Simple spirometry remains the cornerstone of Pulmonary Function Test (PFT) and flow-volume spirometry is a useful investigation to assess lung function physiologically and in disease conditions [1]. FET signifies duration of forced expiration during spirometry. Normally majority of the inspired air (>70%) is expelled in the first second of the FVC manoeuver and the rest of the air is expelled in next few seconds [1]. Although, FET is not recommended as a traditional flow-volume spirometry variables like other commonly used indices of spirometry test such as FVC, FEV1, FEV1/FVC, FEF 25%-75% and PEFR [2]. Previously, several researchers reported that FET might be a useful index to assess small airways (<2 mm internal diameter) obstruction in those patients whose other spirometry indices such as FVC, FEV1, FEV1/FVC ratio were found within normal limit [3,4]. This small airways obstruction commonly reported in smokers before standard spirometry becomes abnormal [3]. Some authors [5] have opined that FET may be useful to assess the chronic airways obstruction in smokers and also may have role in epidemiological survey in these cases. Although, the diagnostic value of FET is still a controversial issue [6,7] the latest guidelines of American Thoracic Society and European Respiratory Society (ATS/ERS) (2005) had given a special interest in FET [8]. In spite of that due to lack of attention, there is paucity of relevant data regarding correlation between FET and other spirometry variables till date [9]. The spirometry indices such as ratio of Forced Expiratory Volume in one second (FEV1) to FVC (i.e., FEV1/FVC) and PEFR are the key factors to make clinical decision regarding lung pathology [10]. In the recent past, the authors of the present study were conducted a retrospective study with one of the above spirometric indices i.e., PEFR and its changes with relevant variables in the population of eastern India. This split study had shown clinical importance of PEFR as a risk assessment tool for the population having apparently normal lung health [11]. That’s why it is important to understand the relation of FET with these spirometry variables during a standard spirometry session where other variables are within normal range in nonsmokers. If found relevant; FET may prove to be a valuable index of spirometry. The present study aimed to evaluate the correlation of FET with anthropometric and spirometric indices in subjects having normal spirometry such as FVC, FEV1, FEV1/FVC, FEF25%-75% and PEFR.
Materials and Methods
A retrospective study was conducted at the spirometry laboratory at Department of Physiology, RG Kar Medical College Kolkata, West Bengal, India, with the stored data of normal test results between February 2016 and July 2016 of 220 patients including males and females (1:1). They were referred from different Outpatient Departments of RGKMCH, Kolkata during that period with chief complaint of Shortness Of Breath (SOB) and all was done this procedure for the first time. All study subjects were Legal residents of the state of West Bengal. Therefore, they could be assigned as Bengali by Ethnicity. According to inclusion criteria of the study, all of them were aged between 25 and 50 years as well as having normal spirometry values {FVC and FEV1 ≥80% to ≤120% predicted, FEV1/FVC ratio ≥0.7, forced expiratory flow in the middle half of the FVC (FEF25%-75%) of ≥50% of predicted [12] and PEFR >60% predicted [13] and they were all non-smokers as per record.
Exclusion criteria of the study were: 1) Restrictive impairment (FEV1 and FVC each <80% of predicted, with FEV1/FVC ratio ≥0.7 with FEV1 <80% of predicted) and obstructive impairment (FEV1/FVC ratio <0.7 with FEV1 <80% of predicted) test results [14];
2) FEF 25%-75% value <50% of predicted and PEFR value <60% of predicted;
3) Subjects with any cardiac ailments like angina pectoris with complaints of SOB (as written in their OPD cards);
4) Test that had been done using 100% ethnic corrections;
5) Age <25 years and >50 years;
6) Smokers as per record.
Appropriate administrative approval was taken for the proposed study from the Principal and Head of Institutional Ethical Committee, RG Kar Medical College and Hospital, Kolkata, West Bengal, India. This present study was conducted following ethical criteria laid down by World Health Assembly, Helsinki declaration, latest amendment in 2015. Written informed consent from every patient was already taken prior to the test.
Experimental protocol: At first data regarding anthropometric parameters like age, sex, height, weight, BMI and smoking habit (Smoking status:an ever-smoker was anyone who smoked cigarette, beedi, hookah, etc., regularly for at least one year and never-smokers were defined as those who never smoked regularly for one year or more) was collected and entered in master chart of the present study. Then spirometry tests were done and the stored data of the patients were gathered following inclusion and exclusion criteria of the present study. At every time the test was performed by RMS HELIOS-702 machine following American Thoracic Society/European Respiratory Society (ATS/ERS) latest guideline of 2005 [8] and using 80% ethnic correction (it had been customary to equate 80% predicted with the lower limit of normal as we had considered percent predicted values for statistical analysis [12,15-17].
Calibration of the testing machine was done on daily basis by using a calibrated syringe and following the latest guidelines of ATS/ERS [8] during the study period. The author checked the syringe for leaks and damage prior to the procedure and kept the syringe next to the spirometer. The largest observed values of FEV1 and FVC available from among at least three acceptable and reproducible tests were taken as the key parameters for interpretation. Pulmonary function indices were recorded as a percentage of the normal predicted value on reported height, age and sex [18] except FET which was recorded in seconds. Finally, only age, sex, BMI, FEV1/FVC ratio, PEFR (percentage value) and FET (seconds) had been chosen from the collected data sheet of each patient for statistical analysis.
Statistical Analysis
The data were expressed in Mean±Standard Deviation (SD). Descriptive analyses were performed using chi-square Test (for categorical variables) and two-sided z-tests (for continuous variables) to compare groups. All data of spirometry variables were expressed in percentage (%) form except FET (seconds). z-tests, r-value of Pearson’s correlation coefficient test among FET with study variables like age, BMI, FEV1/FVC ratio and PEFR, mean values and standard deviation were calculated using Microsoft excel sheet whereas chi-square test and statistical analysis of p-values was done using GraphPad QuickCals Software, California, USA. Differences were considered statistically significant at p-value <0.05.
Results
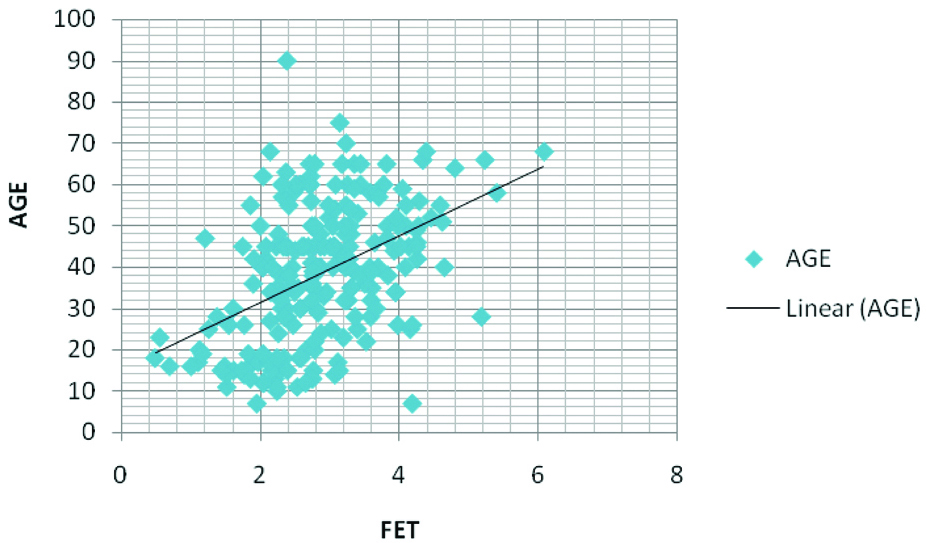
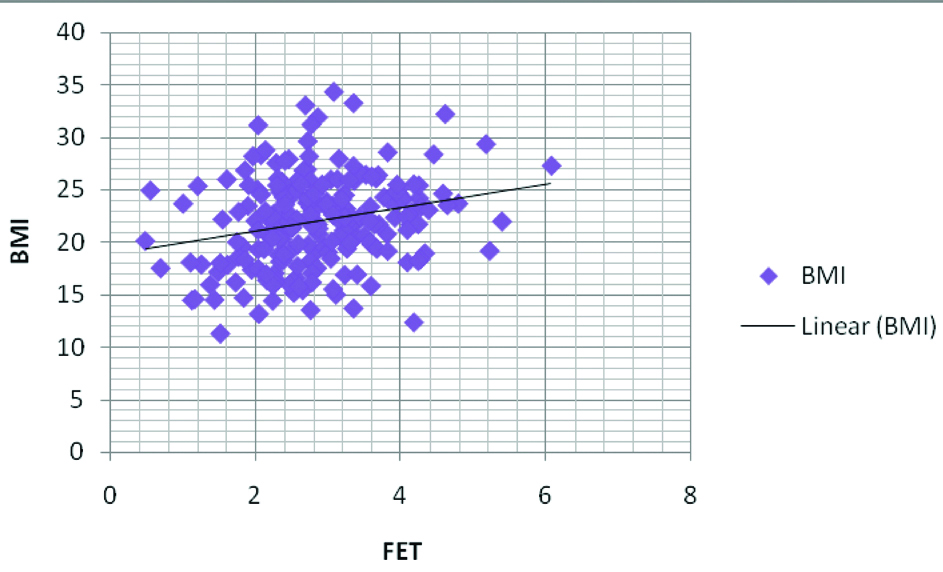
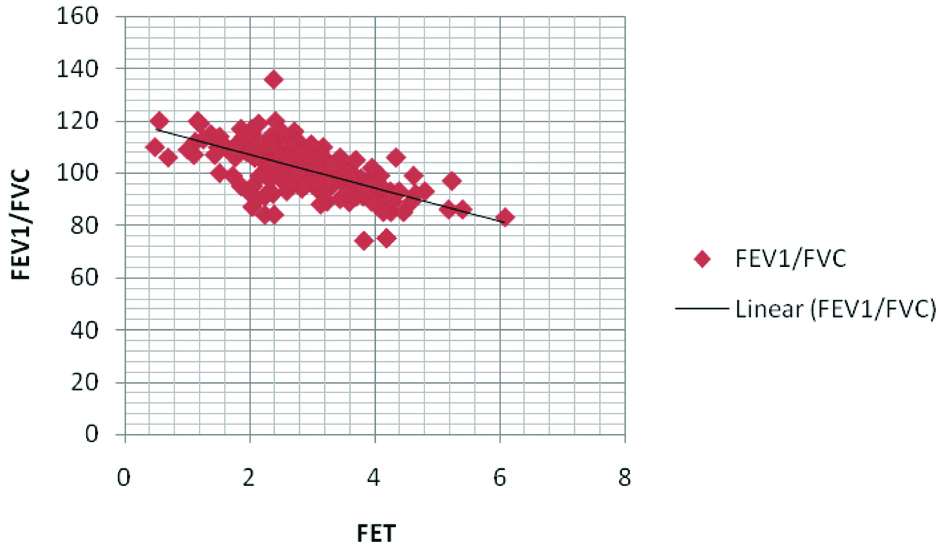
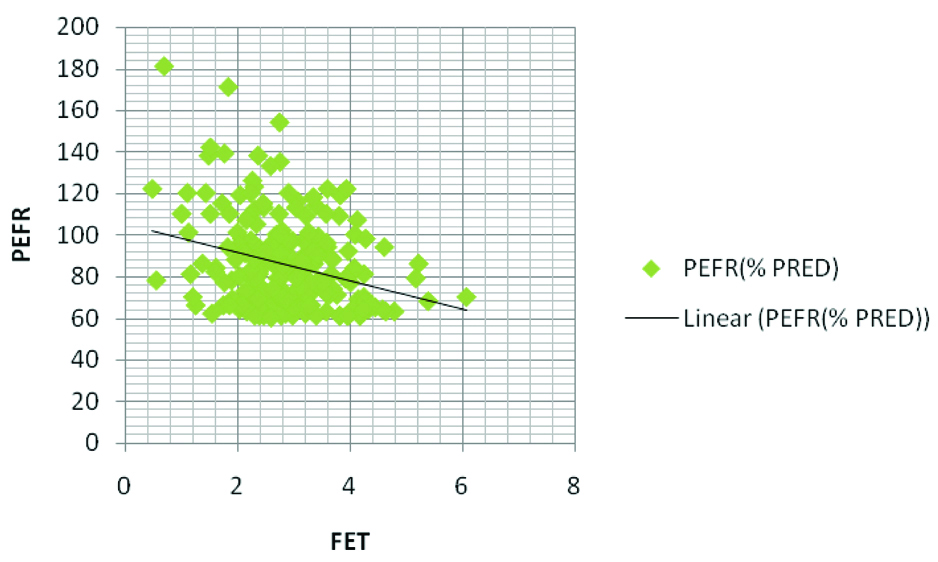
In this study mean age of the study population was around 39 years and was non-obese. Mean FET was around three seconds and mean values of other spirometry parameters like FVC, FEV 1, FEV 1/FVC, FEF 25%-75%and PEFR were well above the Lower Limit of Normal range (LLN) [Table/Fig-1]. FET had significant positive linear correlation with age and BMI respectively but significant strong negative linear correlation with FEV1/FVC and weak significant negative correlation with PEFR values in this study (That means FET increases with ageing and obesity whereas it increases with decreasing value of spirometric indices i.e FEV1/FVC and PEFR) [Table/Fig-2,3a,b,c and d]. These findings had shown FET progressively increased with increasing in age and BMI whereas a trend of gradual increment in duration of FET with increase degree of airway obstruction denoted by decreased mean value of FEV1/FVC and PEFR in this study subjects having normal spirometry.
Overall demographic, anthropometric andspirometric profile of the study population (n=220).
| Parameters | Analysed data |
|---|
| Age (years)(mean±sd) | 38.522±16.417 |
| BMI (kg/m2)(mean±sd_ | 22.074±4.178 |
| FVC (%)(mean±sd) | 102.4364±10.70785 |
| FEV1 (%)(mean±sd) | 103.5182±10.37888 |
| FEV1/FVC ratio (%)(mean±sd) | 101.563±8.992 |
| FEF 25%-75% | 68.54±11.41 |
| PEFR(%)(mean±sd) | 85.859±21.478 |
| FET (seconds)(mean±sd) | 2.872±0.903 |
Correlation of Forced Expiratory Time (FET) with anthropometric and spirometric indices in the study population (n=220).
| Indices | Pearson’s correlation coefficient (R) | p-value |
|---|
| Age | 0.445 | <0.0001* |
| BMI | 0.239 | 0.0002* |
| FEV1/FVC ratio | −0.639 | <0.0001* |
| PEFR | −0.285 | <0.0001* |
Graphical representation of the linear correlations of the above table; FET and AGE (n=220).
FET and FEV1/FVC ratio (n=220).
Discussion
The present study was aimed to find the correlation between FET and anthropometric as well as lung function parameters only, though author considered FET as a potentially relevant quality measurement for diagnostic purpose early on in the analysis. This study had chosen 80% ethnic correction factors implying that predicted values for a pulmonary index, because researchers were reported that the mean total lung capacity and vital capacity in the caucasian group, expressed as percentage predicted, was 17 and 20% higher than in the Indian group [19].
This present study observed that mean FET in study population was around three seconds and mean age was around 39 years which was close proximity with the study finding of Kotur NS, et al., where mean FET was reported as 2.65s in obese (mean age was 34 years) and in non obese it was 1.8 second (mean age was 30 years) [20]. Previously researchers documented that after expelling 70-80% of vital capacity rapidly and smoothly on first second it takes further 2-3 seconds to expire the remaining 20-30% in normal subjects and patients without airways obstruction [1,21]. Although there is paucity of data regarding cut-off range of FET for the healthy Indian population till date.
In this present study, FET had shown moderate positive correlation with age but strong negative correlation with the key spirometry parameter FEV1/FVC in both genders. These findings were similar to the previous study conducted by Kainu A et al., [22]. Researchers had shown that due to ageing various anatomical, physiological and immunological changes occur in respiratory system resulting in increased Functional Residual Capacity (FRC) and thus an increased airway resistance [23,24]. In addition, airway calibre decreases with age and the proportion of collapsible small airways increases, as well as the airways receptors, undergo functional changes with age resulting in increasing resistance in airways [24]. Therefore, FET tends to be prolonged with advancement of age in this study subjects.
Furthermore, this study observed significant positive correlation between FET and BMI. Previously researchers were reported similar results [22]. Kotur NS et al., had also shown that FET was prolonged in obese compared to non-obese population and they opined FET as one of the most significant and sensitive lung function test parameter [20]. Salome CM et al., documented that obesity causes increased demand for ventilation, elevated work of breathing, respiratory muscle inefficiency and diminished total respiratory compliance in almost two third of obese compared to normal individuals, leading to decrease in ERV followed by decrease in FRC with a high closing volume to FRC ratio in obese causes increase the risk of both expiratory flow limitation and airway closure at the dependent part of the lung [25]. Therefore, prolongation of FET might be indicative of some form of airflow limitation due to lower FRC in obese [20]. Thus, positive correlation between FET and BMI in the present study indicates reduction in respiratory well-being in obese, even in the absence of specific respiratory disease as seen in the present study.
On the other hand, a strong negative correlation between FET and FEV1/FVC observed in this study and this association was similar to the finding of Smith LJ et al., [26]. As the reduction in the FEV1/FVC ratio below the LLN of a normally distributed set of values of FEV1/FVC indicates large airflow obstruction for a population of non-smoking, normal individuals [27,28] as well as in severe cases <40% of the vital capacity is expelled in the first, second and the remainder takes much longer before patient being forced to take another breath leading to prolong FET [1]; therefore a reduced FEV1/FVC ratio results in increased forceful exhalation time could be suggestive for FET to be used as a supportive test to diagnose obstructive airways diseases.
Significant negative correlation between FET and PEFR in this study population corroborates with the observation of previous researchers [29]. A PEFR measure the force generated by the expiratory muscles [30] and also gives idea about the dimensions of the large intra and extrathoracic airways [31]. Generally, it is reduced in all type of respiratory diseases. Although its measured value is reduced more significantly in obstructive lung diseases such as asthma, emphysema, Chronic Obstructive Pulmonary Diseases (COPD) and chronic bronchitis compared to restrictive lung diseases. Over and above PEFR is highly sensitive to diagnose asthma than other respiratory diseases [32]. Hence, negative correlation of FET with PEFR might be indicated either large or small airflow limitation in subjects with normal spirometry.
Limitation
This study had some limitations that need to be considered. Firstly, this study did not assess the correlation between change in FET and clinical indices such as dyspnoea. As a small, retrospective study performed in a single centre with a relatively homogeneous population, the results may or may not vary in other settings. Secondly author analysed only the recorded duration of forceful expiratory effort but not the intensity of that effort which can be measured by Trans-diaphragmatic or maximum expiratory pressures. Moreover, whole-body plethysmography was not used to assess FRC, airway resistance and other variables.
Conclusion
The FET demonstrates as an important diagnostic tool in simple spirometry to assess airflow limitation even in subjects having normal results and helps to diagnose future obstructive airway diseases. Although the present analysis of FET provides insight into spirometric performance in a single testing session, a clinical role for FET was identified. It also suggests age related alteration in pulmonary mechanics and indicates pulmonary efficiency in obese. Future follow-up studies addressing the above limitations with large sample size of healthy volunteers can bring definitive conclusions. The role of FET in characterising bronchodilator response targeting to establish correlation with clinico-spirometric changes can also be considered.