Internal Jugular Vein Thrombosis Mimicking Sternoclavicular Joint Septic Arthritis- A Rare Case Report
Surendra Umesh Kamath1, Arjun Ajith Naik2
1 Professor and Head, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Senior Registrar, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surendra Umesh Kamath, KMC Hospital, Attavar, Mangalore-575001, Karnataka, India.
E-mail: skamath3@hotmail.com
Internal jugular vein thrombosis is a vascular disease occurring spontaneously. Some of the predisposing factors include trauma, intravenous catheterization and deep neck infections. It is important to an orthopaedician, as it mimics sternoclavicular joint septic arthritis very closely. This can lead to wrong decision in opting for surgical drainage of the abscess which may turn out to be disastrous to the patient. Our case report describes a patient who presented to the emergency room with pain, swelling and redness over the sternoclavicular joint. Initial evaluation suggested septic arthritis of left sternoclavicular joint. On further evaluation this was ruled out and finally diagnosed as internal jugular vein thrombosis with adhesive capsulitis of left shoulder.
Intravenous catheterisation, Joint sepsis, Venous thromboembolism
Case Report
A 51-year-old female diabetic patient presented to the emergency room with pain, swelling and redness over the left clavicular region associated with a history of fever for the past three days.
She was diagnosed with an intracranial bleed two months ago for which she underwent conservative treatment. She was discharged three weeks later after reasonable functional recovery. Two weeks after discharge she developed pain, redness and localised swelling over the left sternoclavicular joint in order of presentation.
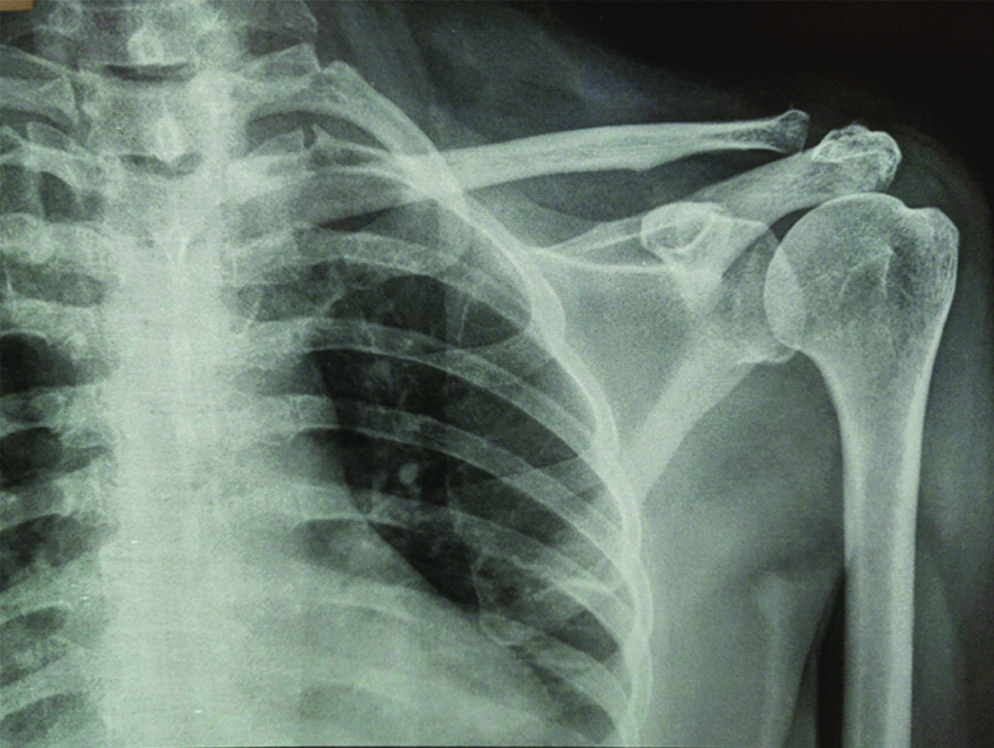
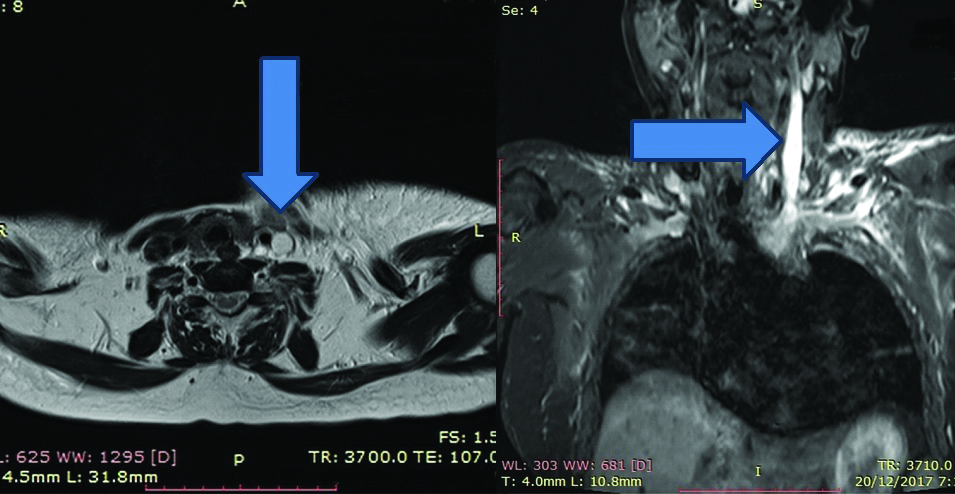
On examination, cervical lymph nodes were enlarged but non-tender. Local rise of temperature, diffuse swelling and redness was present over left sternoclavicular joint and the base of the neck. Left shoulder movements were grossly restricted in all planes. Radiographs of the left shoulder and sternoclavicular joint were normal [Table/Fig-1]. MRI scans of the left shoulder and sternoclavicular joint showed internal jugular vein thrombosis with tissue oedema around the vessel wall and confirmed no collection in the joint ruling out septic arthritis [Table/Fig-2]. A decision had to be taken on further plan of action with analgesics, antibiotics and anticoagulants or surgical drainage of the collection.
Radiograph of left shoulder and sternoclavicular joint.
Arrows showing thrombus in the Left internal jugular vein with diffuse vessel wall oedema.
After discussion with the cardio-thoracic vascular surgery and medicine department, it was decided that conservative line of management will be carried out. Blood was sent for culture and sensitivity. She was treated with intravenous antibiotics Piperacillin-Tazobactam, 4.5 g intravenous twice daily, analgesics (Diclofenac 75 mg twice daily and tramadol 50 mg twice daily intra muscular) and low molecular weight Heparin (5000 IU). Since blood culture was inconclusive, the antibiotic was not changed. After four days of therapy, clinical improvement in the swelling and redness was seen. However, the left shoulder pain persisted, which was re-evaluated and clinically appeared to be frozen shoulder. We treated the shoulder pain with physical therapy and ice-pack application. Intravenous antibiotics were given for two weeks. As the pain was severe and did not subside we had to administer a sub-acromial triamcinolone injection (dosage-40 mg). Her blood glucose levels were maintained within normal limits with insulin. She improved symptomatically and was discharged after two weeks of hospital stay.
On regular follow-up, patient showed signs of improvement. Two months later she presented with a localised swelling over the left sternoclavicular joint which was tender and fluctuant. Ultrasound of the swelling reported a well localised collection of pus measuring roughly 2×2.5 cm in the subcutaneous plane. Since the ultrasound scan gave a clear picture, no repeat MRI scan was required. The sternocalvicular joint was not involved. She underwent drainage of the pus under local anaesthesia. Culture of the pus drained showed Staphylococcus aureus with sensitivity to Cefuroxime. Therefore, antibiotic (Cefuroxime 500 mg twice daily oral) was administered for a period of two weeks until the wound healed and patient was asymptomatic. She recovered uneventfully.
Discussion
Isolated internal jugular vein thrombosis is a rare condition which usually presents as part of a Syndrome (Trousseau syndrome) or an associated condition (Ovarian Hyperstimulation Syndrome) [1,2]. However, in this case report we have not investigated the cause for the same. Early diagnosis and treatment is essential to avoid complications like infection, sepsis, pleuropulmonary complications, chylothorax and jugular foramen syndrome [3]. Most common clinical presentations are swelling and redness around the clavicle, cervical spine pain, painful shoulder movements and fever.
Studies have concluded malignancy [4] and hypercoagulable state [5] patients are more prone to this condition. Insertion of central venous catheter has shown to cause internal jugular vein thrombosis which can be explained by Virchow’s triad [6]. Septic jugular vein thrombosis is a life threatening condition due to the risk of pulmonary embolism and septic involvement of peripheral organs [7]. Inflammation and abscess formation in the nearby soft tissues has been well described [8].
However, the best non-invasive diagnostic modality for soft tissue infection is MRI. Few studies have published excellent results with contrast computed tomography, ultrasound scans and nuclear medicine scans. MRI provides better definition of soft tissues and sensitivity to blood flow rates. It does not require exposure to radiation unlike CT scans [9].
Many studies consider contrast CT scans to be gold standard in diagnosis of thrombosis [10-12]. The standard anticoagulation protocol administered to these patients includes low molecular weight or unfractioned heparin for a period of 5-7 days. This is immediately followed by oral anticoagulant therapy (warfarin or factor X inhibitors) for a period of three months [11]. The anticoagulant therapy in our case was low molecular weight Heparin 5000 IU administered sub-cutaneously for one week followed by oral warfarin 5 mg for a period of three months. However, when the patient presented again with a well formed localised abscess after two months in the subcutaneous plane of the sternoclavicular joint, drainage of the abscess followed by sensitive antibiotics for a total period of two weeks was administered until the symptoms completely resolved. The frozen shoulder had shown signs of improvement in terms of range of movement in this follow-up.
Conclusion
Internal jugular vein thrombosis can present as septic arthritis of sternoclavicular joint. One of the diagnostic modality (contrast CT or MRI scan) has to be carried out in any patient suspecting septic arthritis. This can be followed by the standard anticoagulation protocol. Since diabetics are prone to infection, antibiotics and if necessary, drainage of abscess must be carried out. Early diagnosis and adequate treatment can avoid life threatening complications.
[1]. Abbasi AA, Harrop NS, An unusual swelling in the neckEmergency Medicine Journal 2005 22(9):674-75.10.1136/emj.2004.01461316113203 [Google Scholar] [CrossRef] [PubMed]
[2]. Ayoub O, Cheang PP, Fryer J, Singh V, Spontaneous bilateral internal jugular vein thrombosis: A sign of metastasisJ Laryngol Otol 2004 118(7):570-72.10.1258/002221504161525415318969 [Google Scholar] [CrossRef] [PubMed]
[3]. Fliss DM, Gatot A, Hertzanu Y, Tovi F, Septic jugular thrombosis with abscess formationAnn Otol Rhinol Laryngol 1991 100(8):682-84.10.1177/0003489491100008161872521 [Google Scholar] [CrossRef] [PubMed]
[4]. Koshi A, Leci-Tahiri L, Tahiri A, Zherka-Saracini H, Bilateral internal jugular vein thrombosis due to malignant tumorJ Med Case Rep 2018 12(1):42-45.10.1186/s13256-017-1556-029458414 [Google Scholar] [CrossRef] [PubMed]
[5]. Bekkenk MW, Simmers TA, VidakovicVukic M, Internal jugular vein thrombosis after cervical tractionJ Intern Med 1997 241(4):333-35.10.1046/j.1365-2796.1997.95894000.x [Google Scholar] [CrossRef]
[6]. Butler G, Costantini L, Gu C, Lee AY, Levine MN, Webb C, Incidence, risk factors, and outcomes of catheter-related thrombosis in adult patients with cancerJ Clin Oncol 2006 24(9):1404-08.10.1200/JCO.2005.03.560016549834 [Google Scholar] [CrossRef] [PubMed]
[7]. Celikel UM, Muthuswamy E, Septic pulmonary emboli secondary to internal jugular vein phlebitis (post angina sepsis) caused by Eikenella corrodensAm Rev Resir Dis 1984 130(3):510-13. [Google Scholar]
[8]. Colley DP, Clark RA, Herwig SR, Merhar GL, Computed tomography demonstration of cervical abscess & jugular vein thrombosis. A complication of intravenous drug abuse in the neckArch Otolaryngol 1981 107(5):313-15.10.1001/archotol.1981.007904100510147224954 [Google Scholar] [CrossRef] [PubMed]
[9]. Holland GA, Carpenter JP, Baum RA, Magnetic resonance venography for the detection of deep venous thrombosis: comparison with contrast venography and duplex Doppler ultrasonographyJ Vasc Surg 1993 18(5):734-41.10.1016/0741-5214(93)90325-G [Google Scholar] [CrossRef]
[10]. Fagan J, Jonas N, Internal jugular vein thrombosis: a case study and review of the literatureThe Internet Journal of Otorhinolaryngology 2006 6(2):1-5.10.5580/1a8a [Google Scholar] [CrossRef]
[11]. Toratani M, Hayashi A, Nishiyama N, Nakamura H, Chida R, Komatsu T, Thrombosis in an internal jugular vein and an upper limb deep vein treated with edoxabanInternal Medicine 2017 56(9):1053-55.10.2169/internalmedicine.56.740528458311 [Google Scholar] [CrossRef] [PubMed]
[12]. Bandara AR, Gunathilake SSC, Kalupahana R, Wimalarathna H, Internal jugular venous thrombosis due to Trousseau’s syndrome as the presenting feature of metastatic prostate carcinoma: a case reportJ Med Case Reports 2016 10:104-07.10.1186/s13256-016-0884-927097872 [Google Scholar] [CrossRef] [PubMed]