Periapical Cemento-Osseous Dysplasia in Anterior Maxilla
Francisca Lívia Parente Viana1, Bruno Carvalho De Vasconcelos2, Filipe Nobrechaves3, Karuza Maria Alves Pereira4, Marcelo Bonifácio Da Silva Sampieri5
1 Student, Department of Stomatology, Federal University of Ceara-Campus, Sobral, Ceará, Brazil.
2 PhD, Department of Endodontics, Federal University of Ceara-Campus, Sobral, Ceara, Brazil.
3 PhD, Department of Stomatology, Federal University of Ceara-Campus, Sobral, Ceará, Brazil.
4 PhD, Department of Stomatology, Federal University of Ceara, Fortaleza, Ceará, Brazil.
5 PhD, Department of Stomatology, Federal University of Ceara-Campus, Sobral Ceará, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Francisca Lívia Parente Viana, Rua Miguel Teles da Frota 217, Sobral, Ce, Brazil.
E-mail: liviapviana@hotmail.com
Periapical cemento-osseous dysplasia is a reactional fibro-osseous lesion that affects the supporting tissues of vital teeth. A 33-year-old female was referred for endodontic retreatment of the right maxillary central incisor with chief complaint of pain. On radiographic examination, endodontic treatment in tooth 11 and external root resorption in the apex of tooth 12 were observed. Moreover, a radiopaque lesion circled by a radiolucent halo involving the roots of teeth 11 and 12 was also present. The cone beam computed tomography showed resorption and perforation of the cortical bone. The result of the histopathological examination combined with the clinical findings made it possible to confirm the diagnosis of periapical cemento-osseous dysplasia. This case report emphasises on the value of association between imaging findings and histopathological examination in the diagnosis of such lesions.
Cone-beam computed tomography, Maxillary fibro-osseous lesions, Periapical cemento-osseous dysplasia
Case Report
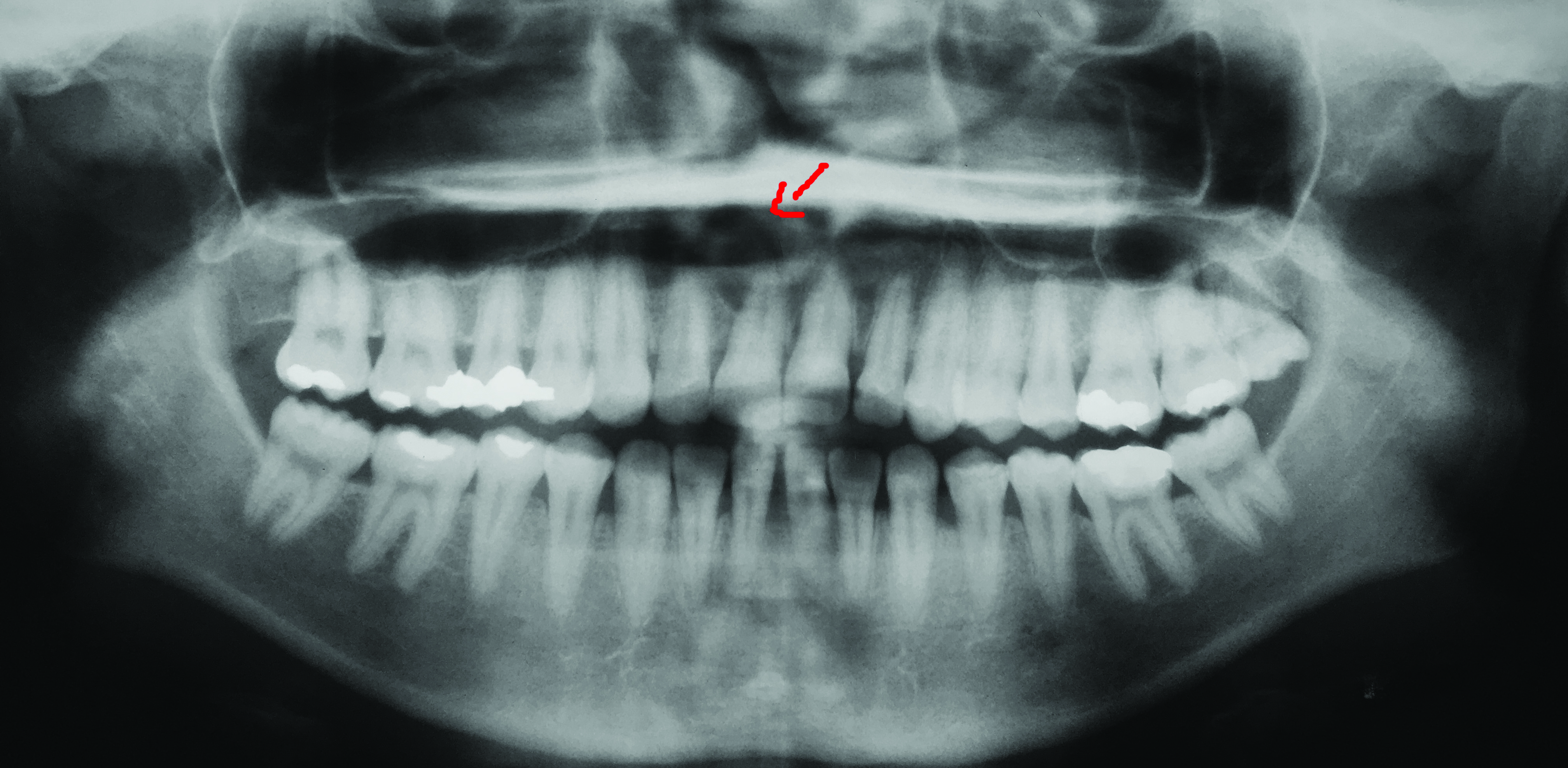
A 33-year-old white female was referred for endodontic retreatment of the right maxillary central incisor due to the presence of pain since last 30 days. The patient reported that she had undergone endodontic treatment in this tooth 10 years ago. A 10-year-old panoramic radiograph showed a radiolucent area of 1 cm of diameter associated with the root of tooth 11. Probably, the presence of such radiolucent lesion indicated the need of endodontic treatment [Table/Fig-1]. Moreover, the patient finished orthodontic treatment three months ago, after which she reported pain in teeth 11 and 12.
Initial panoramic radiography performed previously to the endodontic treatment (approximately 10 years ago).
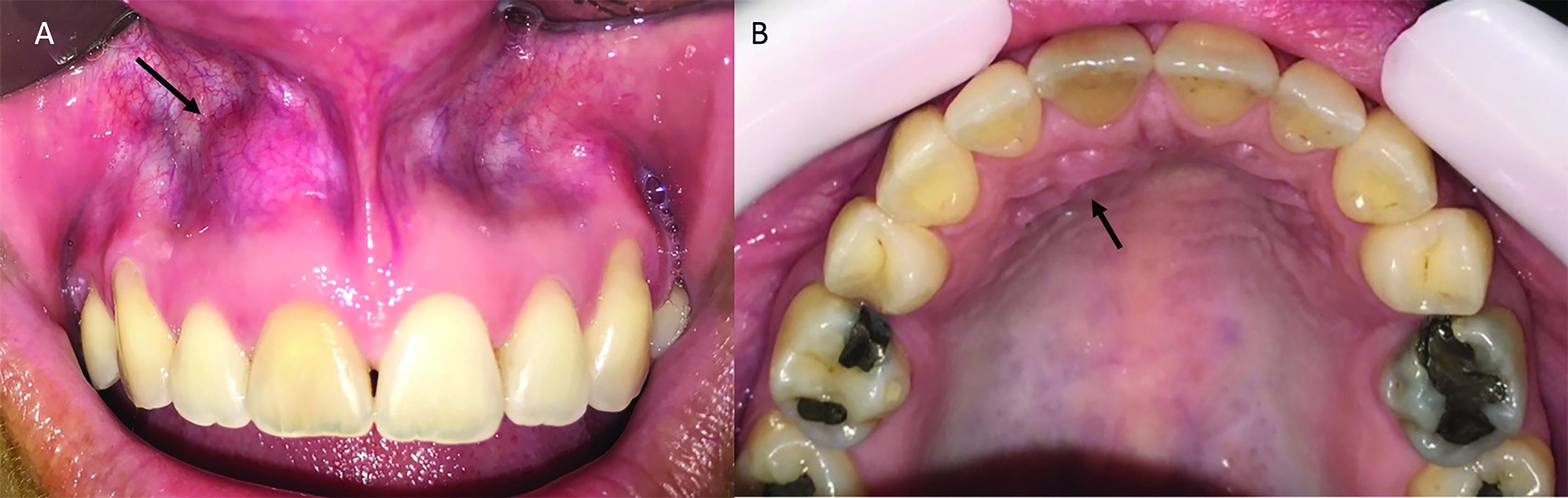
During inspection, a swelling of approximately ≈1 cm of diameter was seen in the labial vestibule and anterior palate associated with teeth 11 and 12 [Table/Fig-2a,b]. On palpation, the lesion was hard in consistency. The patient exhibited a normal response to the percussion test when tooth 11 was evaluated. However, the sensitivity test was negative for tooth 11 and positive for tooth 12, 21 and 22. The periapical radiographic examination revealed that tooth 11 had undergone endodontic treatment and that tooth 12 presented external root resorption. Moreover, at the roots of teeth 11 and 12, a radiopaque lesion of approximately 1 cm circled by a radiolucent halo was observed [Table/Fig-3].
Intra oral examination. Labial view (a) and palatal view (b)-black arrow.
Initial periapical radiograph.

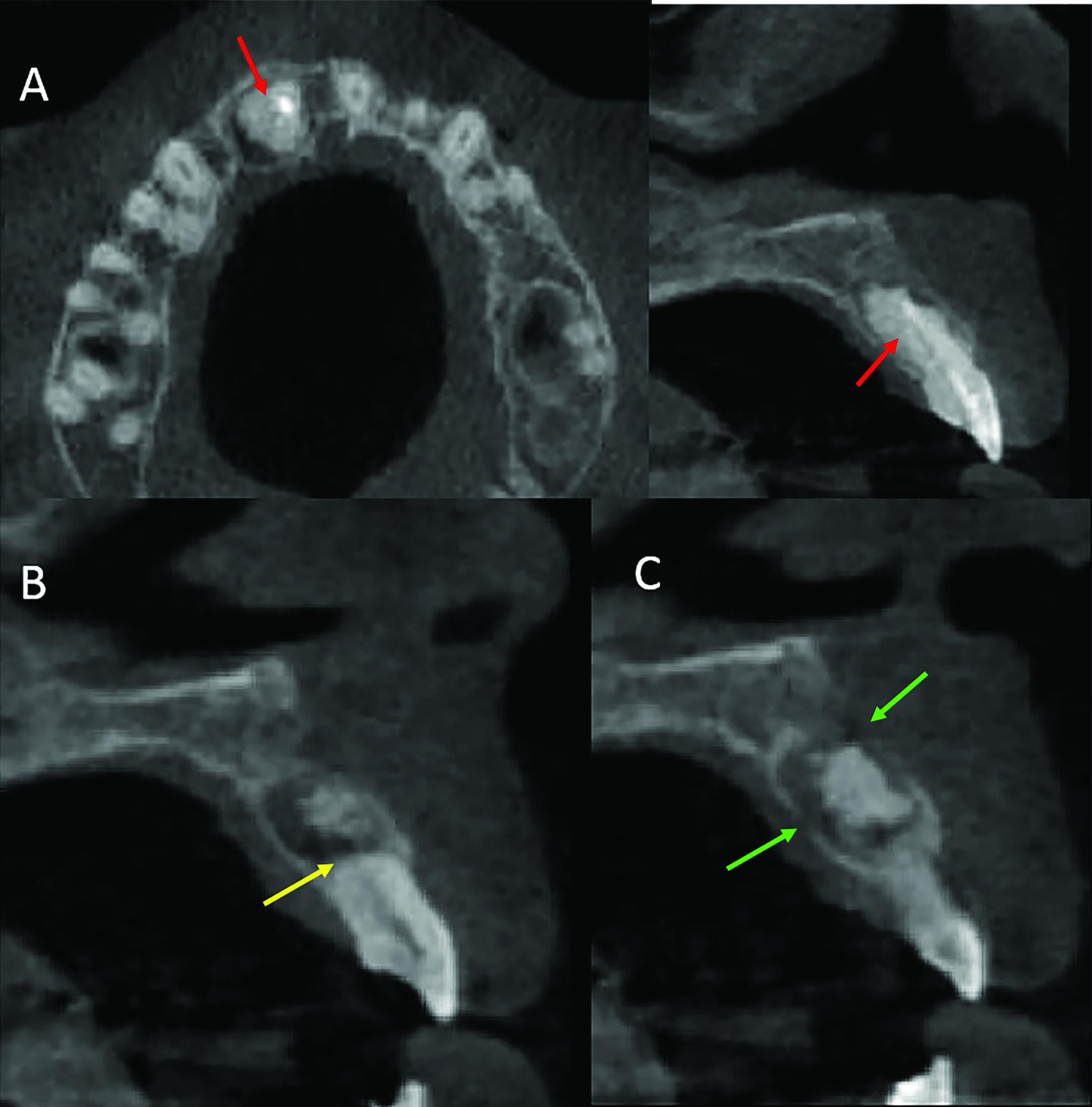
The clinical aspects and the uncertainty regarding the size of the lesion required deeper investigation. Thus, a cone-beam computed tomography was performed. At the tomographic examination, it was possible to observe that there was a poor definition between the limits of the lesion and the roots of the teeth, which presented loss of the periodontal ligament space [Table/Fig-4a]. Besides, vertical root resorption was also seen in tooth 12, which coincided with the extension of the lesion [Table/Fig-4b]. At the parasagittal plane, the lesion caused fenestration of the buccal and palatal cortical bone [Table/Fig-4c].
a) In the axial and parasagittal planes loss of the space of the periodontal ligament is seen in tooth 11. In this site, the limits between lesion and tooth root are not clear-red arrow. b) In the parasagittal plane, external root resorption can be seen in tooth 12, which matches the extension of the lesion-yellow arrow. c) In this parasagittal plane, it can be seen that the lesion provoked fenestration of the cortical bone in both buccal and palatal sides-green arrow.
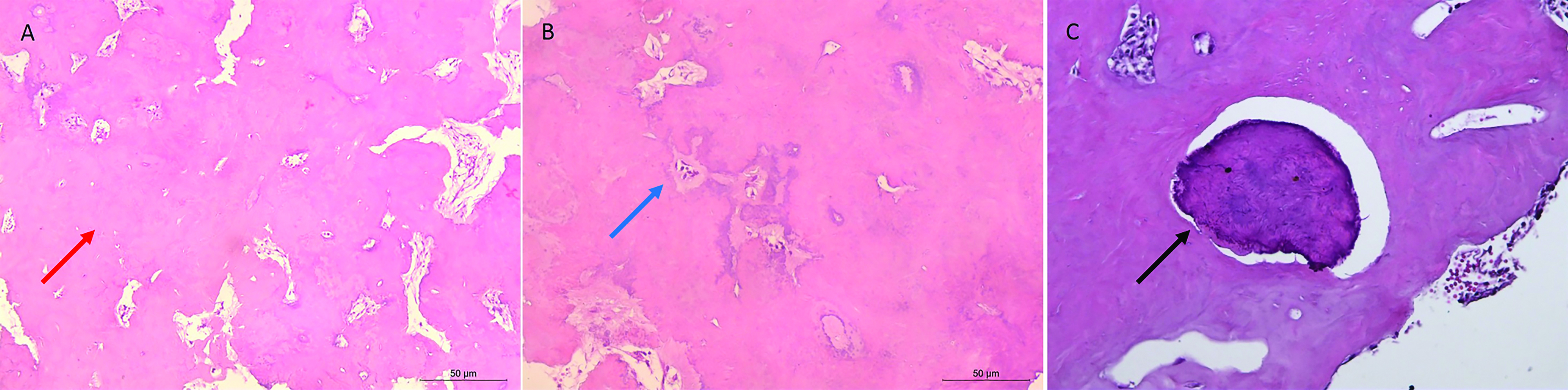
An incisional biopsy of the lesion was performed under local anaesthesia and a 0.5 cm diameter fragment of the lesional hard tissue was removed and sent for histopathological examination. The histopathological examination revealed fragments of bone tissue with unorganised lamellae containing fibrovascular tissue exhibiting signs of sclerosis. Moreover, a peripheric discontinuous thin fibrous capsule was also present [Table/Fig-5]. Thus, the diagnosis of periapical cemento-osseous dysplasia was established by association of the clinical, imaging and histopathological features of the lesion. The patient was explained and advised to maintain follow-up visits to the clinician. This same patient was evaluated one year after the diagnosis [Table/Fig-6a], and the swelling in labial vestibule in relation to 11 was regressed. It could also be seen radiographically that the radiolucent area had decreased in size [Table/Fig-6b].
(a) Histopathological examination shows a lesion formed predominantly by mineralised tissue with varying degrees of mineralisation in the form of osteoid, bony trabeculae (H and E, x100)-red arrow. (b) Bone tissue containing osteocytes permeates basophilic area (H and E x200)- blue arrow. (c) cementum-like material (H and E, x200)-black arrow.
One year and 5-month follow-up (a) intra oral examination and (b) periapical radiograph.

Discussion
Cemento-osseous dysplasia is a type of lesion in which the normal bone is replaced by a fibrous tissue that contains focal mineralised substances. Due to the similarity with a number of other oral pathologies, the clinical diagnosis is eventually challenging. The periapical cemento-osseous dysplasia is a specific type of cemento-osseous dysplasia that affects more commonly the anterior mandible of middle-aged women [1-5]. A 0.4% worldwide prevalence of cemento-osseous-dysplasia has been reported, and within this percentage, periapical cemento-osseous dysplasia accounts for 57.3% of the diagnosis. The present case report does not corroborate with the literature in regard to the most affected site since we diagnosed a periapical cemento-osseous dysplasia in the anterior maxillae. Only a few cases of periapical cemento-osseous dysplasia affecting the anterior maxillae have been reported, which emphasises the rarity of this clinical presentation [5-7].
Radiographically, the periapical cemento-osseous dysplasia presents three developmental phases: (I) Osteolytic stage-It is the initial phase in which the lesion presents well-defined radiolucent areas associated with the apical third of a tooth root; (II) Maturation stage-A stage characterised by the presence of radiolucent areas containing nodular radiopaque deposits; (III) Mature stage-A phase characterised by a well-defined dense radiopaque area circled by a radiolucent halo. At this last phase, the periodontal ligament separates the lesion from the root [8-11]. The evolution of the lesion might take months or even years. In this case report, the initial panoramic radiography showed a well-defined radiolucent area associated with the root of tooth 11. The initial phases of periapical cemento-osseous dysplasia might be misdiagnosed due to the similarity with other periapical lesions, such as abscesses, granuloma, or periapical cysts. These different possibilities of differential diagnosis might lead to an unnecessary endodontic treatment. The more recent periapical radiography of our patient showed that the lesion evolved to the mature stage. Other different aspect of the case reported is that the lesion seemed to be associated with the tooth root, so no differentiation could be made between periodontal ligament and the radiopaque area. Histologically, the lesion reported in our study exhibited signs of sclerosis, which corroborated with the study of Sapp JP et al., [8].
The use of the cone-beam computed tomography to diagnose periapical cemento-osseous dysplasia allows a more accurate study of the lesions, mainly of the localisation regarding the roots and condition of the cortical bone, periodontal ligament, and lamina dura [5,12]. In our case report, the tomographic examination was of extreme value in the observation of how the cortical bone was being resorbed by the lesion in the labial-palatal direction. This characteristic reveals an atypical and rare manifestation of periapical dysplasia, which could not be seen in the panoramic radiograph.
The differential diagnosis is dependent on the developmental stage of the lesion. For instance, when the lesion is in the mature stage, the differential diagnosis might be cemento-ossifying fibroma, Paget disease [13], chronic osteomyelitis [14], and cementoma [15]. The diagnosis of the case reported in this study was challenging, since the tooth affected by the lesion had already received endodontic treatment, and vitality tests were no longer useful. The final diagnosis was based on clinical, histologic, and imaging features of the case. Cases of periapical cemento-osseous dysplasia does not require treatment, and only clinical follow-up is advised. However, since this case presented an aggressive behaviour, incisional biopsy was preceded for a better diagnosis and follow-up.
Conclusion
This paper shows a rare case of periapical cemento-osseous dysplasia involving the anterior maxilla with signs of bone expansion and root resorption, which could only be diagnosed through the association of clinical, histological and imaging findings.
[1]. Eskandarloo A, Yousefi F, CBCT findings of periapical cemento-osseous dysplasia: A case reportImaging Science in Dentistry 2013 43(3):215-18.10.5624/isd.2013.43.3.21524083217 [Google Scholar] [CrossRef] [PubMed]
[2]. Abramovitch K, Rice DD, Benign fibro-osseous lesions of the jawsDent Clin N Am 2016 60(1):167-93.10.1016/j.cden.2015.08.01026614954 [Google Scholar] [CrossRef] [PubMed]
[3]. de Noronha Santos Netto JN, Cerri JM, Miranda AMMA, Pires FR, Benign fibro-osseous lesions: clinicopathologic features from 143 cases diagnosed in an oral diagnosis settingOral Surg Oral Med Oral Pathol Oral Radiol 2013 115(5):e56-e65.10.1016/j.oooo.2012.05.02222981804 [Google Scholar] [CrossRef] [PubMed]
[4]. Ahmad M, Gaalaas L, Fibro-osseous and other lesions of bone in the jawsRadiol Clin N Am 2018 56(1):91-104.10.1016/j.rcl.2017.08.00729157551 [Google Scholar] [CrossRef] [PubMed]
[5]. Cavalcanti PHP, Nascimento EHL, Pontual MLA, Pontual AA, Marcelos PGCL, Perez DEC, Cemento-osseous dysplasias: imaging features based on cone beam computed tomography scansBrazilian Dental Journal 2018 29(1):99-104.10.1590/0103-644020180162129267533 [Google Scholar] [CrossRef] [PubMed]
[6]. Heuberger BM, Bornstein MM, Reichart PA, Hürlimann S, Kuttenberger JJ, Periapical osseous dysplasia of the anterior maxilla: a case presentationSchweiz Monatsschr Zahnmed 2010 120(11):1001-11. [Google Scholar]
[7]. Rodrigues CD, Estrela C, Periapical cemento-osseous dysplasia in maxillary teeth suggesting apical periodontitis: case reportGen Dent 2009 57(3):21-24. [Google Scholar]
[8]. Sapp JP, Eversole LR, Wysocki GP, Bone LesionsIn: Contemporary Oral and Maxillofacial Pathology 2002 St. Louis, USAMosby [Google Scholar]
[9]. Senia ES, Sarao MS, Periapical cemento-osseous dysplasia: a case report with twelve-year follow-up and review of literatureInternational Endodontic Journal 2015 48(11):1086-99.10.1111/iej.1241725425097 [Google Scholar] [CrossRef] [PubMed]
[10]. Woo SB, Central cemento-ossifying fibroma: primary odontogenic or osseous neoplasm?J Oral Maxillofac Surg 2015 73(12):S87-S93.10.1016/j.joms.2015.05.01026608158 [Google Scholar] [CrossRef] [PubMed]
[11]. Mainville GN, Turgeon DP, Kauzman A, Diagnosis and management of benign fibro-osseous lesions of the jaws: a current review for the dental clinicianOral Diseases 2017 23(4):440-50.10.1111/odi.1253127387498 [Google Scholar] [CrossRef] [PubMed]
[12]. Alsufyani NA, Lam EWN, Osseous (Cemento-osseous) dysplasia of the jaws: clinical and radiographic analysisJ Can Dent Assoc 2011 77:70 [Google Scholar]
[13]. Su L, Weathers DR, Waldron CA, Distinguishing features of focal cement-osseous dysplasia and cement-ossifying fibromasOral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 84(5):540-49.10.1016/S1079-2104(97)90271-7 [Google Scholar] [CrossRef]
[14]. Alawi F, Benign fibro-osseous diseases of the maxillofacial bonesAmerican Journal of Clinical Pathology 2002 118:S50-70.10.1309/NUXA-JUT9-HA09-WKMV14569813 [Google Scholar] [CrossRef] [PubMed]
[15]. Konopka W, Smiechura M, Stru_zycka M, Kozakiewicz M, Dzieniecka M, Ossifying fibromacementoma of jaw. Differences in histopathological nomenclatureOtolaryngologia Polska 2012 66(5):359-62.10.1016/j.otpol.2012.06.02723036127 [Google Scholar] [CrossRef] [PubMed]