Case Report
A 47-year-old female patient came to the clinic with a chief complaint of swelling on the lower lip on the right side for the past seven years. Patient gives a history of swelling which showed gradual increase in size with no history of rupture or any associated pain. Patient also gave a history of trauma due to occasional biting.
On systemic examination, all vital signs were within normal limits. On external examination, no abnormalities were detected. Patient gave a history of siddha treatment for Psoriasis. On inspection, a circumscribed submucosal swelling was evident on the right side of the lower lip measuring about 2.5 cm×1 cm involving the labial mucosa and extending till the vermillion border of lip, corresponding to 11,12,13.
Swelling appeared smooth and glossy, mildly translucent and sessile in nature. Colour of the swelling was similar to the adjacent normal mucosa and no surface changes were seen [Table/Fig-1].
Extra-oral Circumscribed swelling on the right side of the lower lip.

On palpation, all the inspectory findings were confirmed and the swelling was slightly movable and mildly compressible in nature with mild pain. On the basis of clinical examination a differential diagnosis of Fibroma, Mucocele, and Haemangioma were considered.
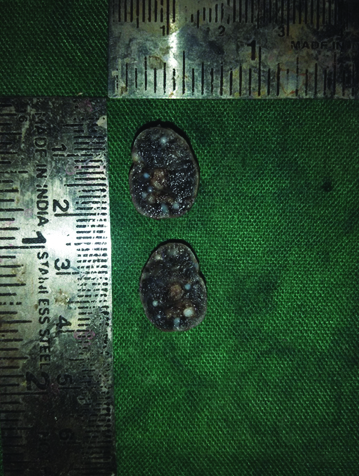
Complete blood count was done and all values were within normal limits. Excisional Biopsy was performed under local anaesthesia and sutures were placed. The gross specimen was oval in shape with well-circumscribed borders and was firm in consistency with irregular surface. The cut section of the specimen showed that the centre was blackish with few white elevated areas and the periphery was brown in colour [Table/Fig-2].
Macroscopic examination of specimen received in 10% formalin.
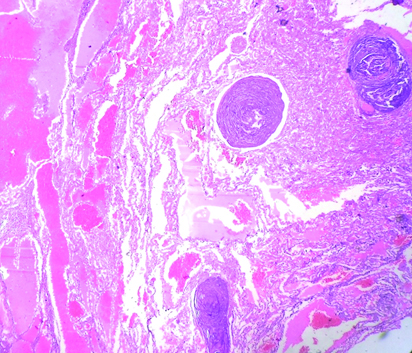
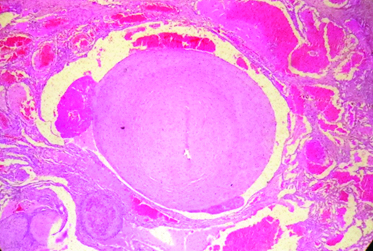
The microscopic features showed a nodular lesion with thin-walled, dilated and congested blood vessels, containing fibrin thrombi in the lumen. Foci of organisation and calcification were seen. Areas of hyalinisation and calcification were also seen. In few areas, clusters of lymphocytes were also seen [Table/Fig-3,4]. Based on the clinical and histopathological findings, a final diagnosis of haemangioma with multiple phleboliths was given.
Histopathology shows thin walled, dilated and congested blood vessels, containing fibrin thrombi in the lumen (H&E-4X).
Histopathology shows organising thrombus with dense basophilic calcifications at the centre surrounded by onion ring pattern of lamellar arrangement (H&E-10X).
Discussion
Centuries ago it was believed that vascular birthmark were due to “maternal impression”. Hence these lesions were termed as nevus maternus and stigma metrocelis, implying the mother responsible for such lesions [1].
Biological classification was first published in 1982 by Mulliken JB and Glowacki J [2]. They divided vascular anomalies into two major categories: tumors and malformations. This classification was later adopted by the International Society for the Study of Vascular Anomalies (ISSVA) in their first workshop held in Rome during June 1996. This classification system is now widely accepted to properly diagnose and manage vascular anomalies [3].
Haemangioma and vascular malformations of the maxillofacial regions have shown established correlation with the presence of multiple phleboliths. However, isolated or solitary phleboliths in the oral mucosa occurs due to regression of childhood haemangioma or trauma. Usually, they are associated with intravascular calcifications called phleboliths, which are basically calcified thrombus formed due to stasis of blood in the vascular channels [4]. Phlebolith formation, is reported as a predictable feature of haemangioma and was first described in the splenic vein by Canstatt in the year 1843 [5,6] while this was first described in the maxillofacial location by Kirmission in 1905 [7].
Hemangiomas are defined as benign, vascular lesions, which are congenital in origin, developing from abnormally differentiated blood vessels [8]. They are generally called vascular tumour of infancy [9]. They are usually biphasic, that is they have a phase of rapid growth during the first year of life which is called as proliferating phase and then the slow regression phase called the involuting phase (between 10 and 14 months of age) which may continue upto 10 years of age [1].
The exact aetiology is unknown, but repeated trauma, excess contraction of muscle and hormones are thought to play an important role in the lesion progress [10].
Intramuscular Haemangioma (IMH) represents less than 1% of all haemangioma, most commonly found in the skeletal muscles of limbs or the trunk. 10% to 15% of IMH is seen in the maxillofacial region, mainly in the masseter, sternomastoid and trapezius muscles [11].
Haemangioma presents with reddish-blue discoloration and has hyperthermic change, the skin over the haemangioma shows hypervascularity. Sometimes, haemangioma presents with thrills, bruits or compressibility. But due to the thickening and fibrosis of the superficial muscle layer, the clinical signs of IMH are hidden [12]. The predominant complaint is the presence of a slowly enlarging mass.
Diagnosis of this lesion is complicated due to the rare incidence of the lesion and the lack of typical clinical findings. Only 8% of the cases have definitive preoperative diagnosis [13]. The differential diagnosis being benign muscular hypertrophy, neoplasms in the parotid and congenital cysts [14].
Phleboliths are defined as pathologic, calcified vascular thrombi which are formed due to stasis of blood or even trauma usually associated with other vascular lesions, as vascular malformations (VM) [15]. They can also be caused by an injury to a vessel wall or due to stasis of blood (stasis can result because of tortuous blood vessels within a haemangioma) [16]. The injury can result in damage to the tunica intima which is followed by healing. A protective thrombus is formed as a part of this healing process. This thrombus undergoes slow calcification and extends to the periphery with concomitant lamellar fibrosis. Thus, the thrombus formation is favoured by two factors, slowing of blood and stagnation of blood flow, which further leads to calcification of thrombus and finally results in formation of phleboliths. Phleboliths mainly consists of mixture of calcium phosphate salts and calcium carbonate, which are deposited at the centre and mineralisation extends to the periphery also. The fibrous component always attaches to the developing phleboliths, and this fibrous component in turn, becomes calcified [17]. Repetition of the process causes a layering effect giving phleboliths the usual concentric ring or onion-like appearance; this suggests the growth mechanism given by Ribbert H in the year 1917 [17].
Radiographically, they appear as multiple round or oval laminated bodies which can either have a radiopaque or radiolucent laminated cores that corresponds to the alternating high and low mineral content laminations [1].
Phleboliths are usually incidental findings and has no typical subjective symptoms, they are found during routine imaging or during studies of vascular lesions. Phleboliths in the maxillofacial region are usually multiple, varying in size (from 1 to 5 mm in diameter to 1 cm or even larger) and distributed randomly, and they are mainly related with IMHs or Vascular Malformations (VMs). Phleboliths are most commonly found in the pelvic areas, mainly within the prostatic, uterine, or the intestinal veins (due to stress injury during defecation), next site of occurrence is the head and neck region which is about 15% to 25% of IMHs [18]. Phleboliths in the oral cavity occurs mostly in the first and third decade of life, with females (48.28%) and males (51.72%). Sometimes these phleboliths also involve the masticatory process (27.6%) [19,20].
Standard radiographs are essential diagnostic tool in diagnosing the phleboliths. Other non-ionising techniques such as Magnetic Resonance Imaging (MRI), Computerised Tomography (CT) and ultrasound; can provide good images demonstrating the location and extent of the lesions and also help in preoperative diagnosis of IMHs [19]. They can also be found in periapical regions near dental structures in a plain radiograph.
The head and neck phleboliths needs to be differentiated from other calcifications occurring in the same area. Thus, the differential diagnosis being sialolithiasis, tonsilloliths, osteomas, carotid artery calcifications, cysticercosis, miliary skin calcified lymph nodes [15,19], Metastatic and dystrophic calcifications and calcified cutaneous acnes [21].
Occasionally, phleboliths are seen in association with some syndromes like the Sturge-Weber syndrome, the Klippel-Trenaunay-Weber syndrome, Maffucci syndrome, and the rubber-bleb syndrome [21].
Phleboliths located in salivary gland regions are clinically misdiagnosed as a salivary gland disease or a sialolith (mainly in cases of intermittent swelling). Sialography acts as diagnostic tool in these cases. The [Table/Fig-5] below shows the difference between salivary calculus and phleboliths. Sialolith cause pain and phleboliths are painless.
Radiological differences between salivary calculus and phleboliths.
| Salivary calculus | Phleboliths |
|---|
| 1) Uniformly radiopaque. Can be laminated if large, especially in submandibular gland. | 1) Usually laminated with radiopaque centre or nucleus, sometimes radiolucent centre. |
| 2) Usually takes the shape of the duct, thus they are elongated. | 2) Usually circular |
| 3) They are usually 1-2 in number | 3) Usually multiple in number. |
| 4) Sialography shows filling defect at site of calculus. | 4) Sialography shows phleboliths to be outside the duct system. |
Other than imaging, final diagnosis can be obtained by performing a biopsy followed by microscopic examination, commonly Haematoxylin and Eosin (H&E) is used. Microscopically these phleboliths are seen in the vessel as concentric calcification exhibiting onion like pattern. Immunohistochemistry studies acts as an adjuvant (using CD34 and SMA for vascular endothelium and smooth muscle wall positivity), for coming to a final diagnosis [20].
Conclusion
Cases of Phleboliths in intraoral vascular malformations are usually rarely seen. Haemangioma with phleboliths should be identified from the differential diagnosis for lesion appearing as swellings like sialolithiasis, based on the clinical examination, imaging, histopathological and Immunohistochemical methods.
[1]. Scolozzi P, Laurent F, Lombardi T, Richter M, Intraoral venous malformation presenting with multiple phlebolithsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2003 96(2):197-200.10.1016/S1079-2104(03)00098-2 [Google Scholar] [CrossRef]
[2]. Mulliken JB, Glowacki J, Hemangiomas and vascular malformations in infants and children a classification based on endothelialcharacteristicsPlast Recontr Surg 1982 69:412-20.10.1097/00006534-198203000-000027063565 [Google Scholar] [CrossRef] [PubMed]
[3]. Workshop I, The B, ISSVA classification for vascular anomalies Vascular tumors ISSVA classification of vascular tumors 2014;(April) [Google Scholar]
[4]. George R, Donald PM, Gopu S, Haemangioma with phlebolith on the upper lip: a rare case report 2015 1(9):55-56. [Google Scholar]
[5]. Amin R, Hegde P, Shetty P, Makannavar JH, Intraoral venous malformation with phleboliths–a case report with review of the literatureInt J Adv Res 2017 5(2):663-66.10.21474/IJAR01/3198 [Google Scholar] [CrossRef]
[6]. O’Riordan B, Phleboliths and salivary calculiBr J Oral Surg 1974 12(2):119-31.10.1016/0007-117X(74)90120-6 [Google Scholar] [CrossRef]
[7]. Ikegami N, Nishijima K, Hemangioma of the buccal pad with phlebolithiasis: report of a caseActa Med Okayama 1984 38(1):79-87. [Google Scholar]
[8]. Park JW, Kim C, Moon CW, Kim C, Intramuscular hemangioma in buccal cheek: a case reportJ Korean Assoc Oral Maxillofac Surg 2017 :262-66.10.5125/jkaoms.2017.43.4.26228875141 [Google Scholar] [CrossRef] [PubMed]
[9]. Mohan RPS, Dhillon M, Gill N, Intraoral venous malformation with phlebolithsSaudi Dent J [Internet] 2011 23(3):161-63.Available from: http://dx.doi.org/10.1016/j.sdentj.2011.02.00310.1016/j.sdentj.2011.02.00324151422 [Google Scholar] [CrossRef] [PubMed]
[10]. Mandel L, Surattanont F, Clinical and imaging diagnoses of intramuscular hemangiomas: the wattle sign and case reportsJ oral Maxillofac Surg 2004 62(6):754-58.10.1016/j.joms.2003.05.02215170294 [Google Scholar] [CrossRef] [PubMed]
[11]. Kanaya H, Saito Y, Gama N, Konno W, Hirabayashi H, Haruna S, Intramuscular hemangioma of masseter muscle with prominent formation of phleboliths: a case reportAuris Nasus Larynx 2008 35(4):587-91.10.1016/j.anl.2007.11.00318207684 [Google Scholar] [CrossRef] [PubMed]
[12]. Altuğ HA, Büyüksoy V, Okçu KM, Doğan N, Hemangiomas of the head and neck with phleboliths: Clinical features, diagnostic imaging, and treatment of 3 casesOral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology 2007 103(3):60-64.10.1016/j.tripleo.2006.09.00617188913 [Google Scholar] [CrossRef] [PubMed]
[13]. Clemis JD, Briggs DR, Changus GW, Intramuscular hemangioma in the head and neckCan J Otolaryngol 1975 4(2):339-46. [Google Scholar]
[14]. Demir Z, Öktem F, Çelebioğlu S, Rare case of intramasseteric cavernous hemangioma in a three-year-old boy: a diagnostic dilemmaAnn Otol Rhinol Laryngol 2004 113(6):455-58.10.1177/00034894041130060715224828 [Google Scholar] [CrossRef] [PubMed]
[15]. Mandel L, Perrino MA, Phleboliths and the vascular maxillofacial lesionJ Oral Maxillofac Surg 2010 68(8):1973-76.Available from: http://dx.doi.org/10.1016/j.joms.2010.04.00210.1016/j.joms.2010.04.00220542619 [Google Scholar] [CrossRef] [PubMed]
[16]. Shemilt P, The origin of phlebolithsBr J Surg 1972 59(9):695-700.10.1002/bjs.18005909034341799 [Google Scholar] [CrossRef] [PubMed]
[17]. Ribbert H, Die phlebolithenVirchows Arch 1917 223(3):339-50.10.1007/BF02034326 [Google Scholar] [CrossRef]
[18]. Morris SJ, Adams H, Paediatric intramuscular haemangiomata-don’t overlook the phlebolith! Br J Radiol 1995 68(806):208-11.10.1259/0007-1285-68-806-2087735755 [Google Scholar] [CrossRef] [PubMed]
[19]. Zengin AZ, Celenk P, Sumer AP, Intramuscular hemangioma presenting with multiple phleboliths: A case reportOral Surg Oral Med Oral Pathol Oral Radiol 2013 115(1):e32-36.Available from: http://dx.doi.org/10.1016/j.oooo.2012.02.03210.1016/j.oooo.2012.02.03223217548 [Google Scholar] [CrossRef] [PubMed]
[20]. Gouvêa Lima GDM, Moraes RM, Cavalcante ASR, Carvalho YR, Anbinder AL, An Isolated Phlebolith on the Lip: An Unusual Case and Review of the LiteratureCase Rep Pathol 2015 2015:507840Available from: http://www.hindawi.com/journals/cripa/2015/507840/10.1155/2015/50784026266070 [Google Scholar] [CrossRef] [PubMed]
[21]. Nagaraja A, Kumar NG, Kumar BJ, Naik RM, Sangineedi YJ, A solitary phlebolith in the buccal mucosa: Report of a rare entity and clinicopathologic correlationJ Contemp Dent Pract 2016 17(8):706-10.10.5005/jp-journals-10024-191627659092 [Google Scholar] [CrossRef] [PubMed]