The normal male urethra is anatomically divided into prostatic and membranous portions forming the PU and bulbous and penile segments forming the AU. Anomalous obstructing developmental membranes formed by mucosal folds in the distal prostatic urethra are referred to as PUV. A cause of congenital infravesical obstruction in male neonates with an estimated incidence of 1 in 5000 to 8000 live male births, PUV leads to bladder dysfunction forming the commonest cause of chronic renal disease in a significant portion of boys [1,2]. Earliest described in 1515 on autopsy, the first clinical case was reported by Young HH etal., in 1913 [3]. Still, over 100 years later, more than a third of affected children develop renal failure due to under detection and delayed diagnosis [4]. Presentation is either with obstructive symptoms, more prevalent among neonates and infants or with features of Urinary Tract Infection (UTI), more frequent in older children [4,5]. The current reference standard for diagnosis and management being cystoscopy is expensive and invasive requiring specialised equipment, hospitalisation and general anaesthesia [6,7]. A cost effective technique for early detection could dramatically reduce morbidity and mortality.
Our aim was to evaluate cystourethrogram (VCUG) as a diagnostic modality and predictor of PUV, subsequently confirmed on cystoscopy. To assess this, ratios of posterior to anterior urethra (urethral ratio) were measured and the degree to which these ratios corresponded to the diagnosis of PUV as seen on cystoscopy were validated. The study also aimed to derive age-stratified normative ratios of PU to AU in the paediatric population.
Materials and Methods
The study was approved by the institutional review board and ethics committee of the hospital and undertaken prospectively over an 18 month period from March 2009 to September 2010. Participant selection was from a consecutive series within the time frame and independent of VCUG or cystoscopy. The principal investigator was blinded to cystoscopy findings.
The study included male children up to 15 years presenting with either UTI or significant symptoms who underwent VCUG and subsequently cystoscopy. Decision for cystoscopy was based on significant post void residual urine, abnormal urethral appearance on VCUG and relevant clinical data. (UTI definition: urine microscopy of >10 WBCs per high power field and/or urine culture showing bacterial growth more than 105 colony-forming units per mL of urine collected by an appropriate method. Significant symptoms included poor urinary stream, reduced urinary output, bedwetting, urinary dribbling, haematuria, urinary retention, poor urinary stream, abdominal distension, elevated serum creatinine, fever, antenatally detected hydronephrosis and vesicoureteric reflux).
The study excluded children undergoing repeated VCUG as a part of follow-up for treated PUV or those with other conditions requiring VCUG.
According to current practice in the institution, patients initially underwent urine microscopy and culture followed by VCUG and USG. If VCUG suggested PUV, further evaluation with cystoscopy was done within an approximate interval of two weeks between the VCUG and cystoscopy.
Index Test: Voiding Cystourethrogram (VCUG)
VCUG was performed after UTI (if present) had resolved and done in the fluoroscopy unit of the radiology department. The procedure was explained to the patient and/or parents, and informed consent obtained.
With the patient supine on the fluoroscopy table, catheterization using a number 5F infant feeding tube in very small children and number 8F or 10F infant feeding tube in older children was performed, after lubricating the catheter tip with anaesthetic jelly. Contrast volume to be instilled was calculated using
Koff’s formula: (age in years+2)×30 mL.
Diluted contrast (Diatrizoate meglumine 76% solution, 370 mg/mL of iodine) was instilled into the bladder with a syringe with intermittent fluoroscopic screening to document presence of vesicoureteric reflux, diverticula or other abnormalities. A distended bladder was determined by signs of discomfort or peri-catheter leak. An image of the distended bladder in antero-posterior projection was taken. Following catheter removal, images of the bladder in steep oblique views were obtained demonstrating both vesicoureteric junctions. During voiding phase, oblique views delineating the entire urethra was taken. At the end of voiding, a full-frontal film of the abdomen including kidney regions, was obtained and amount of post-void residual urine noted. Images were reviewed by a radiologist as usual and subsequently by the principal investigator.
VCUG was considered positive for presence of PUV in case of abnormal narrowing at the posterior and anterior urethral junction with proximal dilatation and narrowing distal to obstruction or if a persistent linear lucent defect was observed either associated with or in the absence of posterior urethral dilatation. All measurements were made on the same image. Additional findings associated with infravesical obstruction were documented.
Measurements
Points of measurement of posterior and anterior urethra:
Posterior Urethral Diameter (PU) was measured at the midpoint of the posterior urethra (halfway between the bladder neck and membranous urethra), in [Table/Fig-1a].
Diagrammatic representation of measurement technique of posterior and anterior urethral diameters to calculate urethral ratio. a=point of measurement of posterior urethral diameter. b=point of measurement of proximal bulbar urethera. c=point of measurement of distal bulbar urethra.
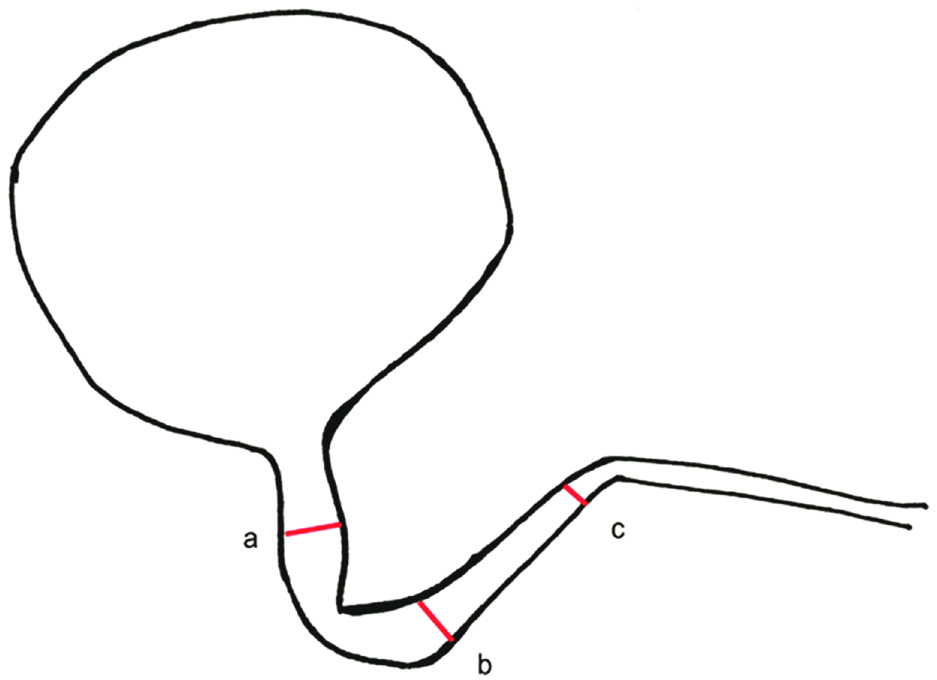
Anterior urethral diameter (AU) was assessed at two points in the horizontal segment of the bulbar urethra i.e. proximal (AU proximal bulbar) and distal (AU distal bulbar), in [Table/Fig-1b,c] respectively. {The bulbar urethral segment was chosen to represent the anterior urethra because this segment remains fixed, unlike the penile urethra which can have variable distension}. Measurement was taken at two points in order to obtain a more accurate estimate due to varying diameter along this segment depending on the amount of distension.
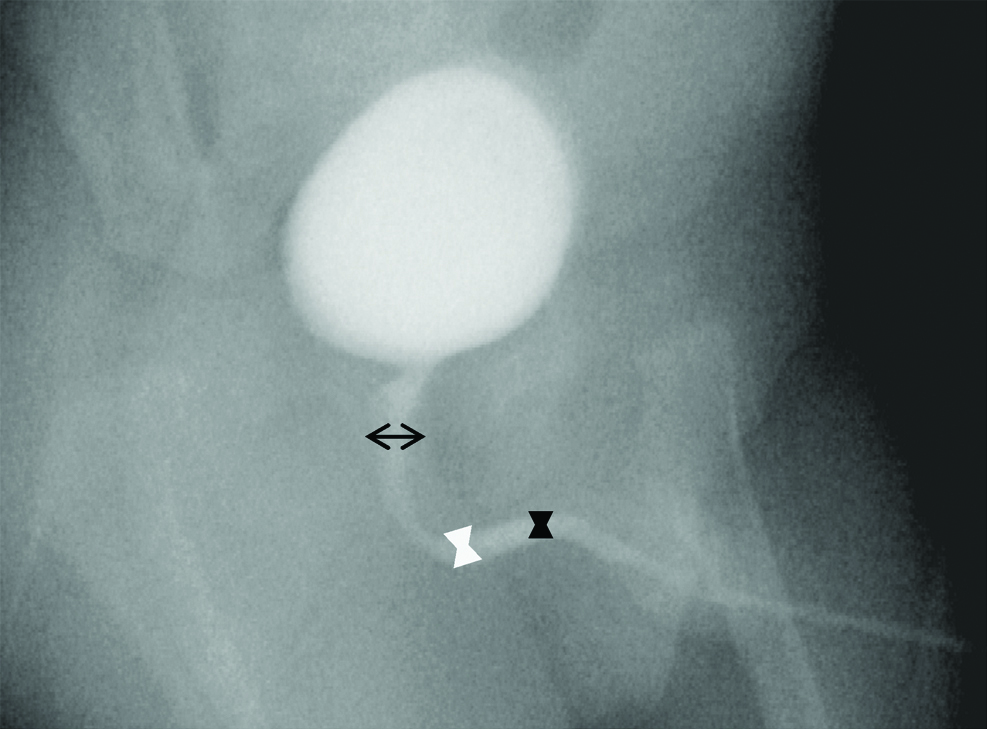
Voiding cystourethrogram in a normal male child with measurement points to demonstrate measurement technique (black arrow=a, white bowtie=b, black bowtie=c)
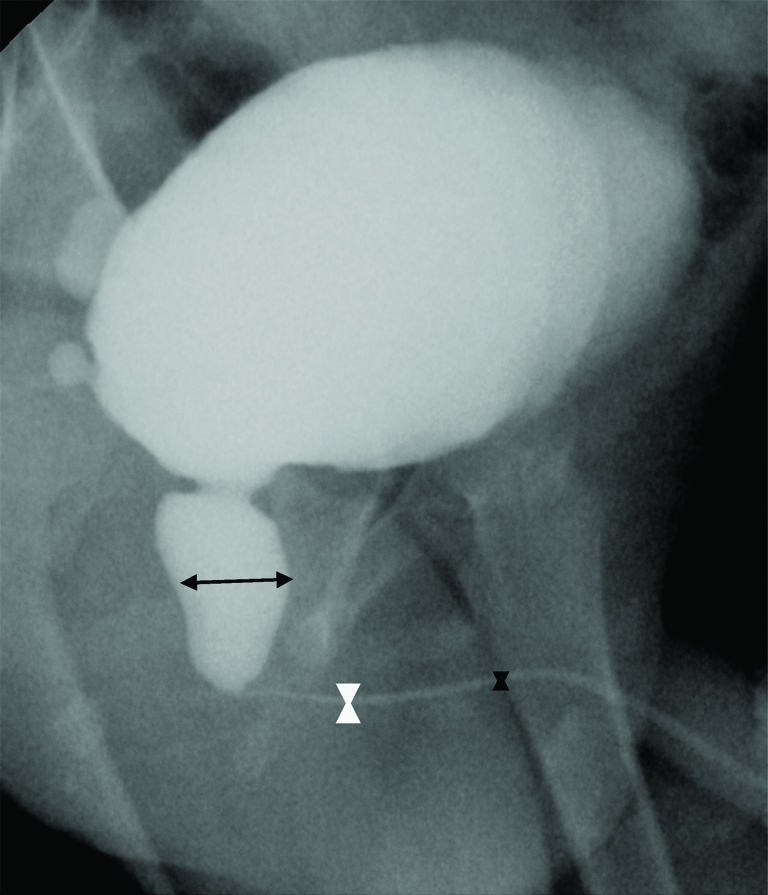
Voiding cystourethrogram in a male child with posterior urethral valves demonstrating measurement technique (black arrow=a, white bowtie=b, black bowtie=c)
Average of the two (AU proximal segment and AU distal segment) was obtained.
The ratio of posterior urethra to anterior urethra was subsequently calculated for all the three measurements i.e., (i) PU/AU proximal bulbar; (ii) PU/AU distal bulbar; (iii) PU/AU average of proximal and distal bulbar urethra.
Reference Standard: Cystoscopy
Cystoscopy was done in the department of paediatric surgery and performed on patients with significant post void residual urine and/or abnormal urethral appearance on VCUG or relevant clinical data. This was performed under general anaesthesia by an experienced paediatric surgeon. With the patient supine, a 7.5F cystoscope was inserted per urethra. Presence of posterior urethral valves was confirmed by identifying abnormal mucosal valves at the posterior and anterior urethral junction.
The VCUG was interpreted prior to and independent of cystoscopy; the principal investigator being blinded to cystoscopy findings. Decision to perform cystoscopy was based on interpretation of VCUG as well as relevant clinical data.
Data Entry and Statistical Analysis
Relevant data was tabulated and descriptive statistical methods used to summarise baseline data. Sensitivity, specificity, positive predictive value and negative predictive values were calculated.
Diagnostic accuracy of the ratios was calculated using ROC, best cut-off values and corresponding estimates of sensitivity and specificity determined. The area under the ROC curve (AUC) was used as a measure of diagnostic ability of ratios.
Results
In the present study population of 493 patients, 80 had an appearance of PUV on VCUG, among which confirmatory cystoscopy was performed in 55. Review of records of the 25 patients in whom cystoscopy was not performed showed-equivocal VCUG findings in 16 cases, hence patients were advised regular follow-up with cystoscopy planned if symptoms recurred, five were cases of neurogenic bladder and four had obvious features of PUV. Of these four, one underwent bilateral percutaneous nephrostomy and one underwent bilateral ureterostomy and did not undergo cystoscopy during the period of this study. The remaining two patients with obvious features of PUV did not undergo further treatment at the institution with no further documentation in the records. These were considered lost to follow-up cases.
A total of 100 patients underwent cystoscopy; these also included patients with clinical suspicion of PUV. At cystoscopy 49 patients were found to have a PUV. On VCUG the presence of a PUV was confirmed in 48 of these patients giving a sensitivity of 97.96% (48/49) and a specificity of 86.27% (44/51). In 87.27% (48/55), the VCUG was able to predict the presence of a PUV and in 97.78% it was able to exclude a PUV [Table/Fig-2].
Two-way contingency table showing the comparison between the presence and absence of posterior urethral valve as assessed by VCUG vs cystoscopy.
| PUV | Cystoscopy | Total |
|---|
| Valve present | Valve absent |
|---|
| VCUG | Valve present | 48 | 7 | 55 |
| Valve absent | 1 | 44 | 45 |
| Total | 49 | 51 | 100 |
Thus we found VCUG to be a reliable imaging modality in the assessment of PUV.
The mean and standard deviation of PU/AU ratio in patients with cystoscopically proven PUV, were calculated as shown in [Table/Fig-3].
The mean and standard deviation of PU/AU ratio in patients with posterior urethral valve.
| PU/proximal AU (a/b) | PU/distal AU (a/c) | PU/avg AU (a/(b+c/2)) |
|---|
| Mean | 5.151 | 5.546 | 5.366 |
| SD | 3.908447 | 3.881118 | 3.922125 |
The relevance of each of these ratios was further tested using ROC curves to determine which of the three had most clinical significance. Diagnostic accuracy of the three sets of ratios was calculated using ROC curves that displayed relationship between sensitivity (true-positive rate) and 1-specificity (false-positive rate) across all possible threshold values that could define the presence of PUV. Calculation was made on a sample size of 354 which included: (i) all patients with PUV confirmed on cystoscopy; (ii) all those with normal urethra as confirmed on cystoscopy; and (iii) all VCUGs that showed a normal urethra with no other associated or unrelated findings.
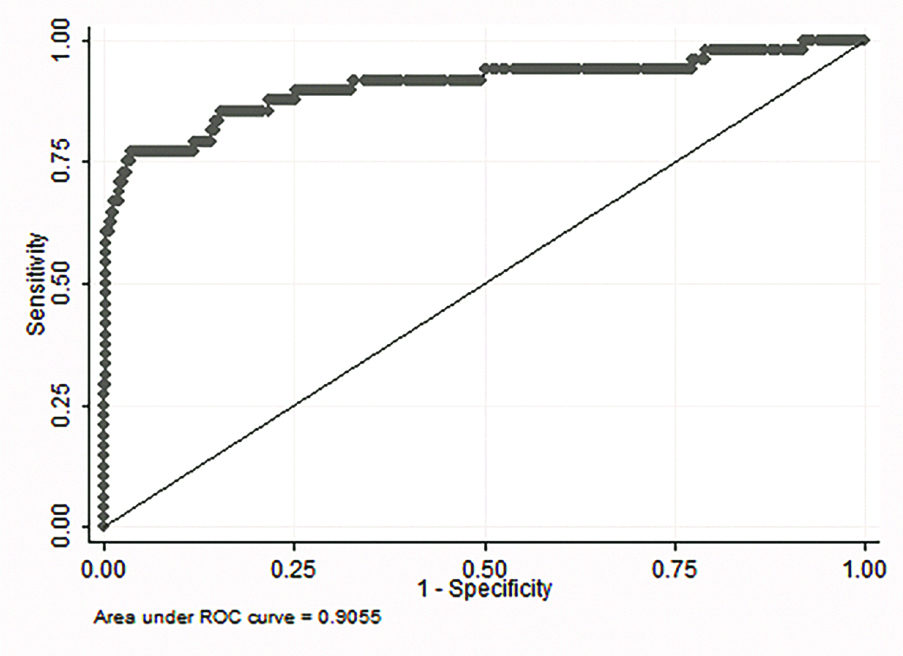
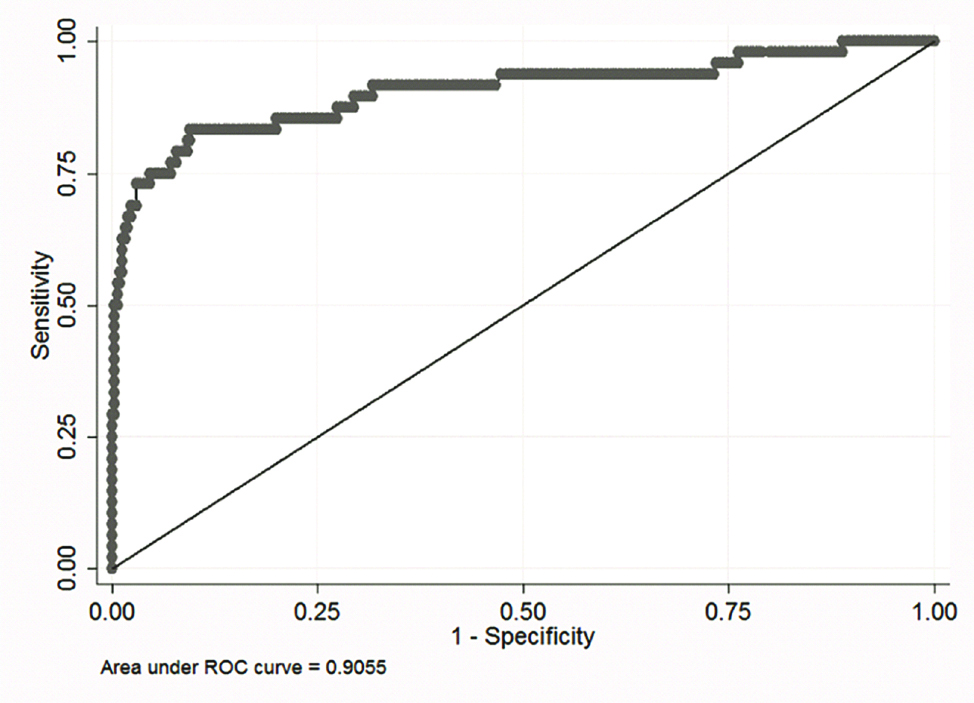
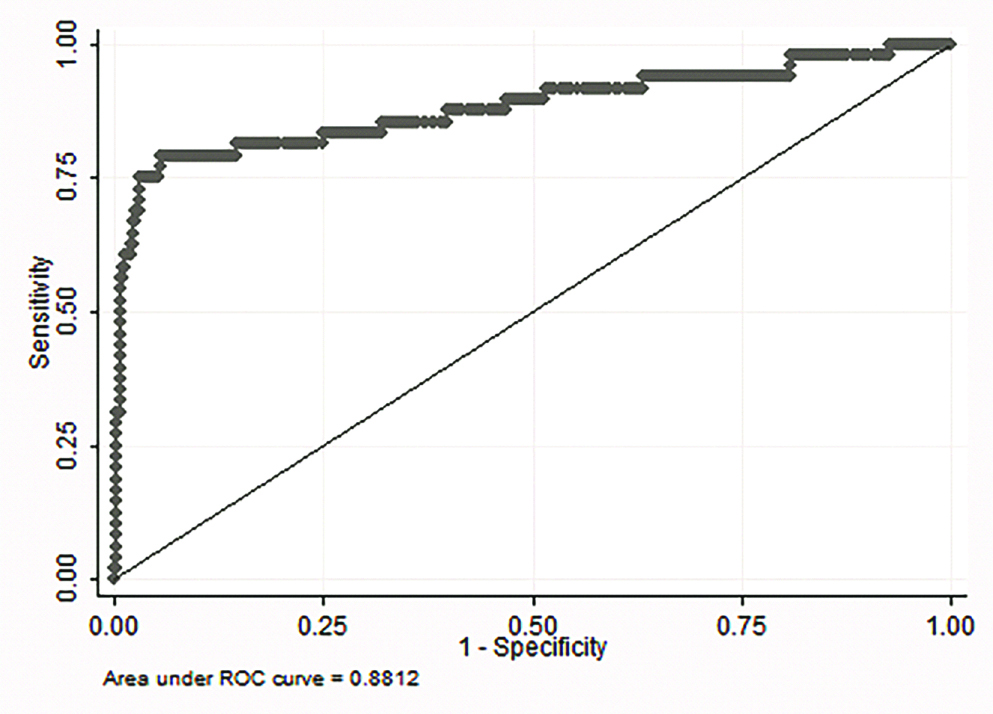
Calculated AUC was found to be significant for all three ratios and was most significant for ratio of posterior urethra to average of proximal and distal segments of the anterior urethra i.e., PU/avg AU [Table/Fig-4a,b and c].
ROC curve derived from ratio PU/average AU.
ROC curve derived from ratio PU/proximal AU.
ROC curve derived from ratio PU/distal AU.
The threshold values for the best combination of sensitivity and specificity for each of the PU/AU ratios is shown in [Table/Fig-5].
Threshold values of each calculated PU/AU ratio with best corresponding sensitivity and specificity.
| Threshold value | Sensitivity | Specificity |
|---|
| PU/AU average | ≥2.11 | 83% | 91% |
| PU/AU distal | ≥2.30 | 81% | 81% |
| PU/AU proximal | ≥2.02 | 85% | 85% |
Of the 3 ratios, PU/avg AU had the best combination of sensitivity and specificity, at a threshold ratio of ≥2.11 suggesting that at a ratio ≥2.11 the patient most likely has a PUV with an 83% sensitivity and 91% specificity.
The mean ratio in all true positive cases of PUV was 5.15 (SD±3.90) for PU/AU proximal portion, 5.54 (SD±3.88) for PU/AU distal and 5.36 (SD±3.92) for PU/average of AU. The relevance of these ratios were further tested using ROC curves to individually test the diagnostic accuracy of each and the most significant was found to be the ratio of PU/average of proximal and distal segments of the anterior urethra (AUC of 0.905, standard error 0.030, 95% Confidence Interval 0.84-0.96).
From the ROC curve we derived threshold values for each set of ratios that had the corresponding highest sensitivity and specificity. We found threshold values of ≥2.11 (sensitivity 83%, specificity 91%) for PU/average of AU, ≥2.30 (sensitivity and specificity of 81%) for PU/distal AU and ≥2.02 (sensitivity and specificity of 85%) for PU/proximal AU. Therefore, we concluded the most useful ratio in determining the presence or absence of a PUV on VCUG to be ratio between the posterior urethral diameter and the average of the proximal and distal bulbar urethral diameter (PU/ average AU ≥2.11).
The second part of the present study constituted calculation of normal PU/AU ratios. To the best of our knowledge this is a finding that has not been described till date. To obtain a range for normal PU/AU ratio, the average of ratios of posterior urethra to anterior urethra was calculated from the 3 different measurement points taken for the anterior urethra as described above on a total of 305 patients-all patients with negative appearance of PUV on VCUG. Mean, standard deviation and percentiles of normative ratios was calculated for each age from birth to 15 years in yearly intervals as shown in [Table/Fig-6,7 and 8], and again in stratified age groups for each set of ratios in [Table/Fig-9,10,11a and 11b].
Normative ratio for PU/AU proximal segment.
| Age | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| <1 | 65 | 1.57 | 0.68 | 0.77 | 0.93 | 1.07 | 1.39 | 1.88 | 2.48 | 2.99 |
| 1-2 | 47 | 1.50 | 0.58 | 0.96 | 0.97 | 1.15 | 1.42 | 1.57 | 2.16 | 2.50 |
| 2-3 | 24 | 1.48 | 0.79 | 0.90 | 0.91 | 0.97 | 1.35 | 1.63 | 2.09 | 2.40 |
| 3-4 | 21 | 1.17 | 0.30 | 0.80 | 0.82 | 0.97 | 1.13 | 1.27 | 1.44 | 1.88 |
| 4-5 | 12 | 1.40 | 0.52 | 0.57 | 0.88 | 1.04 | 1.36 | 1.69 | 1.94 | 2.48 |
| 5-6 | 17 | 1.54 | 0.66 | 0.75 | 0.90 | 1.05 | 1.33 | 1.96 | 2.63 | 3.01 |
| 6-7 | 16 | 1.27 | 0.45 | 0.52 | 0.66 | 1.04 | 1.24 | 1.46 | 1.83 | 2.43 |
| 7-8 | 18 | 1.51 | 0.60 | 0.74 | 0.93 | 1.12 | 1.37 | 1.68 | 2.40 | 3.21 |
| 8-9 | 13 | 1.13 | 0.38 | 0.60 | 0.77 | 0.95 | 1.12 | 1.29 | 1.44 | 2.09 |
| 9-10 | 13 | 1.53 | 0.54 | 0.84 | 1.01 | 1.23 | 1.52 | 1.67 | 1.87 | 3.04 |
| 10-11 | 11 | 1.22 | 0.40 | 0.74 | 0.90 | 0.92 | 1.16 | 1.60 | 1.69 | 2.06 |
| 11-12 | 12 | 1.21 | 0.39 | 0.73 | 0.87 | 0.93 | 1.15 | 1.46 | 1.51 | 2.17 |
| 12-13 | 11 | 1.04 | 0.34 | 0.65 | 0.69 | 0.71 | 1.02 | 1.15 | 1.26 | 1.86 |
| 13-14 | 15 | 1.15 | 0.29 | 0.62 | 0.72 | 0.94 | 1.12 | 1.33 | 1.51 | 1.72 |
| 14-15 | 10 | 0.95 | 0.26 | 0.57 | 0.61 | 0.79 | 0.90 | 1.14 | 1.33 | 1.43 |
| Total | 305 | 1.39 | 0.58 | 0.72 | 0.88 | 1.01 | 1.25 | 1.58 | 2.09 | 2.48 |
Normative ratio for PU/AU distal segment.
| Age | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| <1 | 65 | 1.99 | 1.27 | 1.14 | 1.31 | 1.43 | 1.83 | 2.06 | 2.76 | 2.88 |
| 1-2 | 47 | 1.97 | 0.60 | 1.07 | 1.25 | 1.50 | 1.86 | 2.37 | 2.90 | 3.00 |
| 2-3 | 24 | 1.77 | 0.48 | 1.28 | 1.34 | 1.42 | 1.70 | 2.00 | 2.35 | 2.91 |
| 3-4 | 21 | 1.64 | 0.43 | 1.00 | 1.03 | 1.39 | 1.60 | 1.83 | 2.11 | 2.39 |
| 4-5 | 12 | 2.01 | 0.84 | 0.91 | 1.19 | 1.46 | 1.72 | 2.47 | 2.80 | 3.96 |
| 5-6 | 17 | 1.99 | 0.84 | 1.04 | 1.06 | 1.42 | 1.85 | 2.36 | 3.38 | 4.28 |
| 6-7 | 16 | 1.80 | 0.63 | 0.73 | 0.97 | 1.42 | 1.78 | 2.07 | 2.71 | 3.21 |
| 7-8 | 18 | 2.05 | 0.63 | 1.03 | 1.05 | 1.68 | 1.92 | 2.40 | 3.08 | 3.30 |
| 8-9 | 13 | 1.53 | 0.60 | 0.81 | 0.96 | 1.07 | 1.40 | 1.79 | 2.19 | 3.07 |
| 9-10 | 13 | 1.78 | 0.69 | 0.99 | 1.10 | 1.22 | 1.60 | 2.19 | 2.38 | 3.54 |
| 10-11 | 11 | 1.64 | 0.76 | 0.86 | 0.98 | 1.17 | 1.35 | 2.11 | 2.21 | 3.57 |
| 11-12 | 12 | 1.65 | 0.48 | 1.13 | 1.14 | 1.17 | 1.65 | 2.00 | 2.39 | 2.44 |
| 12-13 | 11 | 1.54 | 0.48 | 0.90 | 0.95 | 1.10 | 1.52 | 1.92 | 2.21 | 2.27 |
| 13-14 | 15 | 1.68 | 0.78 | 0.86 | 0.88 | 1.29 | 1.47 | 1.94 | 2.24 | 4.06 |
| 14-15 | 10 | 1.18 | 0.37 | 0.69 | 0.71 | 0.83 | 1.19 | 1.48 | 1.69 | 1.74 |
| Total | 305 | 1.83 | 0.82 | 0.98 | 1.07 | 1.36 | 1.70 | 2.11 | 2.71 | 3.00 |
Normative ratio for PU/AU average (proximal and distal).
| Age | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| <1 | 65 | 1.67 | 0.53 | 0.97 | 1.05 | 1.22 | 1.61 | 1.95 | 2.46 | 2.69 |
| 1-2 | 47 | 1.67 | 0.51 | 1.02 | 1.13 | 1.41 | 1.61 | 1.81 | 2.39 | 2.73 |
| 2-3 | 24 | 1.59 | 0.59 | 1.01 | 1.09 | 1.19 | 1.48 | 1.71 | 2.21 | 2.63 |
| 3-4 | 21 | 1.35 | 0.31 | 0.86 | 1.03 | 1.15 | 1.31 | 1.49 | 1.58 | 1.98 |
| 4-5 | 12 | 1.63 | 0.59 | 0.70 | 1.07 | 1.18 | 1.50 | 2.03 | 2.54 | 2.61 |
| 5-6 | 17 | 1.71 | 0.69 | 0.95 | 1.04 | 1.25 | 1.38 | 2.18 | 3.02 | 3.18 |
| 6-7 | 16 | 1.48 | 0.51 | 0.68 | 0.69 | 1.24 | 1.40 | 1.71 | 2.18 | 2.77 |
| 7-8 | 18 | 1.70 | 0.49 | 0.86 | 0.99 | 1.40 | 1.54 | 1.99 | 2.48 | 2.50 |
| 8-9 | 13 | 1.29 | 0.45 | 0.69 | 0.85 | 1.03 | 1.27 | 1.42 | 1.62 | 2.49 |
| 9-10 | 13 | 1.63 | 0.59 | 0.91 | 1.16 | 1.22 | 1.52 | 1.67 | 2.09 | 3.27 |
| 10-11 | 11 | 1.39 | 0.53 | 0.88 | 0.94 | 0.98 | 1.25 | 1.82 | 1.91 | 2.61 |
| 11-12 | 12 | 1.38 | 0.37 | 0.98 | 1.01 | 1.03 | 1.31 | 1.60 | 1.83 | 2.17 |
| 12-13 | 11 | 1.22 | 0.34 | 0.76 | 0.80 | 0.90 | 1.21 | 1.44 | 1.53 | 1.89 |
| 13-14 | 15 | 1.35 | 0.42 | 0.73 | 0.78 | 1.11 | 1.30 | 1.66 | 1.81 | 2.42 |
| 14-15 | 10 | 1.04 | 0.29 | 0.64 | 0.66 | 0.86 | 1.01 | 1.26 | 1.41 | 1.53 |
| Total | 305 | 1.54 | 0.53 | 0.86 | 0.99 | 1.17 | 1.44 | 1.76 | 2.25 | 2.60 |
Normative ratio for PU/AU-for stratified age groups.
| Age (yrs) | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| 0-5 | 166 | 1.46 | 0.61 | 0.76 | 0.92 | 1.06 | 1.29 | 1.65 | 2.14 | 2.50 |
| 6-10 | 77 | 1.41 | 0.55 | 0.74 | 0.77 | 1.05 | 1.29 | 1.58 | 2.20 | 2.63 |
| 10-15 | 58 | 1.14 | 0.35 | 0.65 | 0.72 | 0.93 | 1.09 | 1.26 | 1.69 | 1.86 |
Normative ratio for PU/AU of the proximal segment
Normative ratio for PU/AU-for stratified age groups.
| Age (yrs) | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| 0-5 | 166 | 1.60 | 0.51 | 0.96 | 1.04 | 1.22 | 1.52 | 1.87 | 2.37 | 2.61 |
| 6-10 | 77 | 1.57 | 0.56 | 0.85 | 0.97 | 1.22 | 1.46 | 1.74 | 2.48 | 2.77 |
| 10-15 | 58 | 1.32 | 0.42 | 0.73 | 0.80 | 1.04 | 1.24 | 1.53 | 1.89 | 2.17 |
PU/Distal segment of anterior urethra
Normative ratio for PU/AU-for stratified age groups.
PU/Average of proximal and distal segments of anterior urethra
| Age (yrs) | N | Mean | SD | p5 | p10 | p25 | p50 | p75 | p90 | p95 |
|---|
| 0-5 | 166 | 1.60 | 0.51 | 0.96 | 1.04 | 1.22 | 1.52 | 1.87 | 2.37 | 2.61 |
| 6-10 | 77 | 1.57 | 0.56 | 0.85 | 0.97 | 1.22 | 1.46 | 1.74 | 2.48 | 2.77 |
| 10-15 | 58 | 1.32 | 0.42 | 0.73 | 0.80 | 1.04 | 1.24 | 1.53 | 1.89 | 2.17 |
Normative ratios determined for each age group (stratified into 3 blocks: 0-5 years, 6-10 years and 11-15 years).
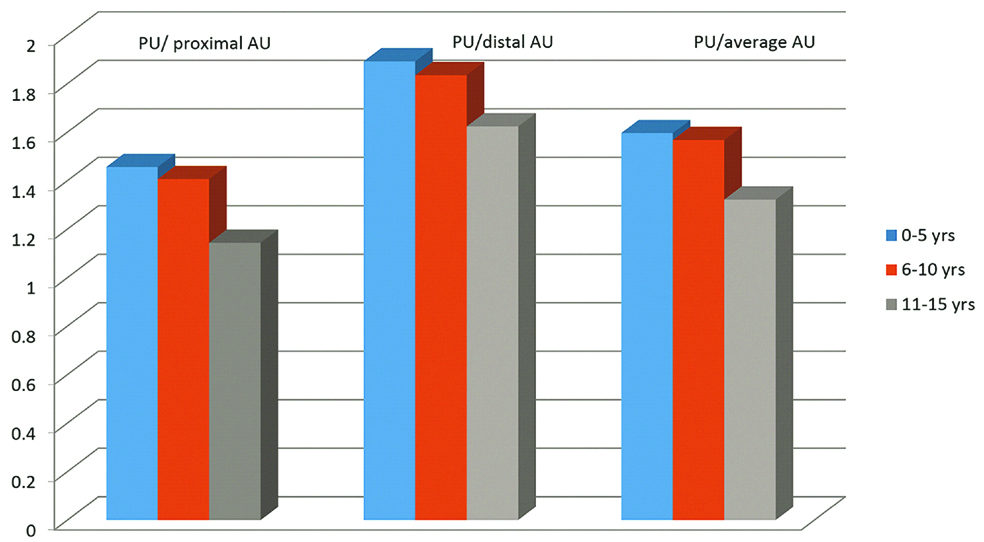
Significantly we also found a general trend of decreasing ratios with progression in the patients age from 1.62 in <1-year-old to 1.04 in 14-15-year-old as depicted in [Table/Fig-8,9 and 10].
The ratios were again assessed after stratifying the children (0 to 5 years, 6 to 10 years and 11 to 15 years) and the decreasing trend was found to remain consistent as depicted in [Table/Fig-11a and 11b].
Discussion
Assessment of Urethral Ratio on VCUG
Urethral ratio assessment has been used thus far in few studies that evaluated the adequacy of posterior urethral valves ablation as a “simple, objective and quantitative measurement” of the success of ablation [7-9]. In the study done by Bani Hani O et al., in 23 children less than 1 year who had undergone treatment by the same surgeon, a mean urethral ratio of 8.6 (ranging from 4 to 14.7) was obtained in 13 patients in whom pre-operative films were available with conclusion that a urethral ratio of 3.5 represented an acceptable post op result. The ratio was 2.6 in 31 normal males undergoing VCUG for investigation of UTI [8].
In the study by Gupta RK et al., mean urethral ratio in the pre and fulguration group was 4.94 (±2.97) and 2.134 (±1.19) respectively [9]. Ratio in the control group of 1.73 (±0.577) was significantly different from the pre-fulguration group result, but not significantly different in comparison to the post-fulguration group.
In the study by Menon P et al., morphological urethral changes three months following fulguration were assessed by evaluating urethral ratio and correlating with patients’ clinical status in an attempt to identify guidelines towards performing a second fulguration [10]. They concluded that in the presence of inadequate fulguration, an elevated ratio persisted. Also, mean urethral ratio in the control group was 0.33 to 1.67, with a mean and standard deviation of 1.04 and ±0.293 respectively.
VCUG and Cystoscopy in Assessment of PUV
de Kort LMO et al., evaluated reliability of VCUG to diagnose infravesical obstruction in boys, inter-observer agreement in the assessment of VCUG for infravesical obstruction and correspondence of VCUG findings with cystoscopy [11]. They concluded VCUG could not predict the presence of endoscopic infravesical obstruction accurately.
Cystoscopy being the current reference standard in the diagnosis of infravesical urethral obstruction [6,7] has been used as such in this study with disadvantages being its invasive nature and the need for general anaesthesia. Further, although cystoscopy offers direct visualisation of urethral abnormalities, de Kort LMO et al., concluded it is subjective as the paediatric surgeon judges whether valves or ring forms significant obstruction [11]. The ideal situation would be assessing cystoscopy in combination with post operative urodynamic testing and clinical follow up. As this data is not yet available, cystoscopy remains the current reference standard.
Limitation
The main limitation of the present study is the invasive nature of the reference standard and requirement for hospitalisation and general anaesthesia. Although cystoscopy is the current reference standard, it is still a subjective investigation. Hence, an ideal situation would be to assess cystoscopy in combination with postoperative urodynamic testing and clinical follow-up. This data however is not yet available. It is unethical to carry out an invasive procedure in a child with a normal urethral appearance on the VCUG to prove the absence of valves. A practical difficulty encountered in urethral measurement, especially the anterior urethra was inaccuracy in measurement of small diameters compounded by reduced resolution and resultant blurred edges when images were enlarged to aid measurement. An attempt to assess correlation between certain parameters seen on the VCUG (lucent filling defect, significant post void residual urine and PU dilatation) with outcome on cystoscopy for presence of a PUV was of no clinical significance due to very small numbers in each cell and the skewed outcome.
Conclusion
VCUG has a high sensitivity, specificity, positive and negative predictive value when compared with cystoscopy which is the current reference standard in the diagnosis of posterior urethral valves.
The PU/AU ratio is a valid indicator of the presence of PUV. In assessing the ratio of PU to AU on an VCUG it is more accurate if the ratio calculated is PU to the average of distal segment of AU and proximal segment of AU due to variability of anterior urethral diameter with varying distension rather than assessing AU based on a single measurement.
A value ≥2.11 suggests that the patient most likely has a PUV (sensitivity 83%, specificity 91%, 95% Confidence Interval-0.84-0.96).
The calculation of the normative ratios of PU/AU for the three measurements, to the best of our knowledge, has not been described till date. Ratios in normal boys showed a general trend of decreasing ratios with progression in age up to 15 years.
Cystourethrogram is a useful test in predicting presence of PUV, comparable to cystoscopy which is the current reference standard despite its drawbacks.
Normative ratio for PU/AU of the proximal segment
PU/Distal segment of anterior urethra