CrossRef] [PubMed]
[7]. Ashi M, Assur R, Awan B, Aljaaly H, Bilateral split hand foot malformation in siblings: Case seriesInt J Surg Case Rep 2018 44:114-17.10.1016/j.ijscr.2017.12.03029499514 [Google Scholar] [CrossRef] [PubMed]
[8]. Lévy J, Jouannic JM, Saada J, Dhombres F, Siffroi JP, Portnoï MF, Prenatal diagnosis of bilateral ectrodactyly and radial agenesis associated with trisomy 10 mosaicismCase Rep Genet 2013 2013:59270210.1155/2013/59270223401811 [Google Scholar] [CrossRef] [PubMed]
[9]. Lu J, Vaidya N, Meng H, Dai Q, Romine LE, Jones MC, Prenatally diagnosed fetal split-hand/foot malformations often accompany a spectrum of anomaliesJ Ultrasound Med 2014 33:167-76.10.7863/ultra.33.1.16724371113 [Google Scholar] [CrossRef] [PubMed]
[10]. Canale: Campbell’s Operative Orthopaedics 2003 10th edPhiladelphia, PAMosby, Inc [Google Scholar]