Schwannomas are infrequent tumours of oral cavity that are not routinely included in the differential diagnosis of oropharyngeal masses. The tumour presents with non-specific clinical symptoms and is clinically indistinguishable from varied soft tissue neoplasms of the oral cavity. Of the 84 cases of lingual schwannoma reported in English literature in the past 61 years, only 18 cases have been reported in paediatric age group ranging from 1 to 15 years. We, herein, report a rare case of schwannoma of the tongue in a 14-year-old boy, presented as a painless swelling with characteristic Antoni A and Antoni B pattern with Verocay bodies on histopathology. Strongly positive immunohistochemical staining with S 100 protein confirmed the Schwann cell origin.
Case Report
A 14-year-old boy presented with slowly progressing non-tender swelling at the tip of the tongue for three months duration. There was no history of trauma or bleeding. The swelling was not associated with dysphagia or dysphonia. The patient was otherwise healthy. There was no significant personal, past or family medical history. Intraoral examination revealed a smooth, firm, non-tender, non-ulcerated swelling, one centimeter in diameter, present towards the right lateral border of anterior two-thirds of tongue. The margins were well-demarcated. There was no associated neurologic deficit or palpable neck nodes. The rest of the oral and head and neck examination was unremarkable. The systemic examination revealed no swelling elsewhere. All routine laboratory investigations were within normal limits. No imaging modalities were done as the swelling was easily visible and palpable. The provisional work up diagnosis was oral fibroma, mucocele and haemangioma. An excisional biopsy was planned as a diagnostic and therapeutic measure. The patient underwent transoral excision of the swelling under general anaesthesia. After applying two stay sutures, an oblique incision was made over the swelling. The whole mass was completely enucleated from beneath the mucosa using blunt dissection and primary closure was done. Intraoperatively, the mass appeared well-encapsulated with no extension to surrounding muscle or nerve fibers. The postoperative period was uneventful.
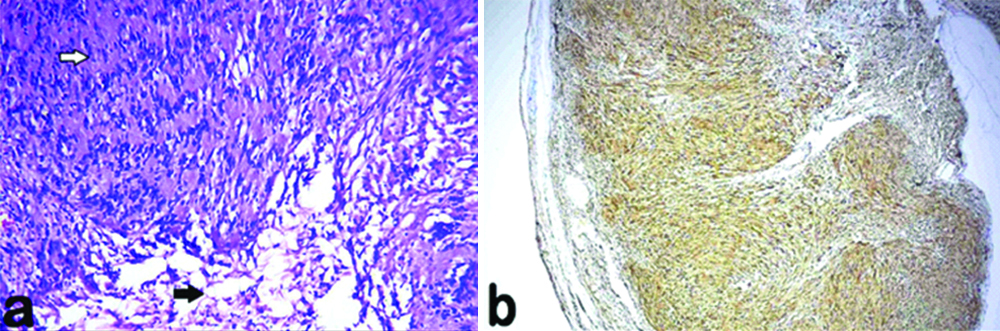
The excised specimen was a well-encapsulated nodule measuring 1×0.7×0.5 centimeter size. The cut surface was firm and grey white in colour [Table/Fig-1]. On histopathological analysis, the nodule was a benign neoplasm with dual hypercellular (Antoni A) and hypocellular (Antoni B; [Table/Fig-2a]) pattern. Antoni A pattern comprised of closely packed spindle shaped tumour cells arranged in interlacing bundles and in rows with elongated palisaded nuclei embedded in a neurofibrillary stroma forming Verocay bodies in between. Antoni B pattern comprised of less number of disorganized tumour cells separated by abundant oedematous stroma. No mitosis or necrosis was seen. The tumour showed complete excision. The histological features were that of a schwannoma. A strongly positive immunohistochemical cytoplasmic reaction for S 100 protein confirmed the diagnosis [Table/Fig-2b]. After the final diagnosis, a thorough objective general examination was performed to check the presence of other characteristic signs of Von Recklinghausen’s syndrome, including spinal and peripheral neurofibromas, café au lait macules, axillary and inguinal freckling, optic gliomas, Lisch nodules, skeletal deformities, neurological or cognitive impairment, malignant tumours of the nerve sheath, and pheochromocytoma. The patient had no signs of von Recklinghausen’s syndrome. He was followed-up for a period of one year after surgery and there was no evidence of any recurrence of the tumour.
Excised specimen of tongue nodule.

a) Photomicrograph showing the Antoni A region (white arrow) where spindle shaped tumour cells are arranged in palisaded pattern forming Verocay bodies and Antoni B region (black arrow) where tumour cells are loosely arranged in an oedematous stroma (haematoxylin and eosin, original magnification x200); b) Tumour strongly positive for S 100 protein.
Discussion
Schwannoma of the tongue is a slow growing benign tumour of nerve sheath origin first described by Verocay in 1908 [1,2]. It is relatively rare in the head and neck, with an incidence of approximately 25-45% cases. Of these, 1% cases occur intraorally, most frequently being the tongue [3,4]. In the review of literature, few studies have reported that base of the tongue is the commonest site while other studies have reported approximately 66% cases in the anterior one-third of tongue [5]. The peak incidence is between third and sixth decade with no gender predilection and is relatively rare in paediatric age group with only about 18 in 84 cases reported in English literature in a duration of six decades [3,6,7]. Including the present case, 19 cases of lingual schwannoma have been reported till now.
A review of literature about the 19 paediatric cases have been described in [Table/Fig-3] [1-3,7-19]. The mean age at presentation was 13.2 years. Eleven cases were males and eight cases, females. Fourteen cases (73.7%) presented with lump on the tongue. Mean size of the tumour was 1.5 centimeter. The tumour was anterior in location in 11 (57.9%) of the cases and, posterior in seven (36.8%) of the cases. Standard treatment was transoral excision in 17 (89.5%) cases. All cases were histopathologically diagnosed as schwannoma. The overall disease free survival ranged from 3-136 months (median, 12 months).
Demographic and clinical features of lingual schwannomas in paediatric age group reported in literature [1-3,7-19].
| Author | Year | Gender (M/F) | Age (yrs) | Size (cm) | Site | Clinical presentation | Surgical approach | Follow-up (months) |
|---|
| Craig D [8] | 1964 | F | 8 | 3 | Posterior | Lump | Transoral | |
| Akimoto Y et al., [9] | 1987 | M | 15 | 1 | Anterior | Lump | Transoral | |
| Cinar F et al., [10] | 2004 | M | 7 | 1 | Anterior | Lump | Transoral | |
| Bassichis BA et al., [11] | 2004 | M | 9 | 2.3 | Posterior/base | Snoring | Transoral | 60 |
| Nakasato T et al., [12] | 2005 | F | 9 | 2 | Posterolateral/base | Bleeding/ulceration | Transoral | 17 |
| Hsu YC et al., [13] | 2006 | M | 9 | 1.2 | Anterior | Lump | Transoral | 56 |
| 2006 | F | 15 | 2 | Anterior | Lump | Transoral | 136 |
| 2006 | F | 12 | 1.6 | Anterior | Lump | Transoral | 13 |
| Enoz M et al., [14] | 2006 | M | 7 | 2.5 | Anterior | Dysphagia/pain | Transoral | 60 |
| Pereira LJ et al., [15] | 2008 | M | 12 | 1.5 | Posterolateral/ventral | Lump | Transoral | 12 |
| Karaca CT et al., [16] | 2010 | F | 13 | 2 | Posterolateral/ventral | Dysphagia | Transoral | 12 |
| Cigdem T et al., [17] | 2010 | M | 13 | 2 | Anterior/ventral | Lump | Transoral | |
| Naidu GS et al., [2] | 2010 | M | 12 | 2 | Anterolateral/ ventral | Paresthesia/bleeding/ulceration | Transoral | 3 |
| Lukšić I et al., [18] | 2011 | M | 10 | 1.5 | Postero midline | Lump | Transoral | 60 |
| Husain S et al., [3] | 2011 | F | 10 | 5 | Left lateral | Lump | Transoral | 12 |
| Manna F et al., [7] | 2012 | M | 15 | | Postero midline | Lump | | |
| Bhola N et al., [19] | 2014 | F | 14 | 1.5 | Anterolateral ventral | Lump | Transoral | 12 |
| Moreno-García C et al., [1] | 2014 | F | 13 | 2 | Anterior/ventral | Lump | Lip split/mandibulotomy | 12 |
| Mathai et al., | Present case | M | 14 | 1 | Anterior | Lump | Transoral | 12 |
Schwannomas present as submucosal, painless, encapsulated neoplasms arising from Schwann cells of cranial, peripheral or autonomic nerve neural sheath [3,20-22]. In head and neck region, the commonest nerve involved is the 8th nerve, followed by 5th, 7th, 12th nerve and rarely 9th, 10th and 11th cranial nerves. Within the tongue, schwannomas are of an average size of 2.5 centimeter and can originate from hypoglossal, glossopharyngeal or lingual nerve. Intraoral schwannoma, apart from tongue occur in palate, mouth floor, buccal mucosa, gingiva, lip, and vestibule. Usually, they remain asymptomatic till the tumour enlarges in size causing dysphagia, dysphonia, bleeding, infection or ulceration, or they can impinge on the affected nerve causing pain, loss of sensation, motor or sensory loss. The specific functional deficits caused and the area involved may be used to identify the nerves involved. However, in more than 50% of cases, it is difficult to differentiate between tumours of the lingual, hypoglossal, and glossopharyngeal nerves [5]. Schwannomas are commonly solitary, albeit multiple lesions which occur in association with neurofibromatosis in von Recklinghausen’s disease and schwannomatosis with intracranial tumours [1].
Clinically, schwannomas mimic other benign reactive and soft tissue neoplasms including mucocele, traumatic fibroma, neurofibroma, granular cell tumours, haemangiomas, leiomyomas, rhabdomyomas, lymphangiomas, lipomas, and benign salivary gland tumours [23,24]. However, histological differential diagnosis include other neural tumours such as neurofibroma, neuroma, or muscular or fibroblastic origin tumours. An excision biopsy with histopathological evaluation is mandatory for confirmation.
The differentiation between schwannoma and neurofibroma is essential because a ‘solitary’ neurofibroma may be a manifestation of neurofibromatosis that can have malignant transformation in one or more lesion, which is in contrast to the typical biologic behaviour of a schwannoma [24]. Schwannomas have a well-defined capsule and dual pattern of tumour arrangement. In one pattern (Antoni type A), the Schwann cells are arranged in interlacing fascicles, palisades and organoid pattern resulting in Verocay bodies. In the other pattern (Antoni type B), the Schwann cells are loosely packed and embedded in an oedematous stroma. Immunoreactivity for S 100 supports the Schwann cell origin. Long standing cases may show degenerative changes including nuclear atypia, formation of cysts, stromal oedema, xanthomatous change, and fibrosis and sometimes referred to as ‘ancient’ Schwannoma [25]. A rare variant, pseudoglandular schwannoma have also been reported [26]. Neurofibroma, having origin from the fibroblasts of the perineurium, is unencapsulated and comprise of a mixture of Schwann cells, perineurial cells and endoneurial fibroblasts [24]. The absence of large multipolar fibroblasts, smooth muscles, epithelial-myoepithelial elements, adipose tissue, reticulin, and a mucoid matrix distinguishes schwannoma from other similar histologic entities.
Following complete excision, schwannomas carry excellent prognosis. Recurrences and malignant transformation are rarely reported in schwannomas. Risk of malignant transformation varies from 8-10% in head and neck schwannomas, while it is 2.8% in lingual schwannomas [4]. It has been reported that there is increased incidence of recurrence and malignant transformation in oral and maxillofacial schwannomas compared with that of neck [27]. Focal changes of increased cellularity, numerous mitoses, anaplastic cells, and invasiveness suggest malignant transformation. In the present case, excision was complete and patient was completely disease free one year post-surgery.
Diagnostic imaging modalities include ultrasonography, computed tomography, and Magnetic Resonance Imaging (MRI) [2]. The preferred modality is MRI to know accurate tumour size, its relation to surrounding structures, the tumour margins, tumour composition, nerve of origin to reduce postoperative neural deficits and extension or infiltration of the tumour to surrounding structures. On MRI, a schwannoma is smooth, well-demarcated, isointense to muscle on T1-weighted images and homogeneously hyperintense on T2-weighted images without invasion to surrounding structures.
Transoral resection with an attempt to preserve the nerve remains the standard treatment [28]. Lately, carbon dioxide laser excision has also been used to treat base of tongue schwannomas. In the present case, the tumour was removed completely without mucosal damage to avoid recurrence and tongue dysfunction.
Conclusion
Schwannomas are rarely encountered in children and even rarer with the involvement of anterior one-third of tongue as in the present case. A meticulous search for schwannoma or other neural tumours at another site in the body should be performed, lest any associated syndromes be missed. The tumour has non-specific clinical presentation and has to be distinguished with other topographically similar benign oral soft tissue neoplasms. Histopathology remains the gold standard for a definitive opinion as complete surgical excision of the lesion is usually curable without any recurrence. The availability of newer minimally invasive therapeutic modalities adds to the importance of accurate diagnosis.
[1]. Moreno-García C, Pons-García MA, González-García R, Monje-Gil F, Schwannoma of tongueJ Maxillofac Oral Surg 2014 13:217-21.10.1007/s12663-010-0101-024822018 [Google Scholar] [CrossRef] [PubMed]
[2]. Naidu GS, Sinha SM, Schwannoma of the tongue: an unusual presentation in a childIndian J Dent Res 2010 21:457-59.10.4103/0970-9290.7079020930365 [Google Scholar] [CrossRef] [PubMed]
[3]. Husain S, Yunus MR, Ramli R, Athar PP, Schwannoma of the tongue in a ten-year old childJ Pak Med Assoc 2011 61:500-01. [Google Scholar]
[4]. Lira RB, Gonçalves Filho J, Carvalho GB, Pinto CA, Kowalski LP, Lingual schwannoma: Case report and review of the literatureActa Otorhinolaryngol Ital 2013 33:137-40. [Google Scholar]
[5]. Abreu I, Roriz D, Rodrigues P, Moreira Â, Marques C, Alves FC, Schwannoma of the tongue-a common tumour in a rare location: A case reportEur J Radiol Open 2017 4:1-3.10.1016/j.ejro.2017.01.00228203620 [Google Scholar] [CrossRef] [PubMed]
[6]. Lee EY, Kim JJ, Seok H, Lee JY, Schwannoma of the tongue: A case report with review of literatureMaxillofac Plast Reconstr Surg 2017 39:1710.1186/s40902-017-0116-228730146 [Google Scholar] [CrossRef] [PubMed]
[7]. Manna F, Barbi E, Murru F, Bussani R, Lingual schwannoma in paediatric patientsJ Craniofac Surg 2012 23:e454-56.10.1097/SCS.0b013e318262d9c722976705 [Google Scholar] [CrossRef] [PubMed]
[8]. Craig D, Neurilemmoma of the tongueArch Dis Child 1964 39:297-98.10.1136/adc.39.205.29714169464 [Google Scholar] [CrossRef] [PubMed]
[9]. Akimoto Y, Yamamoto H, Nishimura H, Komiya M, Kaneko K, Neurilemmoma in the oral cavityJ Nihon Univ Sch Dent 1987 29:203-05.10.2334/josnusd1959.29.2033323425 [Google Scholar] [CrossRef] [PubMed]
[10]. Cinar F, Cinar S, Harman G, Schwannoma of the tip of the tongue in a childPlast Reconstr Surg 2004 114:1657-58. [Google Scholar]
[11]. Bassichis BA, McClay JE, Pedunculated neurilemmoma of the tongue baseOtolaryngol Head Neck Surg 2004 130:639-41.10.1016/j.otohns.2003.09.02915138434 [Google Scholar] [CrossRef] [PubMed]
[12]. Nakasato T, Kamada Y, Ehara S, Miura Y, Multilobular neurilemmoma of the tongue in a childAm J Neuroradiol 2005 26:421-23. [Google Scholar]
[13]. Hsu YC, Hwang CF, Hsu RF, Kuo FY, Chien CY, Schwannoma (neurilemmoma) of the tongueActa Otolaryngol 2006 126:861-65.10.1080/0001648050052721916846930 [Google Scholar] [CrossRef] [PubMed]
[14]. Enoz M, Suoglu Y, Ilhan R, Lingual schwannomaJ Cancer Res Ther 2006 2:76-78.10.4103/0973-1482.2585617998681 [Google Scholar] [CrossRef] [PubMed]
[15]. Pereira LJ, Pereira PP, dos Santos Jde P, Reis Filho VF, Dominguete PR, Pereira AA, Lingual schwannoma involving the posterior lateral border of the tongue in a young individual: Case reportJ Clin Paediatr Dent 2008 33:59-62.10.17796/jcpd.33.1.h131208u28306576 [Google Scholar] [CrossRef]
[16]. Karaca CT, Habesoglu TE, Naiboglu B, Habesoglu M, Oysu C, Egeli E, Schwannoma of the tongue in a childAm J Otolaryngol 2010 31:46-48.10.1016/j.amjoto.2008.09.010 [Google Scholar] [CrossRef]
[17]. Cigdem T, Tulay E, Baris N, Mehmet H, Cagatay O, Erol E, Schwannoma of the tongue in a childAm J Otolaryngol Head and Neck Med and Surg 2010 31:46-48. [Google Scholar]
[18]. Lukšić I, Müller D, Virag M, Manojlović S, Ostović KT, Schwannoma of the tongue in a childJ Craniomaxillofac Surg 2011 39:441-44.10.1016/j.jcms.2010.10.00421041099 [Google Scholar] [CrossRef] [PubMed]
[19]. Bhola N, Jadhav A, Borle R, Khemka G, Bhutekar U, Kumar S, Schwannoma of the tongue in a paediatric patient: a case report and 20-year reviewCase Rep Dent 2014 2014:78076210.1155/2014/78076225126428 [Google Scholar] [CrossRef] [PubMed]
[20]. Gallo WJ, Moss M, Shapiro DN, Gaul JV, Neurilemoma: Review of the literature and report of five casesJ Oral Surg 1977 35:235-36. [Google Scholar]
[21]. Chiapasco M, Ronchi P, Scola G, Neurilemmoma (schwannoma) of the oral cavity. A report of 2 clinical casesMinerva Stomatol 1993 42:173-78. [Google Scholar]
[22]. Mevio E, Gorini E, Lenzi A, Migliorini L, Schwannoma of the tongue: one case reportRev Laryngol Otol Rhinol (Bord) 2002 123:259-61. [Google Scholar]
[23]. Nair V, Dey B, Deshpande AH, Nigam JS, Cystic schwannoma of tongue masquerading as mucocele: A cytological pitfallJ Cytol 2018 35:125-26.10.4103/JOC.JOC_50_1729643663 [Google Scholar] [CrossRef] [PubMed]
[24]. Martins MD, Anunciato de Jesus L, Fernandes KP, Bussadori SK, Taghloubi SA, Martins MA, Intra-oral schwannoma: Case report and literature reviewIndian J Dent Res 2009 20:121-25.10.4103/0970-9290.4905919336874 [Google Scholar] [CrossRef] [PubMed]
[25]. Nakayama H, Gobara R, Shimamoto F, Kajihara H, Ancient schwannoma of the oral floor and ventricular portion of the tongue: A case report and review of the literatureJpn J Clin Oncol 1996 26:185-88.10.1093/oxfordjournals.jjco.a0232058656562 [Google Scholar] [CrossRef] [PubMed]
[26]. Deng A, Petrali J, Jaffe D, Sina B, Gaspari A, Benign cutaneous pseudoglandular schwannoma: A case reportAm J Dermatopathol 2005 27:432-35.10.1097/01.dad.0000175534.73110.4e16148415 [Google Scholar] [CrossRef] [PubMed]
[27]. Kun Z, Qi DY, Zhang KH, A comparison between the clinical behaviour of neurilemmomas in the neck and oral and maxillofacial regionJ Oral Maxillofac Surg 1993 51:769-71.10.1016/S0278-2391(10)80419-7 [Google Scholar] [CrossRef]
[28]. Sitenga JL, Aird GA, Nguyen A, Vaudreuil A, Huerter C, Clinical features and surgical treatment of schwannoma affecting the base of the tongue: A systematic reviewInt Arch Otorhinolaryngol 2017 21:408-13.10.1055/s-0037-159860929018506 [Google Scholar] [CrossRef] [PubMed]