The WHO defines traditional medicine as “the sum total of the knowledge, skill and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness” and complementary medicine as “a broad set of health care practices that are not part of that country’s own tradition or conventional medicine and are not fully integrated into the dominant health-care system” [1].
The interest in traditional and complementary medicine in both the developing and the developed countries is increasing [2]. Easy access, widespread acceptance by the general public, few side-effects, and contribution to economic growth are some of the positive features of traditional medicine [3]. Given the difficulty with having access to modern healthcare services, traditional and complementary medicine can stand as an alternative for the primary healthcare services [4]. Certain forms of traditional medicine, complementary and alternative, play an increasingly important role in healthcare and health sector reform worldwide [5].
In a system where traditional medicine and complementary medicine are integrated, they are recognised and introduced into all areas of healthcare [3]. The process of integration can be a stressful process for providers of both complementary and modern medical services [13]. The WHO supports the integration of traditional and complementary medicine into the national health system of countries [1].
The aim of this study was to identify the elements that have been mentioned concerning the integration of traditional and complementary medicine into primary healthcare and that need to be considered and prioritised by policymakers.
Materials and Methods
Data Sources and Search Strategy
This study was planned according to the “Preferred Reporting Items for Systematic Reviews and Meta Analyses” (PRISMA) guidelines and registered in Iran university of medical science (identification No: 9223476203/2016). The needed data were gathered by searching PubMed (1966-present), Embase (1947-present), Web of Science (1900-present), Scopus (1966-present), and Ovid (1946-present) from January 2000 to February 2017 and the last search was run on 11 February 2017. The search keywords were: (Integrat* OR collabor* OR converg* OR incorpor* OR inclu* OR cooper* OR contribut* OR blend* OR merg* OR assimilat*) AND (Tradition* OR complement* OR alternat* OR home OR primitive OR indigenous OR folk* OR ethno*) AND (Medic* OR therap* OR remed* OR heal* OR treat* OR cure*) AND (primary healthcare OR primary health care OR primary care OR PHC). All the related fields of the Medical Subject Headings (MeSH) and Emtree were searched. MeSH terms of traditional medicine, complementary medicine, integrative medicine, primary healthcare, East Asian traditional medicine, Korean traditional medicine, Tibetan traditional medicine, Mongolian traditional medicine, African traditional medicine, and Chinese traditional medicine were searched in PubMed. Combinations of traditional medicine keywords were also searched in the titles of the papers. The reference lists of eligible studies were scanned and hand searched for related studies. An example of the search strategy is provided in [Appendix 1].
Inclusion and Exclusion Criteria
The included criteria were: 1) Papers published in English; 2) Papers that focused on elements of integrating traditional or complementary medicine into primary health care; 3) Papers published from January 2000 to February 2017; 4) Access the full text of papers with any design (Qualitative, quantitative, mixed method)
The excluded criteria were: 1) Studies whose abstracts were only published; 2) Letters to the editor, editorials, commentaries and case reports; 3) Studies pointing to integration elements other than the issue of integrating traditional medicine into primary healthcare.
Data Extraction and Quality Appraisal
Data extraction was performed using a form that included the name of the author, year of publication, study design, characteristics and number of participants, and the introduced elements. Data were extracted by one author (Ahmad Negahban) and subsequently checked by another author (Mohammadreza Maleki).
The collected data were analysed using the content analysis method, which is a way of identifying, analysing, and reporting themes within a particular text [14,15]. Data was reviewed several times for familiarisation. There was no specific grouping before the analysis and codes and themes were developed according to their repetition within the text.
The analysis and coding steps consisted of getting familiar with the data by reading it several times, identifying and extracting primary codes, merging the codes to build themes, reviewing and completing the themes, naming and defining the themes, and assuring reliability of the codes and themes by reaching an agreement between the two coders.
Items of [Table/Fig-1] were used to appraise the quality of the included studies [16]. These items were selected because they can assess qualitative, quantitative, and mixed studies. Among the eligible studies, 24 were of high quality and one was of moderate quality; all of these were included in the analysis.
The used quality appraisal tool.
| Number | Item |
|---|
| 1 | An explicit theoretical framework and/or literature review |
| 2 | Aims and objectives clearly stated |
| 3 | A clear description of context |
| 4 | A clear description of the sample and how it was recruited |
| 5 | A clear description of methods used to collect and analyse data |
| 6 | Attempts made to establish the reliability or validity of data analysis |
| 7 | Inclusion of sufficient original data to mediate between evidence and interpretation |
Results
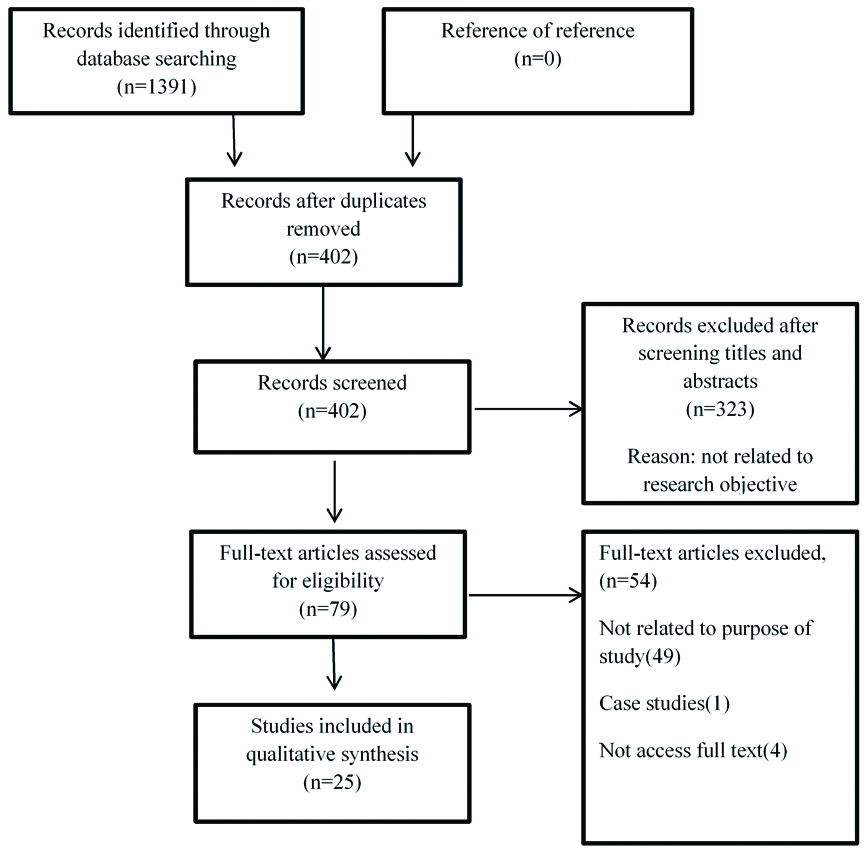
The search of databases resulted in 1391 records that were imported to EndNote X5 software. The duplicates were removed, titles and abstracts were screened and irrelevant records were excluded. Afterwards, full texts of the remaining records were reviewed for eligibility. Finally, 25 studies were included. [Table/Fig-2] conveys the screening and selection process according to a PRISMA flow diagram.
PRISMA flow diagram for screening and selection of the included studies.
Dimensions of Integrating Traditional Medicine into Primary Healthcare
[Table/Fig-3] displays the summary of included studies and their characteristics about the integration of traditional and complementary medicine into primary healthcare [8,17-40].
Summary of included studies and their characteristics [8,17-40].
| ID | Author, year | Study objective | Study design | Participants (N) | Integration elements |
|---|
| 1 | Obijiofor C [17] | Developing a policy to bring the traditional knowledge to the main stream of medicine by creating integrated clinics and providing demographic information on use of TM | Questionnaire | Patients (800) | Setting up IM courses in medical collegesTraining the CAM healersTraining the physicians, nurses and other health workersRecognition and identification of traditional treatments and traditional healerRecording and documenting the TMIncreasing public awarenessDeveloping electronic networks between researchers and civil societyGovernment should have economic, political, and legal frameworkNational policy in support of developing TMCollaboration between government, hospital societies, healers association, and Non-Government Organisations (NGOs) |
| 2 | Frenkel MA et al., [18] | Proposing a comprehensive and rational strategy for integration of CAM with primary health care | Combination of literature review, interview, FGD, Family Medicine residents’ courses, providers of CAM, clinical test at field | Patients, family physicians, providers of CAM | Patient-centeredness (expectations and needs of patients)Communication between patient and physician (patient enforcement and decision involvement)Communication and collaboration with traditional practitioners (common language can create collaboration)Physician in charge for follow and evaluation of treatment plan |
| 3 | Van Haselen RA et al., [19] | Evaluation of perspective of professionals of primary health care towards the need for integration of CAM and its ways | Questionnaire | Workers of primary health care including: physicians (149), nurses (24), other workers (32) | Referral or proposal of referralPatient needsNecessary need for more training and awareness of primary health care workers on CAMAbility to offer more treatments and increasing the patient choiceIncreasing patient satisfaction |
| 4 | Kelly M et al., [20] | Meaning the CAM and integration in perspective of policy makers and identifying its facilitators and barriers | Qualitative study | State policy makers (10) | Evidence-based research on CAMAccreditation and training standards for providers of CAMEconomic issuesConstruct issues such as lack of insurance coverage and the system resistanceSponsorship role and strategic planningHaving a model for providing the CAM |
| 5 | Ben-Arye E et al., [21] | Enforcing the family physicians as coordinator and manager of patients who request the CAM | Educational approach | Residents and specialists of Family Physician (12) | Using online resources and collaboration with providers of CAMEvidence for CAM efficacy when cosidering referralBio-spiritual-social issuesDisease-orientedPatient-orientation |
| 6 | Sundberg T et al., [22] | Describing some key findings of developing and implementing a model for integrated medicine for primary health care | Qualitative inductive study | General physicians, providers of CAM, specialists, managers of primary health care, city council members (48) | Common integrated medicine documentation should reflect multi-modular management, and preferably be computer-basedPatient-centerednessInter-disciplinary and non-hierarchical combination of conventional and CAM for treatment of patient casesAttachment of the integrated medical model for standard clinical treatment of each patient by agreement between the family physician and the team of complementary medical service providers.Investment and resource allocation for improving and planning of the providersHealth economic evaluation of integrated medicine compared with conventional medicine as an incentive for management decisionsAvailability of training on integrated medicine for the general physicians |
| 7 | Frenkel M et al., [8] | Expressing the viewpoints of patients treated in a large family physician clinic on integration of complementary and alternative medicine with primary health care | Questionnaire | Patients (502) | Family physician as the provider and supervisor of primary health careProviders of CAM as a part of family medicine clinic |
| 8 | Garner MJ et al., [23] | Assessing perspectives of two teams of healthcare providers on effects of integrating the chiropractic | Combined methods (questionnaire, FGD for evaluation of heath teams) | Physicians and registered nurses (12), chiropractors (2) | Choosing an interested person for cooperation with health care teamConstructive communication and planning within the defined health care team and the chiropractorsFormal training sessions for health workers to remove the false imagination about chiropractors and weekly clinical sessions for the chiropractors |
| 9 | Ben-Arye E et al., [24] | Assessing the distance between theory and real practice by reviewing the attitudes of patients, physicians and providers of CAM about the integration of CAM with primary health care | Questionnaire | Patients (1150), primary health care physicians (333), providers of CAM (241) | Main role of the physicians as referral for CAMFamily physicians as providers of CAM |
| 10 | Ben-Arye E et al., [25] | Assessing the viewpoints of patients on integration of complementary and alternative medicine with primary health care and finding the best model of integration | Questionnaire | Patients (3840) | Major role of the family physicians: correct and safe referral of the patients to providers of TMCultural multiplicity |
| 11 | Ben-Arye E et al., [26] | Comparing two social groups to assess the effects of modernisation on use of traditional, complementary, and alternative medicine | Questionnaire | Primary health care patients (1341) | Family physician as the beginning point of referral to CAMNative participants had higher expectations from their physician to refer them to CAM and provide CAM in the clinic.Any integration of CAM should be based on the culture of the society |
| 12 | Joos S et al., [27] | Determining the attitudes of the family physicians towards the CAM and its use | Questionnaire | Family physicians (1027) | Training and research on CAM according to the international literature should be increasedPatients are willing to receive the CAM from those physicians that have good knowledgeAll CAM treatments that are evidence-based should be covered by health insuranceStandards of training and quality should be defined by health policies.Role of the naturopaths (heilpraktikers) in the health care system of Germany should be revised immediatelyIntegrating the evidence-based methods of CAM in the under-graduate coursesPractical integration of CAM in the residency courses |
| 13 | Wu J et al., [28] | Assessing the quality of trainings provided by the joint clinics of acupuncture to the students of acupuncture and conventional medicineAssessing the referral of primary health care physicians to acupuncture and other medicinesAssessing the quality of communication between acupuncture providers and the primary health care physicians | Questionnaire | Interns (24), medical students (2), acupuncture supervisors (2) | Sending a summary of diagnosis, treatments and recommendations to the primary health care physician via an electronic message or telephone33% of the primary health care physicians practice acupuncture as a therapy |
| 14 | Ben-Arye E, [29] | Discovering the perspectives of primary health care and physicians and non-physician providers of CAM at HMOs about integrated medicine | Questionnaire | Primary health care physicians (333), CAM providers (241) | Physicians trained in both medicines as mediators of integrationPhysicians support a model of group work in which physician is dominant; like the physicians’ role in primary health careNon-physician providers of primary health care support a model of teamworkPhysicians trained in both medicines mostly use the referral sheet as the preferred communication tool between physician and the provider of CAM |
| 15 | Templeman K et al., [30] | Review and identification of models for integrated medicine around the world and identification of influencing factors in success of the integration of conventional and CAM in primary health care | Literature review | databasesearches, reference lists, desktop searches, texts, and relevant website searches | Evidence-based treatmentIntegrated therapies without any hierarchy of conventional medicine and CAMPatient-centeredness and focus on health rather than sicknessEfficiency and safety of CAMSafety of CAM productsManagement of CAM products along with training, qualification, and regulation of CAM providersStrategic cooperation of the methods and technologies of both complementary and conventional medicine rather than just being togetherHighlighted role of medical elites |
| 16 | Ben-Arye E et al., [31] | Discovering the perspectives of parents regarding the use of CAM for their children and assessing their perspective towards the concept of physician-parents relation and physician-complementary medicine provider relation | Questionnaire | Parents (599) | Relation between physician and CAM provider can improve the health and safety of childrenHighlighted role of physicians in referral to CAM and important role of physicians in providing CAM services |
| 17 | Ben-Arye E et al., [32] | Studying how patients from various regions of the country see the possibility of adding herbal medicine to primary health care teams in local clinics | Questionnaire | Patients (3713) | Depending on various cultural attitudesPrimary health care physicians start to talk with their patients about CAM and herbal drugs |
| 18 | Jong MC et al., [33] | Expressing the viewpoints of patients on integration of CAM with primary health care | Combined methods (questionnaire, electronic panel, FGD) | Patients (416), electronic panel (3449), FGD (10) | General physician as referral and collaborates of the CAM providers (for patients)Developing policies for communication with CAM and referral to the providers of CAM in primary health care |
| 19 | Chung VCH et al., [34] | Creating potential strategies for development of collaboration between the conventional and Chinese TM | FGD and Delphi technic | Physicians (50), Chinese TM practitioners (50), Delphi with political stakeholders of conventional and Chinese medicine | Physicians of both paradigms should have common goal of providing patient-centered carePromotion and development of protocols for joint care and information exchangeEnforcing the collaborations between professionals and leadership for integrationAttitudes of political stakeholders about possibility of strengthening the trust and mutual learning of conventional and Chinese medicine and increasing the innovation and government support |
| 20 | Shuval, JT et al., [35] | Discovering the perspectives of primary health care physicians which have integrated the CAM with biomedicine, towards the boundaries they encounter in their daily clinics and discovering how to deal with epistemological problems and potential disagreements | In-depth interview | Family Physicians (15) | Practice boundariesIdentity boundariesEpistemological boundariesCognitive boundariesOrganisational boundariesSocial boundariesAttending conferences and groups to remove the social boundariesNo insurance coverage for CAMSecret use of CAM methods with biomedicine methodsCultural diversityBehavior and values of family physicians which consider the CAM as an inseparable part of treatmentQuality of CAM methodsTime and place of providing CAM |
| 21 | Hunter J et al., [36] | Determining the success and challenging factors of integrated medicine clinics | Combined methods of qualitative and quantitative | Patients (97) | Common perspective, an open and clear culture, Reliable sponsors, appropriate facilities, trust in the capacity and ability of other providersPatient-oriented careMarketing strategies and trying various therapies and clinical servicesFinancial planningManagement of staff and provider turnoverBalance between physicians of conventional medicine and other providers and also between the personnel and the provided servicesBuilding a team of integrated medicineCreating research capacity |
| 22 | Owolabi OO et al., [37] | Discovering viewpoints and justifications of stakeholders about join of the traditional midwives to the health system | Discussion by E-mail | Front line workers of care and health and citizens (193) | Based on structure of health systemLocal and international evidence on efficacy, need, acceptance, and feasibility |
| 23 | Gray B et al., [38] | Studying the perspectives of workers about theory and practice of models of integrated medicine regarding the affecting factors of referral | Qualitative method with semi-structured interviews | Physicians (2), Naturopaths (2), Osteopaths (2) from two primary health care clinics | Relations of the professionals and the referral networks have a major role in effectiveness of the integrated medicine clinics.Sharing the philosophy and common beliefs about integrated medicine and holistic medicinePersonal and professional relations between providers show mutual trust and respect. Mutual relations increase the referrals.Cooperation between professionals |
| 24 | Habtom GK [39] | Assessing the perception and perspective of modern medicine practitioners and TM practitioners about TM methods and analysing the use of TM | Questionnaire and interview with key individuals | Physicians (250), traditional practitioner (250), 1657 families | Selective integration of TM methods with primary health careDeveloping the political, legal, and supervision for the TM methods regarding national policies and lawsImprovement and conduct of scientific research on medicinal herbs for collaboration with traditional practitioners and proving safety, efficacy, and quality of traditional drugsEnsuring intellectual property rights as priorities of government agenda to maintain the native knowledge of TMCreating an economic, supervision, and political environment for local production of traditional drugs and developing the industries that increases the access by producing standard drugsRegistration and regulation of traditional drugs according to the instructions of the WHOPublishing information about the proper use of traditional drugsCreating capacity of human resources and material to carry out and complete the institutionalisation strategies |
| 25 | McGuire C et al., [40] | Improving the perception of facilitators and barriers of the integrating psychosomatic medicine with primary health care and describing the experiences of providers of psycho-somatic cares | Qualitative analysis of semi-structured telephone interviews | Providers of psychosomatic cares (12) | Systematic changes: care based on values and beliefs, community savings, responsible care, reviewing patient reports for assessing quality of careIncreasing education on psycho-somatic medicine and self-care for service providers and interaction with providers of psychosomatic primary care at the policy making levelInsurance coverage for psychosomatic medicineSufficient time for visits at the clinics |
CAM: Complementary and alternative medicine; IM: Integrative medicine; FGD: Focus group discussion; HMO: Health maintenance organization
Communication and Collaboration: Eighteen studies addressed the consultation, collaboration, and active participation of physicians, and complementary medicine practitioners [8,17,19,21,26,28-31,33,34,38,39].
Patient-Centeredness: Twelve studies mentioned the demands and needs of patients and the centeredness of patients and sickness [18,19,21,22,27,30,32-34,36,38,40].
Practice: Twelve studies addressed types of services that would be integrated into primary healthcare [17,20-22,25-27,30,32,35,37,39].
Education and training: Eleven studies mentioned education and training in terms of training to be delivered to physicians, nurses, healthcare workers and the general population, as well as education in integrative medicine in medical colleges and the use of online resources [17,19,21-23,27,29,30,39,40].
Policy and plan: Eight studies mentioned policy making, strategic planning and legislation [17,20,27,30,33,34,39,40].
Financial support: Seven studies addressed financial issues, insurance and economic evaluation [17,20,22,27,35,36,39].
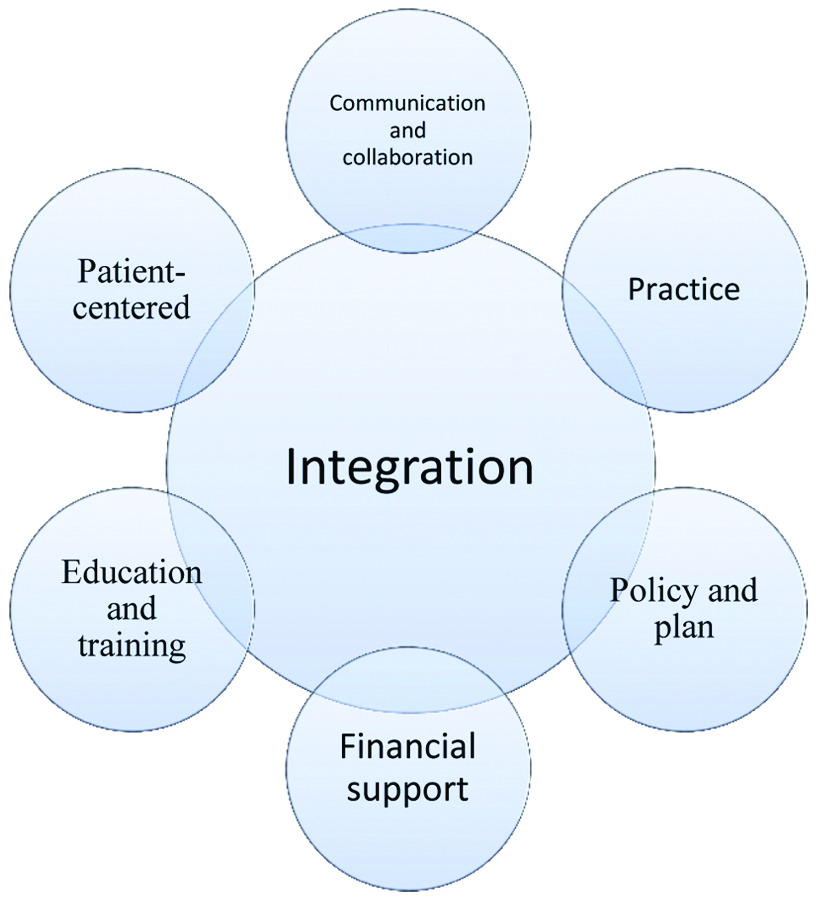
[Table/Fig-4] depicts the summary of study findings on the elements of integrating traditional medicine into primary healthcare.
Elements of integrating traditional medicine with the primary health care.
[Table/Fig-5] displays themes and related codes identified in the reviewed studies.
Themes and related codes identified in reviewed studies on integration of traditional medicine and primary healthcare.
| Number | Themes | Codes |
|---|
| 1 | Communication and collaboration | Professional relationshipMutual respect and trustCommon languageProtocol for shared care and information exchangeReferences among practitionersActive role of physicians in reference and supervising treatment |
| 2 | Patient-centered | Bio-psycho-social approachPatient’s expectations and needsPatient-doctor communicationPatient’s demandsPatient’s choicePatient’s satisfaction |
| 3 | Practice | Evidence-based (safety, efficacy, and quality)Appropriate with culture and prominent CAM modalitySelective integrationInterdisciplinary and non-hierarchical blending of conventional and complementary medicine in all patient management casesRecognition and identificationRecording and documentationIntellectual property rights |
| 4 | Education and training | Public awarenessIntegrate CAM training in medical schools (undergraduate and residency)Training for CAM practitionersEducation for health workersMutual learningStandards of accreditation and training for CAM practitionersStandards on education and quality control should be introduced by healthcare policy |
| 5 | Policy and plan | Government supportNational policies in support of TM developmentModel for service delivery advocacy and strategic planningInvolvement of CAM providers at the policy level |
| 6 | Financial support | Reimburse all CAM therapiesImprove provider participation and planningHealth economic evaluation motivating management decisions for IM managementCarry out and accomplish institutionalisation strategiesFunding and resource allocationEconomic evaluation |
TM: Traditional medicine; CAM: Complementary and alternative medicine; IM: Integrative medicine
Discussion
This study systematically reviewed the literature for various elements of integrating traditional medicine into primary healthcare, whereby six elements were found including communication and collaboration, patient-centeredness, practice, education and training, policy and planning and financial support.
We found communication and collaboration between traditional medicine and modern medicine groups are among the most important elements of integrating traditional medicine into primary healthcare. The interrelationships between professionals are highly conducive to integration [19,20,23,30,34,38]. Garner MJ et al., considered the collaboration between healthcare and complementary medicine providers essential for successful integration, which needs to be pursued by an interested professional [23]. The study by Ben-Arye E et al., described the collaboration between the physician and the providers of complementary medical services as highly important in promoting the health and well-being of children [31]. Gray B et al., highlighted the good and effective relationship between the professionals of the two groups that can result in better efficacy of the integrated medicine [38]. The stronger and more widely these relationships are established at different levels, the better the integration will be [34].
On the other hand, patient-centeredness along with attention to the patient’s request and needs at all stages of the integration process is another element that has been mentioned by numerous studies [18,19,21,22,34,38]. For a successful integration, the patient must have the ability to decide on the treatment [18]. In the model presented by Sundberg T et al., in Switzerland, the integrated services are determined according to both the circumstances of each patient and the agreement reached between the therapeutic teams of modern medicine and complementary medicine [22]. The patient-centeredness is one of the effective elements in improving the quality of the integrated clinics [38]. In Chung VCH et al.’s study, patient-centeredness is described as the common goal of modern and traditional therapists [34].
Another element to consider when integrating traditional and complementary medicine into primary healthcare is the type of service. In the United States, the Federation of State Medical Boards has set guidelines for applying the type of complementary medical services, which is a document that involves guidelines for training physicians and providers of complementary medicine [41]. In Sundberg T et al., proposed model, the type of integrated service should be selected from the complementary or conventional medicine services according to the patient’s conditions as decided and agreed by the healthcare team members [22]. In the study of Templeman K et al., two models are proposed for the integration of the type of complementary medicine service: a model where experience-based complementary medicine is integrated with the conventional medicine, and a model that builds only on evidence-based complementary medicine [30].
Another issue that should be considered in integrating traditional medicine into primary healthcare is education and training. Increasing the knowledge of primary care professionals concerning complementary medicine is a must in order to have a better integration. The study of van Haselen RA et al., suggests that education on integrated medicine to primary healthcare professionals is a must [19]. Joos S et al., from Germany pointed to education as one of the elements on which insurance agencies should invest in order for better access to integrated medicine [42]. Also, Anastasi JK et al., mentioned that while integrated therapies are being applied by the general public, health service providers are not aware of the bases and resources that provide safe and effective treatments [43].
One of the key elements for integrating traditional medicine with primary healthcare is the policymaking and planning. The White House Commission on Complementary and Alternative Medicine Policy has postulated 10 guidelines for policy formulation as well as policy proposals for integration of complementary medicine [13]. Policymakers should develop policies and methods that help integrate complementary and alternative therapies in the modern medicine [44]. Jong MC et al., described it as imperative to formulate policies concerning the relationship between general practitioners and providers of complementary medicine and referral between them in order for integration into primary healthcare [33]. Also, Park H-L et al., highlighted the key role played by national policies in integrating and expanding traditional medicine in China, Japan, and South Korea [45]. In Awodele O et al., study, about 70 percent of traditional medicine practitioners believed that it was necessary to have national policies for traditional medicine [46].
Another issue is the financial supporting for the integration of services. In a study by Obijiofor C, it recommends financial support from the government, NGOs, and other stakeholders in the developed countries for integration of traditional medicine into primary healthcare [17]. Thomas KJ et al., considered financial issues as one of the contributors to the integration of complementary medicine into primary healthcare [47]. Joos S et al., proposed increased funding for research, training, and rewarding physicians for access to integrated medicine in the primary healthcare [42].
Limitation
A limitation of this study was that the literature search was not performed on all scientific databases. However, major related databases were searched and related records were retrieved. Additionally, several synonyms of keywords were searched to ensure that all potentially eligible records would be identified. Another limitation was restricting the search to the English language, whereby we may have missed studies in other languages.
Conclusion
The traditional and complementary medicine should be integrated into primary healthcare gradually through correct policies. Planning and policymaking should involve practitioners of both traditional and conventional medicine. The role of professionals in both fields of medicine is highly important for establishing collaboration between, and providing education to, other stakeholders of the healthcare system. Without this, integration will not be strongly implemented. To accelerate successful integration, types of services must be in line with the community’s culture. The services should also be covered by insurance. The goal and outcome of integration are to provide services that are efficient and have the quality necessary to ultimately satisfy the patient.