Biloma Presentation after Six Months of Thoracoabdominal Trauma: A Case Report
Mojtaba Ahmadinejad1, Saman Afrasiabi2, Izadmehr Ahmadinejad3
1 Thoracic Surgeon, Department of Surgery, Alborz University of Medical Sciences, Karaj, Alborz, Iran.
2 Medical Student, Department of Student Research Committee, Alborz University of Medical Sciences, Karaj, Alborz, Iran.
3 Researcher, Department of Biology, Iran Atomic Energy High School, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Saman Afrasiabi, Student Research Committee, Alborz University of Medical Sciences, Baghestan, Karaj, Alborz, Iran.
E-mail: samanafra@gmail.com
Perforation of biliary tree will result in accumulation of bile as a collection called biloma. Post-traumatic biloma is diagnosed mostly soon after the trauma happened. We are reporting about a patient with traumatic biloma whose manifestation of symptoms appeared six months after an abdominal blunt trauma. A 65-year-old male reported with the complaint of nausea and abdominal pain since three days. On examination, a rigid abdominal mass was detected in the right upper quadrant, which was increasing in size. The patient had a record of admission in his medical history due to blunt thoracoabdominal trauma, six months ago. On laboratory investigations, there was a rise in the level of alkaline phosphatase. Computed Tomography scanning showed a fluid collection with pressure effect on liver. Emergency operation was performed for drainage and about 2 L of bile was discharged via percutaneous drainage. CT scan performed immediately after operation showed liver in the normal site and decompressed. Following-up, the patient was asymptomatic for one year. Traumatic biloma is a probable diagnosis in patients with abdominal trauma even if there is a long period of time between the incidence of trauma and the appearance of symptoms. Biloma is managed mostly by surgical methods in order to drain and find the leakage but in some cases even a percutaneous drainage can be effective.
Abdominal injuries, Abdominal pain, Biliary tract
Case Report
A 65-year-old, Iranian man reported to our hospital with the complaint of nausea and abdominal pain that had been ongoing for three days. He also complained about a rigid mass which was seemingly increasing in size. On examination, abdominal tenderness and a mass with dull palpation in the right upper quadrant of the abdomen was detected. Abdomen was visibly bulging but there were no signs of jaundice or fever.
The patient had a history of admission due to blunt trauma from car to car accident, six months back. Due to fall in accident, he was admitted in the hospital for blunt thoracoabdominal trauma that resulted in fracture of left ribs and a subcapsular haematoma. He underwent emergency haematological laboratory tests and radiological investigations. In laboratory investigation, haematologic factors were normal and there were no signs of infection. Also, he had normal biochemical results and renal function tests did not suggest any complications. The patient had a normal total bilirubin, direct bilirubin and blood coagulation tests. Liver function tests were as follows: ALT 47 IU/L, AST 48 IU/L, and ALKP 1405 IU/L. However, his lab tests showed an extreme rise in the rate of alkaline phosphatase (Reference range: 41 to 133 IU/L) which suggested a liver function problem.
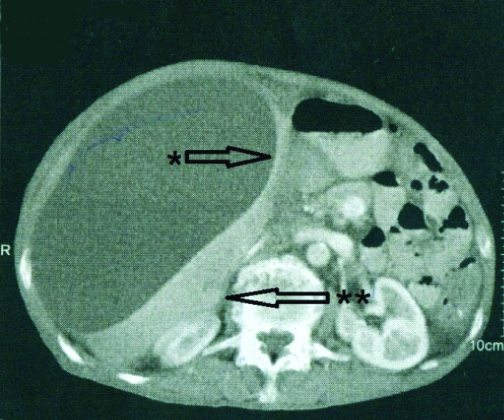
On X-ray imaging, pleural effusion of the right lung was obvious. Computed Tomography scanning showed a huge fluid collection in subcapsular area of liver with pressure effect on the liver. The capsulated mass sized 23×18×12 cm in the CT scan [Table/Fig-1]. Differential diagnosis suggested in the imaging report was haematoma or biloma.
Biolma (*) had a pressure effect on liver (**). Liver is compressed.
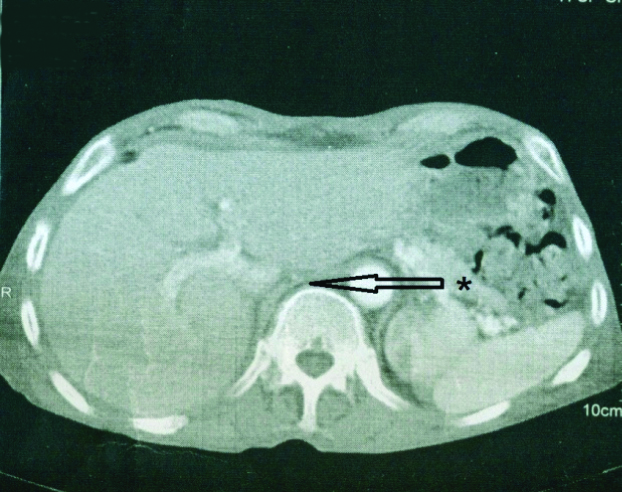
After all the investigations and patient consent, he was transferred to the operating room as an emergency case. Under general anaesthesia, a percutaneous drainage of the mass was performed and 2000 cm3 of bile-stained fluid was aspirated. A subhepatic drain was placed after drainage. Secondary CT scan which was performed post-operatively showed no signs of any abnormal mass and the liver had a normal size [Table/Fig-2]. The drain output after surgery was bilious but the volume decreased in two weeks and finally there was no excretion. Patient was discharged after the leakage stopped and the imaging results were normal.
Liver (*) is in the normal site immediately after discharge. Liver is decompressed.
After one year, all the liver function tests were normal and the patient was asymptomatic. Control CT scan after discharge was normal and no complaint was received from the patient.
Discussion
In medical literature, most prevalent causes of biloma are considered to be surgery and trauma [1,2]. The first case of biloma was reported by Gould L et al., in which the patient had an abdominal trauma caused by bile leak and the accumulation of bile in an encapsulated form resulted in biloma [3]. A perforated bile duct usually appears either localised as an encapsulated collection or a generalised biliary peritonitis. Iatrogenic biliary tree injuries during procedures such as hepatobiliary surgery, percutaneous transhepatic surgical approaches and ERCP-related procedures cause biloma [4]. Iatrogenic bilomas increase from 0.1% to 1.5% due to preference for laparoscopic abdominal surgery over open abdominal surgery approach [5,6]. Cholecystectomy is the most common cause of iatrogenic bilomas [2,7]. Beyond iatrogenic causes, spontaneous rupture of the biliary tree and traumatic injuries, whether blunt or penetrating, may cause biloma [4]. In comparison to other causes, spontaneous perforation of the bile duct is rare. Common causes of spontaneous biloma are congenital biliary malformations in children, and choledocolithiasis in adults [1,8]. Differential diagnosis of intra-peritoneal collections should include haematoma, seroma, liver abscess, cyst, pseudocyst and lymphocele [7].
Management and treatment of biloma may vary case by case. Different techniques have been used from percutaneous aspiration and catheter drainage to overt surgical treatments [9]. Endoscopic decompression and endosonography-guided biloma drainage have also proved to be successful approaches for managing biloma [10]. In case of smaller leaks of biliary tree, biloma is often self-limiting and resolves spontaneously in few days [9].
Conclusion
Although the most attributed etiology of biloma is iatrogenic, traumas, particularly those near the biliary tree and liver should also be closely monitored for they can also be a cause for the disease. Traumatic biloma should be ruled out in any patient who is admitted for post-traumatic abdominal masses; even if there is only a few months interval between the trauma and the appearance of symptoms. Management of biloma depends on many factors but most of the cases should be treated by surgical methods. In this case, the whole bile fluid was aspirated by a simple percutaneous drainage.
[1]. Bas G, Okan I, Sahin M, Eryılmaz R, Isık A, Spontaneous biloma managed with endoscopic retrograde cholangiopancreatography and percutaneous drainage: a case reportJ Med Case Rep 2011 5(1):310.1186/1752-1947-5-321210994 [Google Scholar] [CrossRef] [PubMed]
[2]. Sawaya Jr DE, Johnson LW, Sittig K, Iatrogenic and noniatrogenic extrahepatic biliary tract injuries: a multi-institutional reviewAm Surg 2001 67(5):473 [Google Scholar]
[3]. Gould L, Patel A, Ultrasound detection of extrahepatic encapsulated bile: “biloma”AJR Am J Roentgenol 1979 132(6):1014-15.10.2214/ajr.132.6.1014108953 [Google Scholar] [CrossRef] [PubMed]
[4]. Igarashi H, Yamashita H, Tsuchiya K, Sugimoto D, Ogata I, Intrahepatic subcapsular biloma after endoscopic retrograde cholangiopancreatography treated by endoscopic biliary drainageJ Clin Gastroenterol 2018 11(2):167-71.10.1007/s12328-017-0806-4 [Google Scholar] [CrossRef]
[5]. Kannan U, Parshad R, Regmi SK, An unusual presentation of biloma five years following cholecystectomy: a case reportBMJ Case Rep 2009 2(1):804810.4076/1757-1626-2-8048 [Google Scholar] [CrossRef]
[6]. Lee JH, Suh JI, A case of infected biloma due to spontaneous intrahepatic biliary ruptureKorean J Intern Med 2007 22(3):220-24.10.3904/kjim.2007.22.3.22017939343 [Google Scholar] [CrossRef] [PubMed]
[7]. Vaghela P, Patel J, Shah D, Shah M, Vaghela R, Bilioma due to blunt abdominal trauma: a case report and review of literatureInt J Surg Med 2017 3(3):200-02.10.5455/ijsm.20150808121006 [Google Scholar] [CrossRef]
[8]. Yasar NF, Yasar B, Kebapçı M, Spontaneous common bile duct perforation due to chronic pancreatitis, presenting as a huge cystic retroperitoneal mass: a case reportBMJ Case Rep 2009 2(1):627310.4076/1757-1626-2-627319918569 [Google Scholar] [CrossRef] [PubMed]
[9]. Okello TR, Ocen D, Okello J, Pecorella I, Amone D, Case Report: Biloma gastrostomy after failed sonogram-guided percutaneous aspiration, pigtail catheter insertion and surgical drainageAAS Open Research 2018 :110.12688/aasopenres.12876.1 [Google Scholar] [CrossRef] [PubMed]
[10]. Piraka C, Shah RJ, Fukami N, Chathadi KV, Chen YK, EUS-guided transesophageal, transgastric, and transcolonic drainage of intra-abdominal fluid collections and abscessesGastrointest Endosc 2009 70(4):786-92.10.1016/j.gie.2009.04.04919577742 [Google Scholar] [CrossRef] [PubMed]