Misdiagnosing Tubal Pregnancy: A Fortunate Mistake or a Challenging Concern
Anjali Mundkur1, Shubha Rao2, Jyothi Shetty3
1 Associate Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
3 Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shubha Rao, Assistant Professor, Department of Obstetrics and Gynaecology, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: shubharao257@gmail.com
Early pregnancy scan and a good antenatal care are the most important entities which most of the rural areas in India lack. Here, we report a case of late tubal pregnancy who was mistakenly diagnosed as abdominal pregnancy. Intraoperative findings showed an unruptured 16 weeks tubal ectopic pregnancy which states that at such an advanced gestation it would be very difficult to diagnose either. This states the importance of an early ultrasound diagnosis of an intra-uterine pregnancy especially in developing countries which is required in each and every antenatal patient to ensure a safe and a healthy pregnancy.
Abdominal pregnancy, Diagnostic dilemma, Tubal ectopic pregnancy
Case Report
A 26-year-old G2P1L1 was referred with an ultrasound-based diagnosis of abdominal pregnancy of 16 weeks period of gestation. Her chief complaint was an abdominal pain for four days. The pain was mainly present in left iliac fossa, dragging in nature and was not radiating in type. Her previous pregnancy was uneventful and ended up with a full-term vaginal delivery.
On examination, the patient pulse and blood pressure were haemodynamically unstable. On per abdominal examination, there was palpable mass of 16 weeks, per vaginal examination could not reveal anything in particular because of severe pain when attempting it which pointed us more to an array of diagnosis which included pregnancy leading to an abortion, torsion ovary, ruptured uterus, fibroid complicating pregnancy. Mobilisation of the uterus was limited in this case.
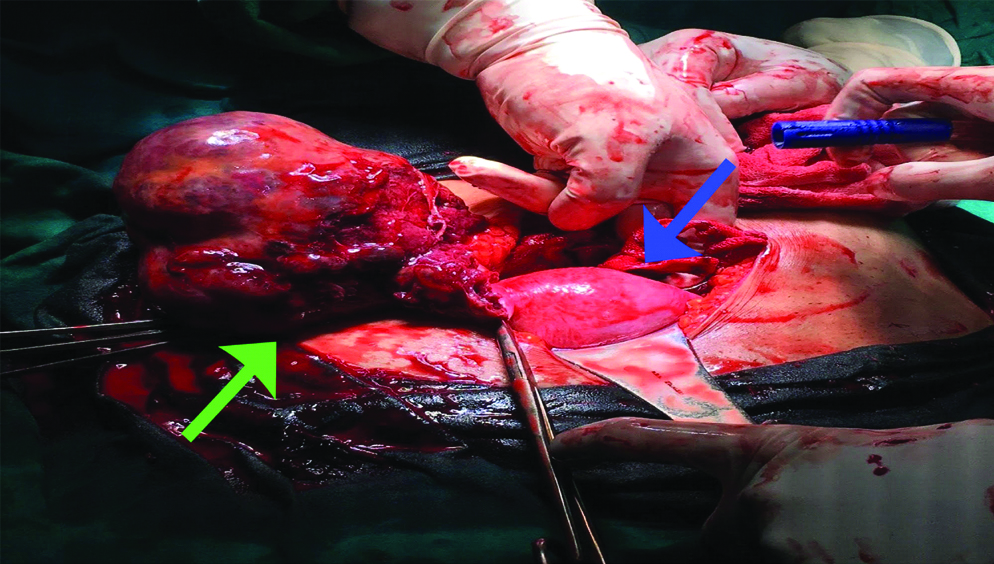
The sonographic examination found an empty uterus with the live foetus of 16 weeks in the abdominal cavity. Minimal free fluid in pouch of Douglas. With the suspicion of abdominal pregnancy, an emergency laparotomy was carried out in the presence of senior gynaecologists, surgeons, and ICU intensivist, if required. A duly informed consent was taken. Laparotomy revealed a vascular cystic structure in right tube at the ampullary region measuring around 10×7 cm [Table/Fig-1]. The uterus was bulky and the left fallopian tube and ovary were normal. However, as the right tube showed an ampullary ectopic pregnancy corresponding to 16 weeks period of gestation, right salpingectomy was done and clots evacuated.
Intraoperative finding of uterus (blue arrow) with right unruptured ampullary ectopic (green arrow).
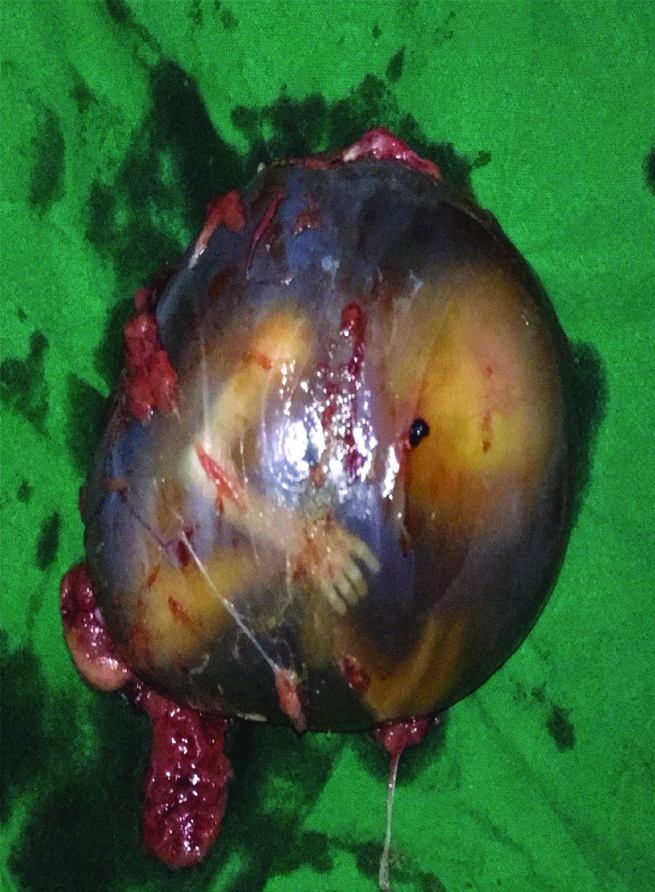
Peroperatively patient received one unit of packed red blood cell. The specimen obtained showed a live foetus contained within the amniotic sac and the placenta attached to the antimesenteric border of the fallopian tube [Table/Fig-2]. The patient had an uneventful post-operative recovery.
Specimen showing 16 weeks size foetus weighing 280 grams.
Discussion
Advanced tubal ectopic is rare, this is because of the present modalities such as early transvaginal ultrasound on the diagnosis of pregnancy which confirms the location of pregnancy and B-HCG doubling time which allows early detection of ectopic pregnancy. Ectopic pregnancy is symptomatic early. In our case, the absence of symptoms, regular antenatal care and no ultrasound done in the first-trimester possible led to the diagnosis of ectopic pregnancy.
Because of the low incidence, high misdiagnosis rate, and overlap of clinical signs and symptoms, the diagnostic options available for tubal ectopic pregnancy may sometimes be erroneous. In comparison to abdominal pregnancy, tubal ectopic pregnancy is an equally life-threatening situation. However, as pregnancy advances, it often becomes difficult to diagnose them as they share almost a similar picture. The case reported here was admitted with complaints of four months of amenorrhoea with abdominal pain. On further investigating a challenging diagnosis of abdominal pregnancy of 16 weeks was made which intraoperatively left us perplexed to find an unruptured ampullary ectopic pregnancy.
The incidence of ectopic pregnancies varies from 10 to 39.5/1000 deliveries [1,2]. There have been very few cases of reported late tubal ectopic pregnancy in the literature due to which there have been no documented incidences of late tubal ectopic pregnancy, in comparison the general rate of abdominal pregnancy is about 10.9 per 100,000 live births. This declining trend is as a result of increasing awareness and improved antenatal care [3,4].
There are many risk factors for an ectopic pregnancy which includes a previous ectopic, presence of tubal damage, history of infertility, IVF treatment [5] but half of the women have no associated risk factors as seen in this case [6].
In developing countries such as ours, ectopic pregnancies are most often discovered when ruptured. Most common time of occurrence is usually noted between 5 and 11 weeks of gestation [7].
There have been very rare cases of advanced tubal pregnancies reported. A similar case was reported by Elie N et al., in northwest Nigeria where there was a co-existence of advanced tubal ectopic ruptured with schistosomiasis [7]. Another study by Sachan R et al., where they reported two such advanced tubal unruptured ectopic [8]. Cases reported by Mhaskar R et al., and Gueyea MDN et al., showed a similar presentation as was seen in our patient and timely intervention done guaranteed a safe post-operative recovery as seen [9,10].
There have been very few cases reported where there was a misdiagnosis of abdominal pregnancy as was seen in our case. One such case has however been reported by Ikechebelu JI et al., where a multigravida with complaints of abdominal pain was diagnosed as abruption placenta. Laparotomy findings showed an abdominal pregnancy of a female live foetus weighing 2.6 kg was delivered and post-operative period was uneventful [11]. Although Allibone GW et al., has provided guidelines for the use of USG to diagnose abdominal pregnancy; the reported diagnostic errors in different series have ranged from 50% to 90% [12], therefore making the diagnosis of abdominal pregnancy complex. Ultrasound, when coupled with clinical evaluation, has approximately a 50 percent success rate in the diagnosis of the site of pregnancy [13].
The treatment of advanced tubal ectopic is always a total salpingectomy and the need for the total hysterectomy is mainly dependent on the site of the ectopic.
Conclusion
This case points out the necessity of an early first-trimester scan for the diagnosis of pregnancy which would provide information regarding the number and site of pregnancy. However, ultrasound modalities will not be a confirmed method of differentiating tubal ectopic and abdominal pregnancy as the pregnancy advances due to the similarities in between the two entities thereby, early referral to a tertiary care centre is a must when there is high suspicion of ectopic pregnancy.
[1]. Shao R, Understanding the mechanisms of human tubal ectopic pregnancies: new evidence from knockout mouse modelsHum Reprod 2010 25(3):584-87.10.1093/humrep/dep43820023297 [Google Scholar] [CrossRef] [PubMed]
[2]. Kirk E, Bourne T, Ectopic pregnancyObstetrics, Gynaecology and Reproductive Medicine 2011 21(7):207-11.10.1016/j.ogrm.2011.04.003 [Google Scholar] [CrossRef]
[3]. Schorge J, Schaffer J, Halvorson H, Bradshaw K, Cunningham F, Hoffman B, Williams Gynaecology 2008 2nd edMcGrawHil [Google Scholar]
[4]. Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C, Williams obstetrics 2010 23rd edMcGrawHillhttps://www.ncbi.nlm.nih.gov/nlmcatalog/101510655 (accessed 2 Jun 2018) [Google Scholar]
[5]. Radaelli T, Bulfamante G, Cetin I, Marconi AM, Pardi G, Advanced tubal pregnancy associated with severe fetal growth restriction: a case reportThe Journal of Maternal-Fetal & Neonatal Medicine 2003 13(6):422-25.10.1080/jmf.13.6.422.42512962269 [Google Scholar] [CrossRef] [PubMed]
[6]. Marion LL, Meeks GR, Ectopic pregnancy: History, incidence, epidemiology, and risk factorsClin Obstet Gynaecol 2012 55(2):376-86.10.1097/GRF.0b013e3182516d7b22510618 [Google Scholar] [CrossRef] [PubMed]
[7]. Elie N, Eveline Foguem T, A case of a 26-week ampullary pregnancy mimicking intrauterine fetal deathAnatolian Journal of Obstetrics & Gynaecology 2012 (1):1-13. [Google Scholar]
[8]. Sachan R, Gupta P, Patel M, Second trimester unruptured ampullary ectopic pregnancy with variable presentations: Report of two casesInternational Journal of Case Reports and Images 2012 3(8):4 [Google Scholar]
[9]. Mhaskar R, Harish M, Jaiprakash T, Unruptured ampullary ectopic pregnancy at 16-week period of gestation with live fetusJ Obstet Gynaecol India 2014 64(1):73-74.10.1007/s13224-012-0228-724587614 [Google Scholar] [CrossRef] [PubMed]
[10]. Guèyea MDN, Guèyea M, Thiamb I, Mbayea M, Gayeb AM, Diouf AA, Unruptured tubal pregnancy in the second trimesterSouth Sudan Medical Journal 2013 6(4):95-96. [Google Scholar]
[11]. Ikechebelu JI, Onwusulu DN, Chukwugbo CN, Term abdominal pregnancy misdiagnosed as abruptio placentaNigerian Journal of Clinical Practice 2005 8(1):43-45. [Google Scholar]
[12]. Allibone GW, Fagan CJ, Porter SC, The sonographic features of intra-abdominal pregnancyJ Clin Ultrasound 1981 9(7):383-87.10.1002/jcu.1870090706 [Google Scholar] [CrossRef]
[13]. Costa SD, Presley J, Bastert G, Advanced abdominal pregnancyObstet Gynaecol Surv 1991 46(8):515-25.10.1097/00006254-199108000-00003 [Google Scholar] [CrossRef]