Case Report
A 63-year-old male patient reported to the department of oral medicine with the chief complaint of painless growth in his left side cheek region for past six months which was smaller in size and gradually increased to the present size following a traumatic injury. On general examination, the patient was hypertensive and under medication for past two years. On physical examination, the patient was moderately built and well-nourished with no abnormalities in the trunk and extremities.
Extra oral examination of head and neck region demonstrated [Table/Fig-1] a symmetrical facial configuration, no abnormal sensation or motor palsy of the cheek, and no significant cervical lymphnode enlargement.
Extra oral photograph of the patient.

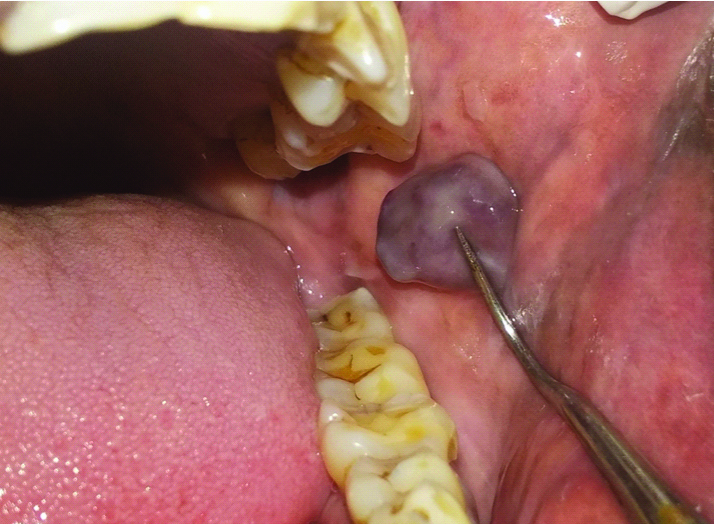
Intra oral examination of the growth demonstrated [Table/Fig-2,3] a solitary, well-defined, bluish black coloured pedunculated, lobulated growth roughly measuring about 3×2 cm in dimension, with whitish area evident surrounding the growth on the left buccal mucosa along the occlusal plane and not attached to the underlying tissue. The growth extends anteriorly approximately 4 cm away from the commisure of lip, and 1 cm away from the retromolar region posteriorly, supero-inferiorly 3 cm away from upper and lower buccal vestibule respectively. The growth was soft to firm in consistency, non-tender on palpation, freely movable, superior aspect of the growth appears to be mildly hyperpigmented, no blanching test was done as the growth presents as a pedunculated mass separated from the underlying structures with surrounding whitish area which might be due to repeated trauma or friction with no evidence of secondary change.
Intra oral picture showing a single, well-defined growth.
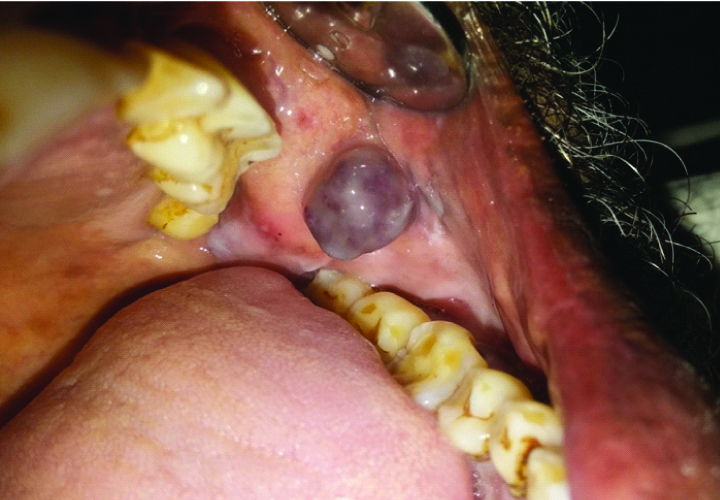
Intra oral picture showing a single, well-defined pedunculated, lobulated growth.
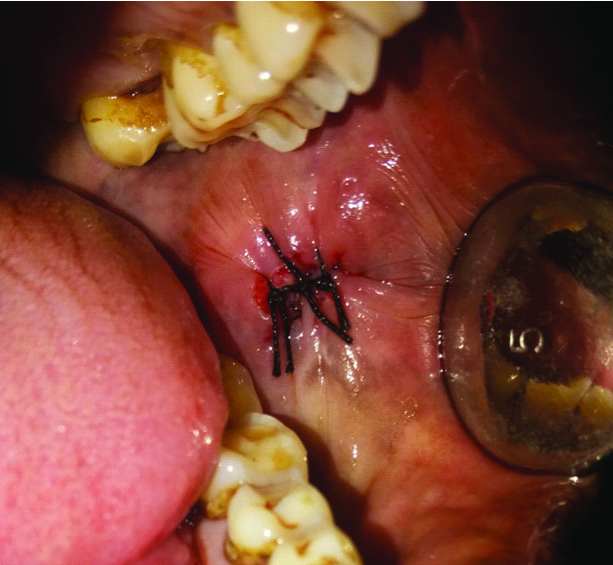
Based on the patient’s history and clinical examination the provisional diagnosis of Traumatic Fibroma was given, along with a differential diagnosis of Fibroepithelial polyp, Haemangioma, Lipoma, Granulofibroma, Mucocele. The growth was surgically excised with the patient’s consent under local anaesthesia with no complications and post-operative instructions were given and the patient was kept under follow-up [Table/Fig-4]. Since the mass was pedunculated, surrounded by a thin capsule and was not adherent to the underlying structures, excision was facile. In the follow-up period of six months, there was no evidence of recurrence upto the third review visit [Table/Fig-5].
Intra oral picture showing excision of the growth with sutures placed.
Intra oral review picture of the surgical site.

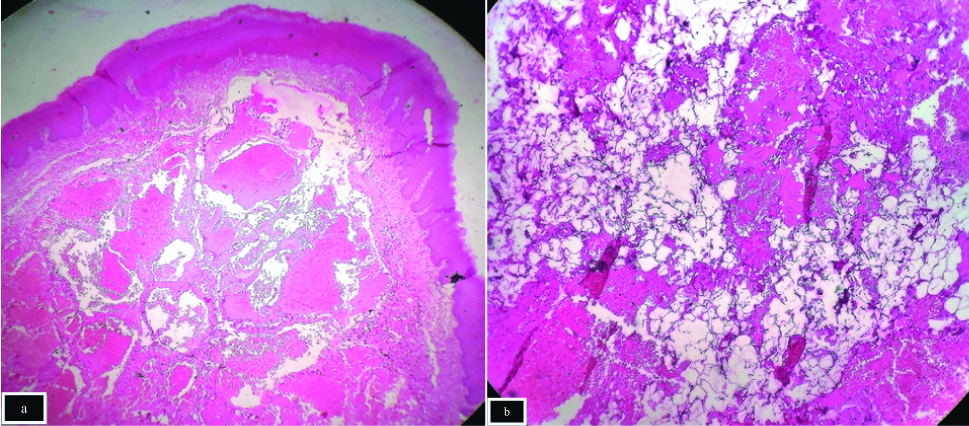
Macroscopic [Table/Fig-6a,b] examination revealed a single soft tissue specimen measuring approximately about 1.4×1×1 cm in size, roughly ovoid in shape, smooth to rough surface, firm in consistency, and cream to dark brown in colour.
The excised specimen measuring 1.4×1×1 cm in size.

Microscopically [Table/Fig-7a,b], H&E stain was done and viewed under microscopic magnification of both X100 [Table/Fig-7a] and X400 [Table/Fig-7b], in which, the encapsulated mass presented with an epithelium and connective tissue component. The epithelium was hyperplastic exhibiting basilar hyperplasia, acanthosis and hyperparakeratosis. The underlying connective tissue showed larger vascular spaces lined by thin endothelium and engorged with RBC’s and in some areas mature adipocytes were interspersed with vessels. There was also evidence of capillary sized vessels, few chronic inflammatory cells, extravasated RBC’s and muscle fibres. And histopathological diagnosis was given as Non-Infiltrating type of Angiolipoma.
(a(X100), b(X400)) - The histopathological picture showing mature adipocytes arranged in sheets separated by thin fibrous connective tissue with interspersed vessels.
Discussion
Bowen JT in 1912 reported the first case of Angiolipoma, a subtype of lipoma [1]. Angiolipomas are usually multiplex and can occur at any age, with a mean age of 48 years (9-76), with a slight male predilection, a ratio of 6:5 male to female [2]. Angiolipomas are chiefly composed of mature adipocytes with proliferating vascular endothelial cells. They are classified into non-infiltrating and infiltrating category based on their histological demonstration [2,3].
A theory was proposed by Howard WR et al., wherein the pathogenic mechanism of the formation of lipoma caused by adolescent hormones which was subsequently stimulated by trauma or irritation, eventually lead to angioproliferation in the lipoma [2]. Based on the literature, a theory that AL originates as a congenital lipoma, which later undergoes vascular proliferation was given. Howard WR et al., thought that embryonic sequestration of multipotential cells becomes active at puberty by hormones and differentiate into a simple lipoma, however with added stimuli such as trauma can lead to vascular infiltration of the lesion, though trauma is not present in many cases of AL [2]. Davis GB et al., reported the first Angiolipoma in the oral cavity as a tumour occurring in the hard palate [4].
A total of 28 cases (1976-2018) inclusive of present case were revealed on Angiolipoma in oral soft tissues [Table/Fig-8] [4-30]; therefore, showcasing the rarity of angiolipoma with a prevalence rate of 6-7% of all lipomas with 2-4% of non-infiltrating angiolipoma [17].
Literature review of angiolipoma in the oral cavity and their sites (1976-2018) [4-30].
| S.No | Authors | Year | Site |
|---|
| 1 | Davis GB et al [4] | 1976 | Hard palate |
| 2 | Weitzner S et al [5] | 1978 | Cheek |
| 3 | Campos GM [6] | 1980 | Cheek |
| 4 | Brahney CP [7] | 1981 | Tongue |
| 5 | Flaggert 3rd JJ [8] | 1986 | Hard palate |
| 6 | Junko Sugiura et al [9] | 1999 | Mucolabial fold |
| 7 | Lin SC et al [10] | 1986 | Tongue |
| 8 | Sanchez Aniceto G et al [11] | 1990 | Cheek |
| 9 | Koizumi K et al [12] | 1992 | Cheek |
| 10 | Ali MH et al [13] | 1996 | Cheek |
| 11 | Takahashi M et al [14] | 1998 | Tongue |
| 12 | Alvi A et al [15] | 1998 | Cheek |
| 13 | Hamakawa H et al [16] | 2000 | Cheek |
| 14 | Mochida C et al [24] | 2005 | Cheek |
| 15 | Ida-Yonemochi H [20] | 2005 | Cheek |
| 16 | Park JY et al [25] | 2008 | Floor of the mouth |
| 17 | Altug H A et al [18] | 2009 | Cheek |
| 18 | Arenaz Bua J et al [26] | 2010 | Cheek |
| 19 | Studart-Soares E C et al [27] | 2010 | Retromolar area |
| 20 | Yanase S et al [17] | 2011 | Buccal mucosa |
| 21 | Palaia G et al [28] | 2011 | Cheek |
| 22 | Sah K et al [29] | 2012 | Upper lip |
| 23 | Silva Junior G O et al [19] | 2013 | Pterygomandibular raphae |
| 24 | Mohiuddin SA et al [30] | 2014 | Buccal vestibule |
| 25 | Ajoy Kumar Shahi et al [23] | 2014 | Cheek |
| 26 | Chandrashekaran D et al [21] | 2016 | Hard palate |
| 27 | Sanat Kumar Bhuyan [22] | 2017 | Floor of the mouth |
| 28 | A Hari Priya et al (current study) | 2018 | Buccal mucosa |
Frequently involved regions of non-inflitrating angiolipoma of oral cavity are cheek, tongue, palate, lip, chin and buccal mucosa. Out of all the 28 cases only 2 cases have been reported in the buccal mucosa including this case. In contrast to lipoma, Angiolipoma in the oral cavity does not correlate with family history or multiple onsets.
Histologic guidelines for diagnosis of AL are based on the following criteria [22]:
Well-encapsulated (non-infiltrating ALs) or poorly encapsulated (infiltrating ALs).
(a) Encapsulated tumour mass consisting of mature adipose tissue intermixed with blood vessel (H&E stain, X100 view); (b) Sheets of mature adipose tissue with vascular component showing no cellular atypia (H&E stain, X400) [Table/Fig-7a,b].
Evidence of 50% mature adipocytes in the tumour.
Interspersed angiomatous proliferation in the tumour.
Fibrinous micro-thrombi.
Absence of other mesenchymal elements (smooth muscle) or pleomorphism.
Lipoma is a benign mesenchymal tumour composed primarily of mature adipocytes with a thin fibrous capsule separating it from the surrounding tissues. One of the aetiological factors of lipoma is said to be trauma though the actual aetiology is still a mystery with an incidence rate of 15-20% in head and neck region of which 1-4% occurs in the oral cavity including the various types of lipoma such as osteolipoma, myolipoma, hamartomatous lesions, diffuse lipomatous proliferation and hibernoma. Mature lipocytes are formed by differentiation of pre-adipocytes which are forms of undifferentiated fibroblasts. Based on their histopathologic appearance they are subclassified into Angiolipoma, Spindle cell lipoma, Myelolipoma, Chondrolipoma and Myxolipoma which are some of the logical variants of lipoma [31].
Fibromas are benign connective tissue tumour. They habitually occur in response to irritation from local trauma, the most commonly affected regions in oral cavity are buccal mucosa and tongue. Chief characteristics include asymptomatic, dome-shaped, smooth surfaced, sessile or pedunculated masses resembling as in present case, with female predilection between 20-50 years of age with an average size of 0.5 to 1.5 cm, and predominantly made up of collagen fibers in histopathological investigation. These features were absent in this case [32].
Fibro-Epithelial Polyps (FEP) are small round knob-like outgrowths found anywhere on mucosa but are most commonly seen on tongue, lips and cheek along the occlusal line. They present as solitary, firm, pink, painless, sessile or pedunculated, polypoid swelling with varying size which range in a few millimeters as was presented in this case, but histopathologically composed of numerous fibrous stroma covered by a non-papillary layer of hyperplastic squamous epithelium differing from this case [33].
Haemangioma is a common soft tissue tumour. Sites commonly involved are gingiva, palatal mucosa, lips, jawbone, and salivary glands. Clinically they present as lobulated, pedunculated, red to purple in colour, hormone-sensitive representing the present case. Histopathological presentation exhibit progression from a densely cellular proliferation of endothelial cells in the early stages to a well-defined lobular mass composed of capillaries in the mature phase, often resembling the pyogenic granuloma without the inflammatory features altering from the presented case [34].
Oral pyogenic granuloma is a type of reactive hyperplasia of connective tissue, a tumour-like growth with slight female predilection. Affected sites are the gingiva followed by lips, tongue, buccal mucosa, and hard palate. They appear as soft, painless, sessile lesion to an elevated mass with deep red to reddish-purple in colour as in this case. The histopathological presentation includes increased vascular proliferation of granulation tissue engorged with red blood cells lined by basal flat or plump endothelial cells and separated by less vascular septa contradicting from current case [35].
Oral Mucocele, a benign minor salivary gland swelling caused mostly due to mechanical trauma to the excretory duct of the gland. Characterised clinically, as single or multiple soft, fluctuant nodule, ranging from the normal colour of the oral mucosa to deep blue demonstrated as in this case. Frequently involved locations are lip, palate, retromolar region, buccal mucosa, lingual frenum, dorsal surface of tongue. The histopathological characteristics include acute inflammation intermingling with mucous collection to patterns of mature lesions with scarce amounts of mucous and connective tissue fibrosis in contrast to this case [36].
Histopathological investigation remains the gold standard for definite diagnosis of these lesions. Other methods include MRI, CT, sonography and aspiration biopsy to distinguish between haemangioma, lipoma and AL. Differences in the percentages of adipose and vascular components among individuals make definite diagnosis of ALs difficult. In the present case, a clinical diagnosis of fibroma was given based on the history and clinical features, but histopathologically the lesion was reported as AL.
In the case presented, the growth was found to be a non-infiltrating angiolipoma on the left buccal mucosa, which was surgically excised with neither any complications nor any evidence of remission in a period of six months.
Conclusion
Hence, a thorough understanding of the lesion is required before preceding the treatment in case of AL. A complete surgical excision without involving the surrounding structures is the appropriate treatment for non-infiltrating AL as was done in this case, whereas in case of infiltrating AL in the absence of capsule, excision of the surrounding structures is recommended. Malignant transformation and recurrence of AL in the oral region have been none with an average follow-up period of 17.5 months as been reported till date. With the presence of a capsule expressing the low proliferative capacity of non-infiltrating AL, as in this case, though recurrence and malignant transformation can be least expected, the patient still needs to be kept under continuous follow-up.
[1]. Bowen JT, Multiple subcutaneous hemangiomas, together with multiple lipomas, occurring in enormous numbers in an otherwise healthy, muscular subjectAm J Med Sci 1912 144:189-92.10.1097/00000441-191208000-00003 [Google Scholar] [CrossRef]
[2]. Howard WR, Helwig EB, AngiolipomaArch Dermatol 1960 82:924-31.10.1001/archderm.1960.0158006007801113716236 [Google Scholar] [CrossRef] [PubMed]
[3]. Lin JJ, Lin F, Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipomaCancer 1974 34:720-27.10.1002/1097-0142(197409)34:3<720::AID-CNCR2820340331>3.0.CO;2-K [Google Scholar] [CrossRef]
[4]. Davis GB, Stoelinga PJ, Tideman H, Bronkhorst F, Angiolipoma of the hard palate: a case report and review of the literatureJ Maxillofacial Surg 1976 4:242-44.10.1016/S0301-0503(76)80046-X [Google Scholar] [CrossRef]
[5]. Weitzner S, Moynihan PC, Angiolipoma of the cheek in a childOral Surg Oral Med Oral Pathol 1978 45:95-97.10.1016/0030-4220(78)90229-3 [Google Scholar] [CrossRef]
[6]. Campos GM, Grandini SA, Lopes RA, Angiolipoma of the cheekInt J Oral Surg 1980 9:486-90.10.1016/S0300-9785(80)80082-2 [Google Scholar] [CrossRef]
[7]. Brahney CP, Aria AA, Koval MH, Najjar TA, Angiolipoma of the tongue: report of case and review of literatureJ Oral Surg 1981 39:451-53. [Google Scholar]
[8]. Flaggert 3rd JJ, Heldt LV, Keaton WM, Angiolipoma of the palate. Report of a caseOral Surg Oral Med Oral Pathol 1986 61:333-36.10.1016/0030-4220(86)90412-3 [Google Scholar] [CrossRef]
[9]. Junko Sugiura, Kouji Fujiwara, Izuru Kurahashi, Yoshitaka Kimura, Infiltrating angiolipoma of the mucolabial fold: A case report and review of the literatureJ Oral Maxillofac Surg 1999 57:446-448.10.1016/S0278-2391(99)90287-2 [Google Scholar] [CrossRef]
[10]. Lin SC, Wang TY, Hahn LJ, Angiolipoma of the tongue: report of a caseAnn Dent 1989 48:37-38. [Google Scholar]
[11]. Sánchez Aniceto G, Salván Saez R, García Peñin A, Angiolipoma of the cheek: report of a caseJ Oral Maxillofac Surg 1990 48:512-15.10.1016/0278-2391(90)90243-U [Google Scholar] [CrossRef]
[12]. Koizumi K, Shirasuna K, Okura M, Yoshioka H, Matsuya T, Angiolipoma of the cheekJpn J Oral Maxillofac Surg 1992 38:1224-25.10.5794/jjoms.38.1224 [Google Scholar] [CrossRef]
[13]. Ali MH, el-Zuebi F, Angiolipoma of the cheek: report of a caseJ Oral Maxillofac Surg 1996 54:213-15.10.1016/S0278-2391(96)90450-4 [Google Scholar] [CrossRef]
[14]. Takahashi M, Kurokawa H, Ando T, Sato Y, Noguchi I, A case of angiolipoma of the tongue in a childJpn J Oral Maxillofac Surg 1998 44:817-19.10.5794/jjoms.44.817 [Google Scholar] [CrossRef]
[15]. Alvi A, Garner C, Thomas W, Angiolipoma of the head and neckJ Otolaryngol 1998 27:100-03. [Google Scholar]
[16]. Hamakawa H, Hino H, Sunida T, Tanioka H, Infiltrating angiolipoma of the cheek: a case reportJ Oral Maxillofac Surg 2000 58:674-77.10.1016/S0278-2391(00)90166-6 [Google Scholar] [CrossRef]
[17]. Shigeaki Yanase, Jouji Nomura, Yoshihiko Matsumura, Hideharu Kato, Takashi Takeoka, Hiroko Imura, Angiolipoma of the cheek: A case report with a literature reviewAsian Journal of Oral and Maxillofacial Surgery 2011 23:35-37.10.1016/j.ajoms.2010.09.002 [Google Scholar] [CrossRef]
[18]. Hasan Ayberk Altuğ, Sermet Sahin, Metin Sencimen, Necdet Dogan, Ozgur Erdogan, Non-infiltrating angiolipoma of the cheek: a case report and review of the literatureJournal of Oral Science 2009 Vol. 51(No. 1):137-139.10.2334/josnusd.51.13719325211 [Google Scholar] [CrossRef] [PubMed]
[19]. Silva-Junior GO, Picciani BL, Costa RC, Barbosa SM, Silvares MG, Oral soft tissue angiolipoma-Report of two cases of rare oral lipomatous lesion with emphasis on morphological and immunohistochemical featuresJournal of Oral Science 2013 55(1):85-88.10.2334/josnusd.55.85 [Google Scholar] [CrossRef]
[20]. Ida-Yonemochi H, Swelam W, Saito C, Saku T, Angiolipoma of the buccal mucosa: A possible role of mast cell-derived VEGF in its enhanced vascularityJ Oral Pathol Med 2005 34:59-61.10.1111/j.1600-0714.2004.00230.x15610409 [Google Scholar] [CrossRef] [PubMed]
[21]. Chanrasekaran D, Swami RDC, Simhan MN, Kumar AEN, Natarajan PS, Non infiltrating angiolipoma of the palate in geriatric patient: A Case report with review of literatureJ Clin Diagn Res 2016 10(1):ZD01-ZD02.10.7860/JCDR/2016/16634.703227014643 [Google Scholar] [CrossRef] [PubMed]
[22]. Bhuyan SK, Bhuyan R, Debta P, Mohandebta F, Non-infiltrating angiolipoma of floor of mouth-a rare case report and literature reviewJournal of Clinical and Diagnostic Research 2017 11(2):ZD03-ZD05.10.7860/JCDR/2017/22407.896428384985 [Google Scholar] [CrossRef] [PubMed]
[23]. Shahi AK, Ash H, Chatterji K, Singh R, Cellular infiltrative angiolipoma of cheek in an infantNatl J Maxillofac Surg 2014 5(2):202-05.10.4103/0975-5950.15483725937736 [Google Scholar] [CrossRef] [PubMed]
[24]. Mochida C, Sumitani K, Nemoto T, Maeda Y, Tachikawa T, Nagumo M, A case of angiolipoma of the cheekJpn J Oral Maxillofac Surg 2005 51:360-63.10.5794/jjoms.51.360 [Google Scholar] [CrossRef]
[25]. Park JY, Yoon YH, Rha KS, Koo BS, A case of angiolipoma of floor of mouthKorean Journal of Otolarynologology Head and Neck Surgry 2008 51(4):399-401. [Google Scholar]
[26]. Yanase Arenaz Búa J, Luáces R, Lorenzo Franco F, García-Rozado A, Crespo Escudero JL, Fonseca Capdevila E, Angiolipoma in head and neck: Report of two cases and review of the literatureInt J Oral Maxillofac Surg 2010 39:610-5.10.1016/j.ijom.2009.12.02120197228 [Google Scholar] [CrossRef] [PubMed]
[27]. Studart-Soares EC, Gurgel Costa FW, Bitu Sousa F, Negreiros-Nunes Alves AP, Verde Osterne RL, Oral lipomas in a Brazilian population: A 10-year study and analysis of 450 cases reported in the literatureMed Oral Patol Oral Cir Bucal 2010 15:e691-96.10.4317/medoral.15.e69120383107 [Google Scholar] [CrossRef] [PubMed]
[28]. Palaia G, Giamari G, Giudice R, Galankis A, Tenore G, Romeo U, Excision of oral angilipoma by ktp laser a case reportAnnals Di Stomatologia 2011 (1-2):28-31. [Google Scholar]
[29]. Sah K, Kadam A, Sunita JD, Chandra S, Non-infiltrating angiolipoma of the upper lip: A rare entityJ Oral Maxillofac Pathol 2012 16(1):103-06.10.4103/0973-029X.9298322438649 [Google Scholar] [CrossRef] [PubMed]
[30]. Mohiuddin SA, Badal S, Doiphode A, Sulatana S, Noninfiltrating intraoral angiolipoma in the mandibular buccal vestibuleJournal of Oral Sciences 2014 5(1):33-34.10.4103/0976-6944.129948 [Google Scholar] [CrossRef]
[31]. El-Momen MH ABD, Gaafar AH, Magdy EA, Lipomas of the head and neck: presentation variability and diagnostic work-upJ Laryngol Otol 2006 120(1):47-55.10.1017/S002221510500459716359147 [Google Scholar] [CrossRef] [PubMed]
[32]. Panta P, Traumatic fibromaPan Afr Med J 2015 21:22010.11604/pamj.2015.21.220.749826448815 [Google Scholar] [CrossRef] [PubMed]
[33]. Koppolu P, Mishra A, Kalakonda B, Swapna LA, Bagalkotkar A, Macha D, Fibroepithelial polyp excision with laser and scalpel: A comparative evaluationInt J Curr Microbiol App Sci 2014 3(8):1057-62. [Google Scholar]
[34]. Sobhana CR, Beena VT, Soni A, Choudhary K, Sapru D, Hemangiolymphangioama of buccal mucosa: Report of a rare case and review of literature on treatment aspectNatl J Maxillofac Surg 2012 3(2):190-94.10.4103/0975-5950.11137923833496 [Google Scholar] [CrossRef] [PubMed]
[35]. Kamal R, Dahiya P, Puri A, Oral pyogenic granuloma: Various concepts of etiopathogenesisJ Oral Maxillofac Pathol 2012 16(1):79-82.10.4103/0973-029X.9297822434943 [Google Scholar] [CrossRef] [PubMed]
[36]. More CB, Bhavsar K, Varma S, Tailor M, Oral mucocele: A clinical and histopathological studyJ Oral Maxillofac Pathol 2014 18(Suppl 1):S72-S77.10.4103/0973-029X.14137025364184 [Google Scholar] [CrossRef] [PubMed]