Filarial Pleural Effusion with Lymphoma: A Rare Association
Kiran Agarwal1, Aruna Chhikara2
1 Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
2 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aruna Chhikara, Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi-110001, India.
E-mail: arunachhikara123@gmail.com
Filariasis is endemic in developing countries with highest prevalence in India. Microfilarias are infrequently reported during cytological examination of body cavity fluids. Its association with neoplasm is still rare, with only a few reported cases of co-existent microfilaria with neoplasm. The malignancies reported in association with malignant pleural effusions are mostly carcinomas. Finding microfilaria in a pleural effusion is a very rare event even in the regions endemic for this organism. Its association with a lymphoma is even rarer. On extensive search of literature we could not find any case report of filarial pleural effusion associated with lymphoma. We here report a case of microfilaria in malignant pleural effusion secondary to lymphoma.
Effusion fluid, Lymphoblastic lymphoma, Microfilaria
Case Report
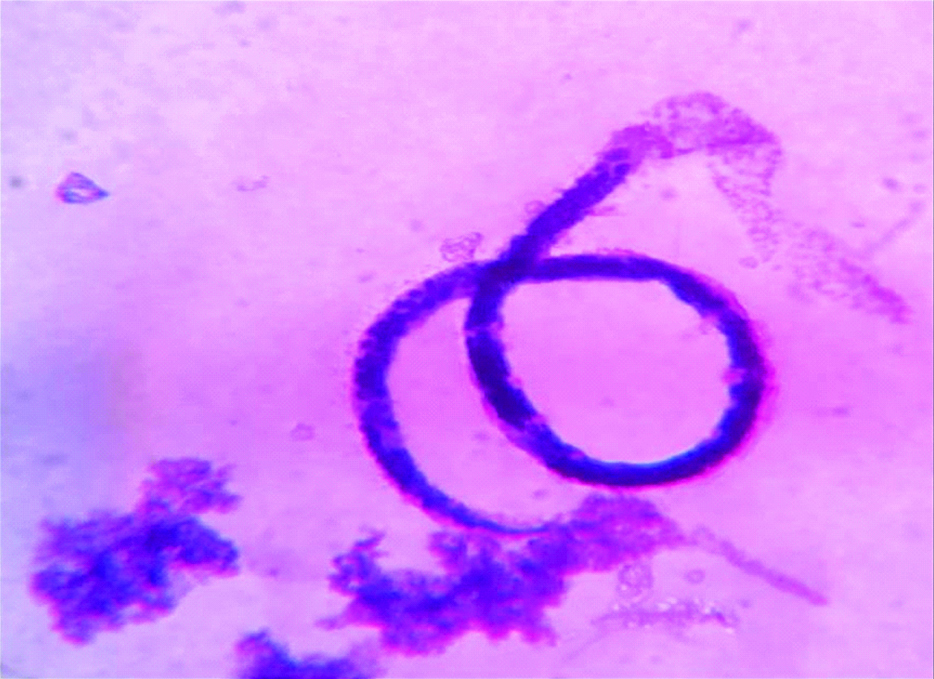
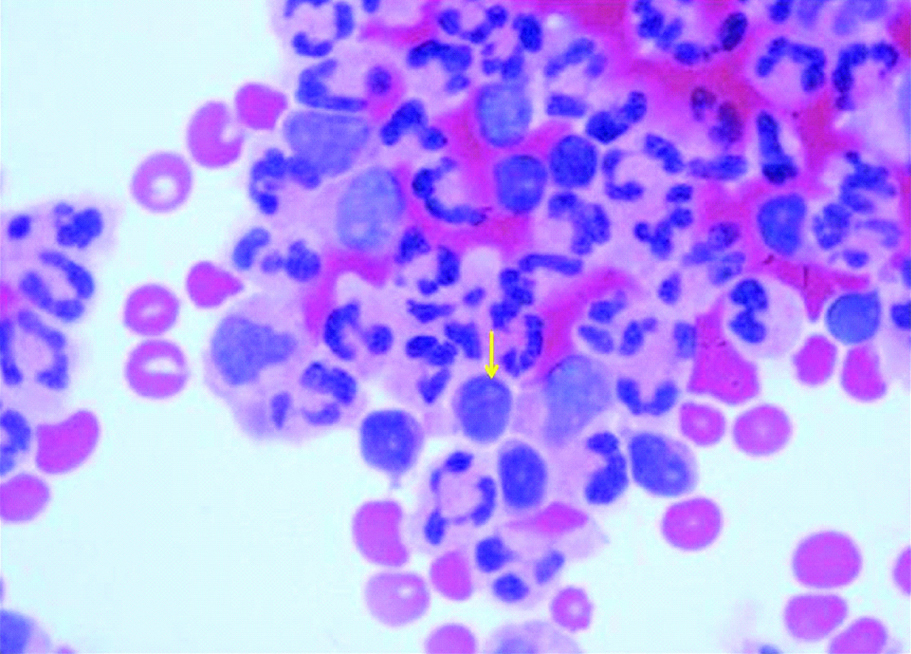
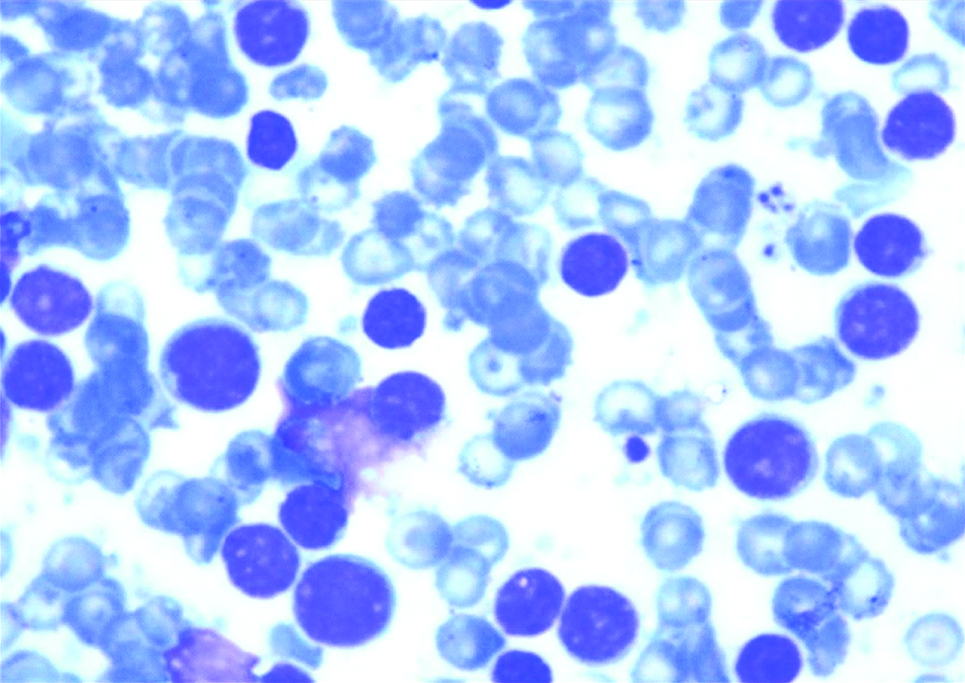
A six-year-old female presented with anterior chest wall lump, fever and weight loss for three months. On examination the child looked cachexic with facial puffiness and prominent veins over abdomen and chest, but was otherwise stable. No significant past history was present. A swelling measuring 5×3 cm was noted on chest. The X-ray chest showed bilateral pleural effusion and pericardial effusion. The ultrasonography of local parts showed a 5×2 cm heterogeneously hypoechoeic lesion, suggestive of a cold abscess. The CT (Radiological images are unavailable as the patient was referred from other center) chest showed mass lesion in mediastinum with bilateral pleural effusion with pericardial effusion, suggestive of Non Hodgkin’s Lymphoma with superior vena cava syndrome (due to compression by mediastinal mass). The ESR was 30 mm in 1st hour. Peripheral blood examination and bone marrow aspirate examination was normal. Blood culture was sterile. Workup for tuberculosis was negative. We received pleural fluid for cytology. The fluid was haemorrhagic. Biochemically, it was an exudative effusion with lymphoid cells constituting 48%. The cytological smear showed a sheathed organism, with lack of nuclei at the tail end, morphologically consistent with Wuchereria bancrofti [Table/Fig-1], along with acute and chronic inflammatory exudate and few cells showing high nuclear to cytoplasmic ratio, scant agranular cytoplasm and irregular nuclear membrane [Table/Fig-2]. The ultrasound guided aspirates and trucut biopsy were performed from the mediastinal mass. The cytological smears were cellular showing clustered as well as dispersed population of medium sized cells. The cells had scant cytoplasm with high nuclear to cytoplasmic ratio, scant amount of agranular cytoplasm and round to oval nucleus, few of which showed indentation. The nucleus of these cells had fine chromatin with 0-1 nucleoli [Table/Fig-3]. Based on morphological findings a possibility of Non Hodgkin’s lymphoma, most likely acute lymphoblastic lymphoma was suggested and histopathological and immunohistochemical examination was advised for confirmation and typing.
Microfilaria in cytospin smears of pleural effusion (MGG, 400X).
Pleural effusion smears showing few malignant cells with acute inflammatory infiltrate (MGG, 400X).
Lymphoblasts in fine needle aspiration smears from mediastinal mass (MGG, 400X).
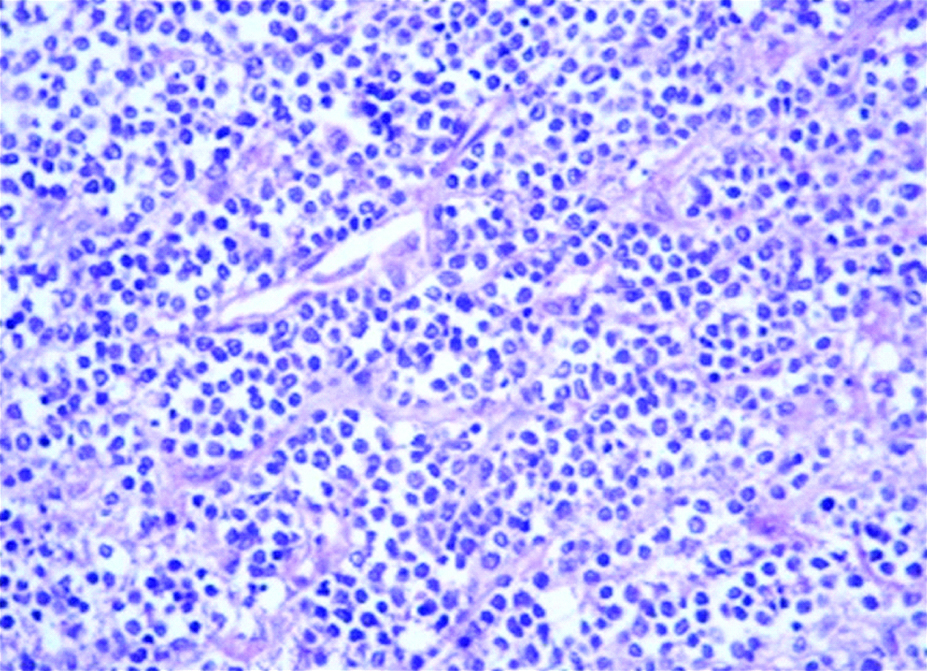
The histopathological sections from incisional biopsy of mediastinal mass also showed a monomorphous population of medium sized cells with high nucleus to cytoplasmic ratio, scant agranular cytoplasm, round to oval nucleus showing mild anisonucleosis. The chromatin was fine with 0-1 nucleoli [Table/Fig-4]. On immunohistochemistry, these cells were positive for tdt, CD3, CD5 and negative for CD20 and CK. Based on morphological examination and immunohistochemistry, a diagnosis of T cell Acute Lymphoblastic Lymphoma was made. The bone marrow aspirate of the patient did not show any malignant cells. The patient was started on treatment for microfilaria in form of diethyl carmazapine 1 mg/kg PO and chemotherapy for T cell ALL using CHOP regime. The patient became sick and was lost after two days of starting the therapy and eventually expired.
Monomorphous population of medium sized cells (H&E, 100X).
Discussion
Lymphatic filariasis is common in tropical countries and is endemic in India, especially along the sea coasts and river banks [1,2]. Filariasis has a variable presentation. Filarial lung involvement is usually present in form of tropical pulmonary eosinophilia with pulmonary infiltrates and eosinophilia in peripheral blood. Filariasis presenting with pleural effusion is an unusual presentation [1,3]. It is very rare to find malignancy in association with filarial pleural effusion and the role of filariasis in such scenarios is controversial.
Filariasis is a major health problem in India [2,4]. It is endemic in the states along the sea coasts and river banks [4,5]. W. bancrofti is the most common species of filaria from lymph nodes, subcutaneous nodules, breast, and hydrocele fluid etc. However, pleural effusion is an uncommon manifestation [2,5,6]. Filarial pleural effusion occurs due to immunological reaction against filarial antigen, lymphangitis, and incomplete lymphatic obstruction [3,6]. Association of microfilaria with debilitating conditions suggests that it may be an opportunistic infection or it may be coincidental finding with various neoplasms [7-11]. In present case pleural effusion was nonchylous exudative type showing microfilariae of species W. bancrofti and few malignant cells. Besides pleural effusion the patient also had lymphoma presenting as mediastinal mass.
Filariasis is endemic in India and, therefore, the coexistence of filariasis with pleural effusion is more likely to be coincidental rather than aetiological. Gupta K et al., reported six cases where microfilariae were found in body fluid cytology and fine needle aspiration smears in association with tubercular pleural effusion/lymphadenitis, pregnancy, non-Hodgkin’s lymphoma, (The type of NHL is not mentioned in the article by the authors) malnutrition and young age [7]. In the current case report microfilaria could be considered as an opportunistic infection. The coexistent debilitating condition lowers the host immunity, leading to manifestations of symptoms secondary to microfilaria infestation [12] or microfilaria maybe an opportunistic in such patients [7]. There is no data suggesting the role of microfilaria in causing malignancy in literature. However there are increasing reports of filaria seen in association with malignancy. Hence, all cases of filarial pleural effusion must be workup up to rule out malignancy. The present case had microfilaria in pleural effusion, along with T cell Acute Lymphoblastic Lymphoma, suggesting presence of microfilaria as an opportunistic infection. Filariasis in pleural fluid is rare. The rarity of present case is all the more unique due to its association with concomitant lymphoma.
Conclusion
In idiopathic cases of pleural effusion from endemic (as well as non-endemic) areas microfilaria infestation should be considered in the differential diagnosis. In cases of recurrent effusion, tuberculosis and malignancy should be considered first, but filarial infestation should also be ruled out in such cases. The association of filariasis with malignancies may be an incidental finding or malignancy might be a predisposing factor for filarial infestation. Hence, all cases with filarial effusions should also be worked up to rule out malignancy.
[1]. Marathe A, Handa V, Mehta GR, Mehta A, Shah PR, Early diagnosis of filarial pleural effusionIndian J Med Microbiol 2003 21:207-08. [Google Scholar]
[2]. Navaz AK, Raikar MP, Acharya V, Shetty SK, Pleural effusion: An unusual cause and associationLung India 2013 30:158-60.10.4103/0970-2113.11043123741100 [Google Scholar] [CrossRef] [PubMed]
[3]. Arora VK, Gowrinath K, Pleueral effusion due to lymphatic filariasisIndian J Chest Dis Allied Sci 1994 36:159-61. [Google Scholar]
[4]. Garg R, Sodhi R, Jabeed P, Rastogi A, Nonresolving pleural effusion in an elderly woman: A case reportAnn Thorac Med 2010 5:247-48.10.4103/1817-1737.6911820981187 [Google Scholar] [CrossRef] [PubMed]
[5]. Menon B, Garg A, Kalra H, Sharma R, Microfilarial pleural effusion in a case of tropical pulmonary eosinophiliaIndian J Chest Dis Allied Sci 2008 50:241-43. [Google Scholar]
[6]. Singh SK, Pujani M, Pujani M, Microfilaria in malignant pleural effusion: An unusual associationIndian J Med Microbiol 2010 28:392-94.10.4103/0255-0857.7183320966579 [Google Scholar] [CrossRef] [PubMed]
[7]. Gupta K, Sehgal A, Puri MM, Sidhwa HK, Microfilariae in association with other diseases. A report of six casesActa Cytol 2002 46:776-78.10.1159/00032699612146052 [Google Scholar] [CrossRef] [PubMed]
[8]. Premi HS, Samaga BN, Subramanyam K, Shetty JK, Teerthanath S, Baikunje V, Microfilaria in pericardial effusion coexisting with spindle cell thymoma-A rare case reportNitte University J Health Sci 2011 1:40-42. [Google Scholar]
[9]. Jaiswal S, Chand G, Lal H, Vij M, Pandey R, Microfilaria in association with adrenal lymphoma diagnosed on cytology: An extremely rare case reportTurk Patoloji Derg 2013 29(2):143-45.10.5146/tjpath.2013.0116623661353 [Google Scholar] [CrossRef] [PubMed]
[10]. Chordiya AP, Datar S, Agrawal AK, Gadkari RU, Shrikhande AV, Microfilaria in malignant pleural effusion: An unusual incidental finding or causative association?Int J Res Med Sci 2015 3(10):2889-991.10.18203/2320-6012.ijrms20150851 [Google Scholar] [CrossRef]
[11]. Chaturvedi A, Kumar A, Malignant pleural effusion with filariasisJournal of The Association of Physicians of India 2017 65(5):106-07. [Google Scholar]
[12]. Kolte SS, Satarkar RN, Mane PM, Microfilaria concomitant with metastatic deposits of adenocarcinoma in lymph node fine needle aspiration cytology: A chance findingJ Cytol 2010 27(2):78-80.10.4103/0970-9371.7075921157559 [Google Scholar] [CrossRef] [PubMed]