Ewings Sarcoma of Fourth Metatarsal: A Rare Presentation
Chetan Peshin1, Kunal Das2, Ahmed Abdul Ghaffar3, Sirazul Haque Malik4
1 Associate Professor, Department of Orthopaedics, Himaliyan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
2 Assistant Professor, Department of Paediatric Hemato-oncology, Himaliyan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
3 Junior Resident, Department of Orthopaedics, Himaliyan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
4 Junior Resident, Department of Orthopaedics, Himaliyan Institute of Medical Sciences, Dehradun, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chetan Peshin, Assosciate Professor, Department of Orthopaedics, Himaliyan Institute of Medical Sciences, Jolly Grant, Dehradun-248016, Uttarakhand, India.
E-mail: chetanpeshin@gmail.com
Ewings sarcoma is a primary aggressive neoplasm of bone seen in the second decade of life. This is a case report of a 10-year-old male child who presented with Ewings sarcoma of fourth metatarsal of left side with no distant metastases. Patient was managed by neo-adjuvant therapy followed by wide excision of the tumour followed by adjuvant chemotherapy. He had a very good response and was disease free for up to two years on follow-up.
Primitive neuroectodermal tumours, Radiotherapy, Surgery
Case Report
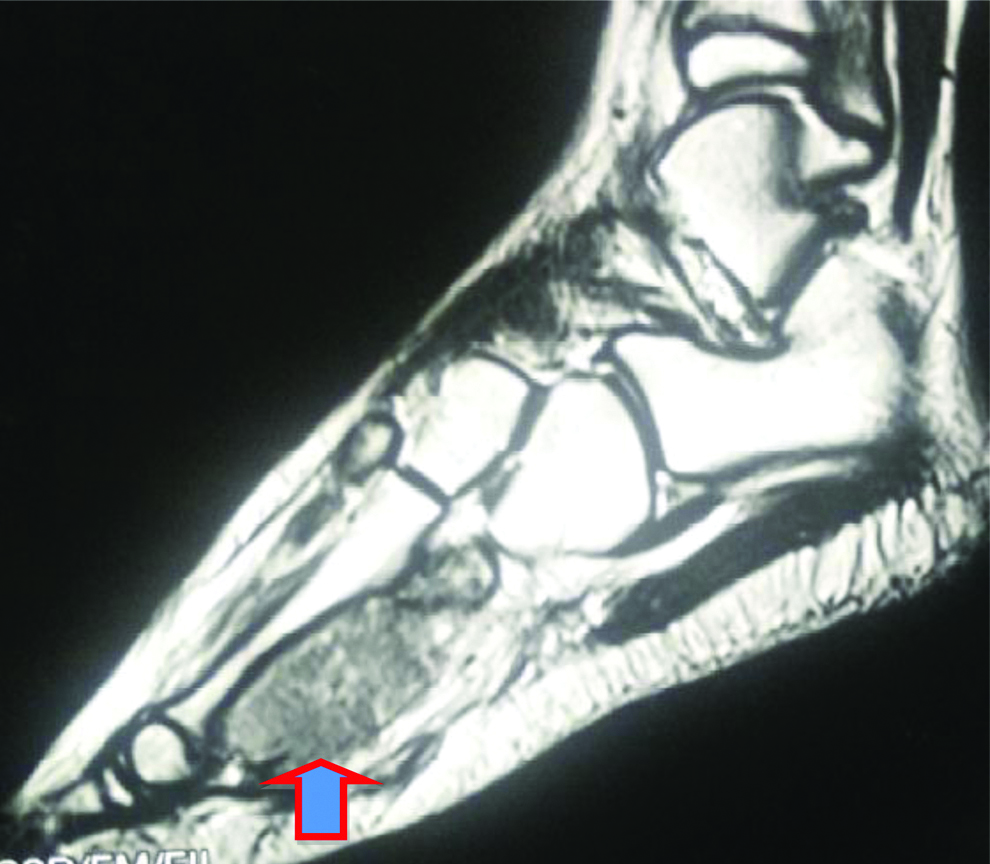
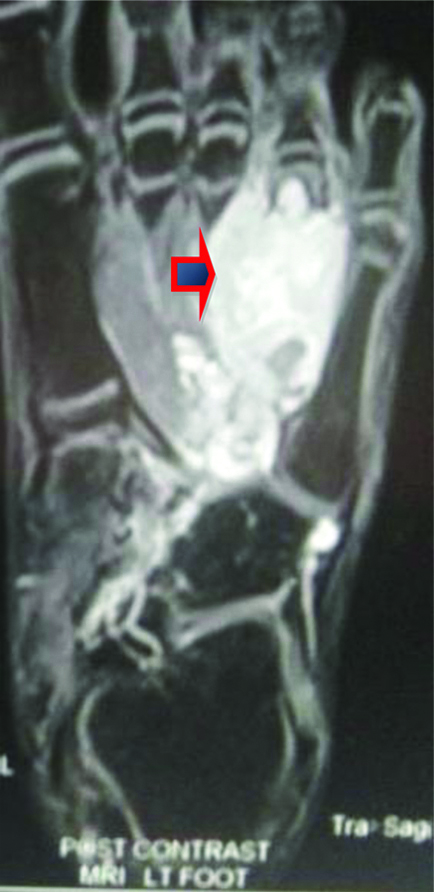
A 10-year-old male presented with complaints of difficulty in walking for three months and swelling in left foot for four days. There was a history of trauma to the left foot while playing three months back. He had no complaints till that time patient noted a swelling in left foot. On examination, mild swelling and tenderness were present at the dorsum left foot. There was no history of fever or significant weight loss. General physical examination did not show anything significant. The radiograph of left foot was taken and showed an expansile lytic lesion at fourth metatarsal [Table/Fig-1] with cortical breach, aggressive periosteal reaction and soft tissue extension. An MRI scan was done which showed a large soft tissue mass around the involved bone beneath the inferior cortex [Table/Fig-2,3]. The soft tissue mass was present in the fourth metatarsal of left foot with cortical breach and showing heterogeneous enhancement. The full blood count and erythrocyte sedimentation rate were normal (Total Leukocytes Count (TLC), platelet count, total erythrocyte count). Blood workup showed Serum ALP-208 and S. Calcium-9.4 mg/dL. All other parameters were normal. Workup including HRCT chest and bone scan did not reveal any distant metastasis. In view of painful swelling and imaging findings of soft tissue density with a cortical breach, clinical diagnosis of bone sarcoma was considered. Osteosarcoma, Ewings sarcoma and granulomatous infection of bone were considered as differential diagnosis.
Preoperative AP X ray of patient showing ill defined lesion in shaft of fourth metatarsal of left foot eroding both the cortices.

Preoperative MRI (sagittal) demonstrating large soft tissue mass with breach in inferior cortex (arrow) of the lesion.
Axial cut showing extent of soft tissue involvement (arrow) using t2 weighed post contrast MRI image.
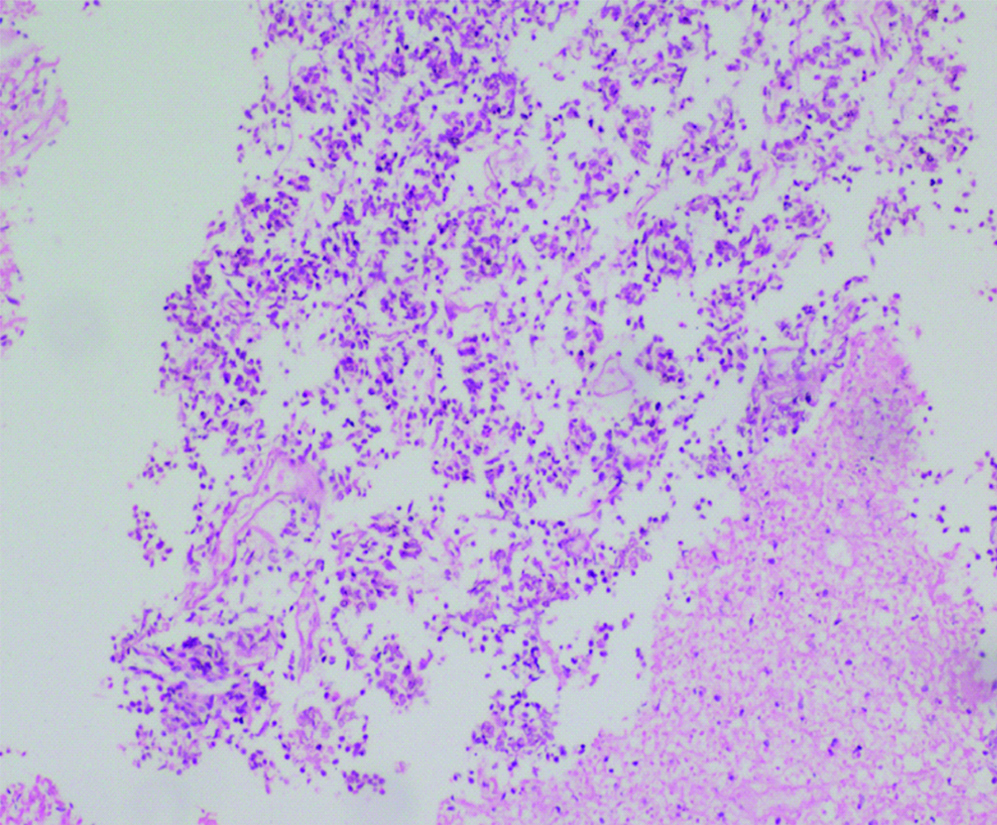
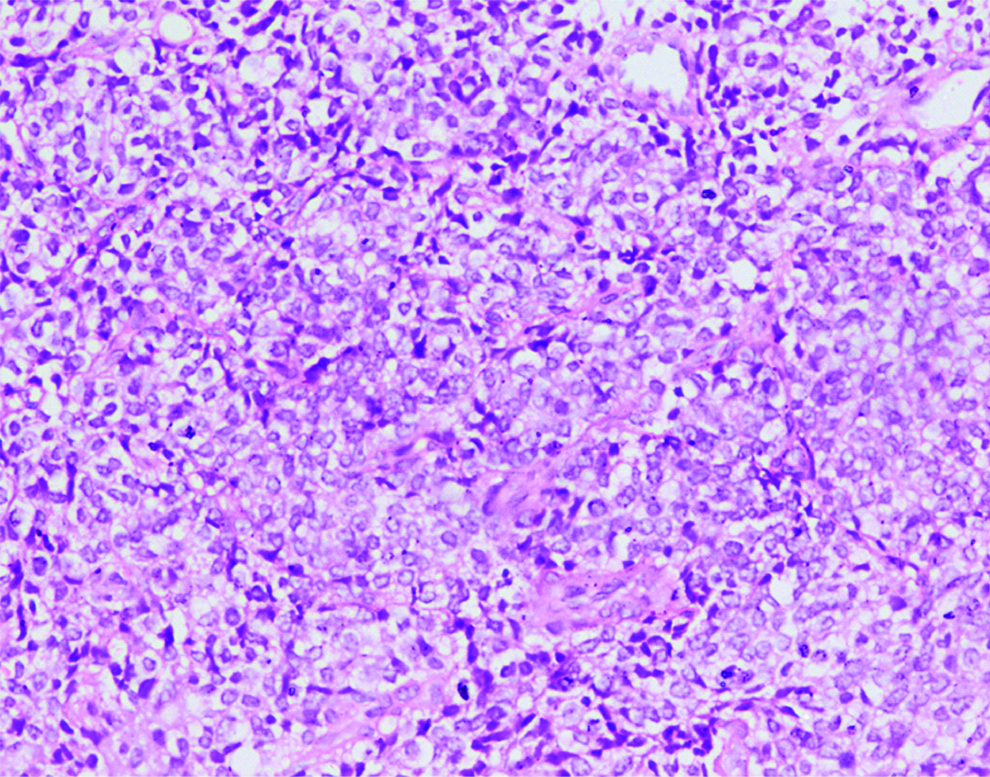
An open biopsy from the fourth metatarsal was obtained. Histopathological examination showed malignant round cell tumour [Table/Fig-4,5]. Tumour was cellular and arranged in sheets and vague lobules separated by thin vascularised fibrous septae. Cells had round nuclei with coarse chromatin and variable amount of finely vacuolated cytoplasm. Mitotic figures were 1-2/HPF. Necrosis was present. Osteoid deposition, rosette formation or giant cells were not seen. Since the tumour was composed of uniform looking round cells, a diagnosis of malignant round cell neoplasm with differential diagnosis of Ewings sarcoma and non-Hodgkin lymphoma of bone were kept in mind. Immuno-histochemistry, as suggested by the pathologist, was vimentin and CD99 (for Ewings sarcoma) and CD 45 (for lymphoma).
Moderately cellular tumour having uniform round to oval nuclei. (H&E;10X).
Tumour cells having round to oval nuclei with fine chromatin and variable amount of cytoplasm (H&E; 40X).
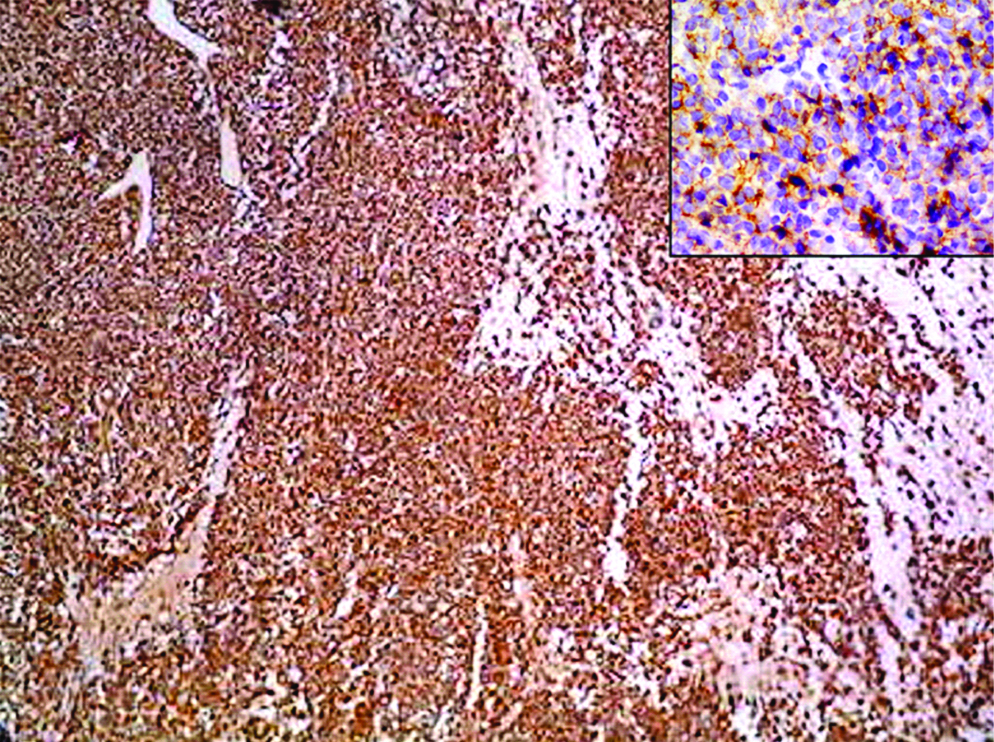
It showed [Table/Fig-6] bright positivity for CD99 and vimentin while cells were negative for pan-cytokeratin, S-100, desmin and SMA (as a routine protocol followed for adolescent round cell tumours) confirming the diagnosis of Ewing’s sarcoma. Patient was seen by an oncologist and neoadjuvant chemotherapy was started. He received vincristine-adriamycin-cyclophosphamide alternate with ifosfamide-etoposide chemotherapy in three weekly schedules. Assessment after four cycles of chemotherapy showed good response and surgical local control was decided. Ray amputation of the left fourth metatarsal was done. Patient was then started-up with adjuvant chemotherapy (same three weekly schedules) with alternate cycles of vincristine-adriamycin-cyclophosphamide and ifosfamide-etoposide and local radiotherapy (54 Gy). He completed his scheduled treatment (total 17 cycles of chemotherapy) and was on follow-up. Patient responded well to chemotherapy. Wounds healed well and he started physiotherapy immediately. He gained full weight bearing privileges within three months and is fully ambulatory now. He was followed up closely for monthly intervals till six months and three monthly intervals subsequently [Table/Fig-7]. He has been disease-free for over 28 months now. No recurrence or relapse has been noted so far.
Strong cytoplasmic positivity on CD99 Immunohistochemistry (IHC; CD99; 4X). Inset image is 40X image with CD99 positivity.
Post-operative X-ray at two months showing complete excision of the involved 4th metatarsal.

Discussion
Ewing’s sarcoma is a rare malignant bone tumour which commonly occurs between 5-20 years of age. It belongs to a class of highly malignant tumours of childhood called primitive neuroectodermal lesions. The essential hallmark of these lesions is small round cell phenotype which they share along with reciprocal translocations between chromosome 11 and 22 [1].
Ewings sarcoma is mainly a diaphyseal lesion, which mostly occurs in the long bones and sometimes involves the flat ones. The incidence of Ewing’s sarcoma in the foot ranges from 1-4% [2]. Our case was classical presentation of Ewing’s sarcoma where there was a permeative lesion with invasion in adjacent soft tissue structures. There were no distant metastases at time of presentation. Absence of distant metastasis and complete resection of lesion should entail good long-term prognosis [3] as was evident in the present case.
There was a good response to chemotherapy and local radiation treatment. Other possibilities in such a scenario are osteomyelitis, cartilaginous tumours, giant cell tumour and osteosarcoma. Differentiation of osteomyelitis from Ewing’s sarcoma is especially difficult due to similar presentation. According to McCarville MB et al., soft tissue mass and non-African ethnicity correspond significantly with Ewings sarcoma when distinguishing from osteomyelitis [4]. The present case too had a large soft tissue component seen both clinically and on MRI which went in its favour of Ewings sarcoma. Vohra VG, performed a study of 156 cases out of which three were of the foot and reported a wide variation in radiographic appearances of Ewings sarcoma and it appeared very similar to osteomyelitis, osteogenic sarcoma, and metastatic deposits [5]. According to Falk S and Alpert M, Tesoro Tess JD, Nessi R., the main difficulty is in distinguishing it from metastatic neuroblastoma, chronic osteomyelitis, and reticulum cell sarcoma [6,7]. Mascard E et al., reported that chondrosarcomas are the most common bony tumours of foot [8]. Other common malignant lesions were osteosarcomas and Ewing’s sarcoma. Prognosis wise they did not find much of difference between them and other groups. For expendable lesions, they recommended intercalary excision followed by chemotherapy. They recommended preservation of first and fifth metatarsal for function if multiple metatarsals are involved. For more proximal lesions, amputations at a suitable level like midfoot or hindfoot or ankle may be desirous. The enhancement pattern after administration of contrast medium on MRI allows differentiation between tumour and peritumoural reactive oedema. Furthermore, MRI can often distinguish the large solid sarcomatous soft-tissue mass around the involved bone from oedema or abscess of osteomyelitis. MRI findings can narrow the differential diagnosis, but a specific diagnosis can rarely be established. Therefore, biopsy of the tumour with histopathological analysis is needed to confirm the diagnosis. MRI should always be performed in the analysis of Ewings sarcoma since it allows accurate evaluation of tumour extent, which is decisive for treatment. Histopathological examination of the lesion is a must in such cases. There is no doubt, that an early recognition of an unusual appearance and location of Ewing’s sarcoma is necessary for its adequate treatment. One should be watchful of this presentation in foot skeleton especially in young patients. Yang P et al., cautioned about doing proper evaluation of non cystic lesions of foot before biopsy [9]. Seven out of eight patients who had intralesional excision of such lesion which turned out malignant on histopathological evaluation had to undergo amputation later on. They concluded that amputation is a respectable outcome in those patients who undergo accidental intra lesional excision [9].
Gupta RP and Mohan V et al., reported two cases of Ewings sarcoma of small bones of hand and feet [10]. Both of these cases masqueraded as acute osteomyelitis from beginning. Results were not favourable in both the cases.
Conclusion
A high index of suspicion should be kept in mind while dealing with a child who has recent onset swellings in his or her small bones of hands and feet. Early diagnosis of this highly malignant neoplasm may entail a favourable outcome.
[1]. Rougraff B, Ewing Sarcoma and Primitive Neuroectodermal Tumour of Bone. In: Torentta Paul, Einhorn TA, Harmon TAOncology and Basic Science 2008 7th EditionLipincott William & Wilkins:188-191. [Google Scholar]
[2]. Sandrasagra FA, Ewing’s sarcoma of a metatarsal boneCeylon Med J 1973 18:58-61. [Google Scholar]
[3]. Wilkins RM, Pritchard DJ, Burgert EO, Unni K, Ewing’s sarcoma of bone: experience with 140 patientsCancer 1986 58:2551-55.10.1002/1097-0142(19861201)58:11<2551::AID-CNCR2820581132>3.0.CO;2-Y [Google Scholar] [CrossRef]
[4]. McCarville MB, Chen JY, Coleman JL, Li Y, Li X, Adderson EE, Distinguishing osteomyelitis from ewing sarcoma on radiography and MRIAJR Am J Roentgenol 2015 205(3):640-50.10.2214/AJR.15.1434126295653 [Google Scholar] [CrossRef] [PubMed]
[5]. Vohra VG, Roentgen manifestations in Ewing’s sarcomaCancer 1967 20(5):727-33.10.1002/1097-0142(1967)20:5<727::AID-CNCR2820200525>3.0.CO;2-B [Google Scholar] [CrossRef]
[6]. Falk S, Alpert M, The clinical and roentgen aspects of Ewing’s sarcomaAm J Med Sci 1965 250(5):493-508.10.1097/00000441-196511000-000025846029 [Google Scholar] [CrossRef] [PubMed]
[7]. Tesoro Tess JD, Nessi R, Late metastasis from neuroblastoma mimicking Ewing’s sarcomaPediatr Radio 1980 10(2):107-09.10.1007/BF01001750 [Google Scholar] [CrossRef]
[8]. Mascard E, Gaspar N, Brugières L, Glorion C, Pannier S, Gomez-Brouchet A, Malignant tumours of the foot and ankleEFORT Open Rev 2017 2(5):261-71.10.1302/2058-5241.2.16007828630763 [Google Scholar] [CrossRef] [PubMed]
[9]. Yang P, Evans S, Bali N, Ramasamy A, Evans R, Stevenson J, Jeys L, Malignant bone tumours of the footAnn R Coll Surg Engl 2017 99(7):568-72.10.1308/rcsann.2017.011428853588 [Google Scholar] [CrossRef] [PubMed]
[10]. Gupta RP, Mohan V, Ewing’s sarcoma of the small bones of hands and feetInd J Rad & Img 2002 12(3):403-05. [Google Scholar]