Atherosclerotic Cardiovascular Disease (CVD) remains the leading cause of premature death worldwide. Age, gender, hypertension, smoking, dyslipidemia, and diabetes mellitus are the well-accepted major risk factors for CVD development [1]. These risk factors can be modified by changes in lifestyle and the use of medications. Few algorithms, such as the Framingham Risk Score (FRS), Systematic Coronary Risk Evaluation (SCORE), Reynolds, QRESEARCH cardiovascular risk (QRISK), and the assessing cardiovascular risk to Scottish Intercollegiate Guidelines Network to assign preventative treatment (ASSIGN) score are available to assess the risk of CAD [2-9].
The CHADS2 score is used to decide for the need of anticoagulation/antiplatelet medication in patients with non-valvular atrial fibrillation for prevention of stroke. It is simple and has been validated by many studies described in the National Registry of Atrial Fibrillation [10]. A high CHADS2 score is indicative of greater stroke risk. In clinical use, the CHADS2 score has been replaced by the CHA2DS2-VASc score, which provides better stratification of low-risk patients [11]. Both the CHADS2 and CHA2DS2-VASc scoring schemes are easily remembered and applied by physicians in clinical practice. As they include similar risk factors for the development or presence of CAD, authors believed that they could also be used to predict CAD severity.
In this study, a new score, termed the CHA2DS2-VASc-HSLp(a) score to increase the likelihood of determining CAD severity was formulated. This scoring system includes Hyperlipidemia (HL), smoking and Lipoprotein a {Lp(a)} as other major risk factors for CAD, in addition to using male rather than female gender. As in comparison to FRS, CHA2DS2-VASc is easily memorable by the physicians, but it is used for stroke risk evaluation of non-valvular atrial fibrillation and in developing countries like India, hyperlipidemia, smoking and Lpa are independent risk factors of CAD and to test whether adding these risk factors to CHA2DS2-VASc score could be a better predictor of CAD, authors created a new scoring system i.e. CHA2DS2-VASc-HSLp(a) score. Authors compared the FRS, CHA2DS2-VASc, and CHA2DS2-VASc-HSLp(a) scores as multivariable risk assessment methods in patients who were undergoing Coronary Angiography (CAG) to identify who is at risk of the severe CAD. There is a more precise scoring system for severity of CAD involvement known as Gensini score [12], authors compared all these three scores in the study for correlation with Gensini score.
Materials and Methods
This was a prospective study on diagnostic accuracy (first the risk score was calculated and then coronary angiography was performed) conducted at Sir Sunder Lal Hospital, IMS, BHU, Varanasi, Uttar Pradesh, India. The study included 516 patients of suspected CAD on the basis of symptoms and result of the previous test, undergoing coronary angiography admitted in cardiology department from May 2015 to October 2015. Study was approved by Institutional Ethics Committee of IMS, BHU, Varanasi vide Ethical Clearance Number, Dean/2014-15/EC/1200.
Study population was derived applying inclusion and exclusion criteria on the target population. Signed written informed consent was taken from each of the patients for participation in the study. All patients in this study underwent routine investigations before angiography.
Sample Size
In view of the fact that angiography will be carried only among the suspected cases, so normal subjects are likely to be very few in numbers (<10%), hence it was decided to take a total sample with normal and abnormal angiography in the ratio of 1:10. Since, scores assigned to each subject were non-normal with unknown distribution, the sample size was calculated with minimum Asymptotic Relative Efficiency (ARE) considering level of significance (α=0.05), power of the test (1-β=0.90) and effect size as 0.6 with allocation ratio 1:10. The software G*Power 3.1.9.2 was used and the minimum sample size needed to be was obtained as 31 subjects with normal angiography and 305 subjects with abnormal angiography. Thus, a total of 336 cases were required. Since, all the suspected subjects consenting for angiography were considered, so to get a minimum of 31 normal subjects, the procedure was continued till 31 normal subjects were obtained. Thus, total subjects in the sample including 31 with normal angiography rose to 516 because of higher number of subjects with abnormal angiography.
Initial Evaluation
Complete Blood Count (CBC)
Renal function test
Lipid profile
Lipoprotein-(a) level
Fasting blood sugar
Two-Dimensional echocardiography
Inclusion Criteria were age >18 years, patient undergoing coronary angiography and competency to give consent. Exclusion Criteria were previous PTCA/CABG (Percutaneous Transluminal Coronary Angioplasty/Coronary Artery Bypass Grafting), presence of acute heart failure, acute ischaemic stroke or Transient Ischaemic Attack (TIA), pregnancy and marked anaemia (Hb <8 g/dL).
Study Procedure
In this study, a thorough history with regards to smoking, Diabetes Mellitus (DM), Cerebrovascular Accidents/Transient Ischaemic Accidents (CVA/TIA), and treatment for Hypertension (HTN), treatment or symptoms of Congestive Heart Failure (CHF) were taken. DM was defined as a previous diagnosis and/or fasting blood glucose >126 mg/dL or the use of anti-diabetic medications [13]. HTN was defined as repeated measurements of systolic blood pressure >140 mmHg, diastolic >90 mmHg or chronic treatment with anti-hypertensive medications [14]. Hyperlipidemia (HL) was considered to be LDL-C above the target level according to the National Cholesterol Education Program-3 recommendations or the use of lipid-lowering medications [7]. Cigarette smoking was defined as smoking >10 cigarettes a day for at least one year without a quit attempt. Family history was defined as the presence of coronary artery disease or sudden cardiac death in a male first-degree relative aged <55 years or in a female first-degree relative aged <65 years. Heart failure referred to documented moderate-to-severe systolic dysfunction {i.e., Heart Failure with reduced Ejection Fraction (HF-rEF)} or patients with recent decompensated Heart Failure requiring hospitalisation, irrespective of Ejection Fraction {i.e. both HF-rEF and Heart Failure with preserved Ejection Fraction (HF-pEF)}[15]. Vascular disease [16] referred to myocardial infarction, complex aortic plaque, and Peripheral Artery Disease (PAD), including prior revascularisation, amputation due to PAD or angiographic evidence of PAD. Raised lipoprotein-a was defined as level >25 mg/dL [17].
Coronary angiogram was performed using the Judkins technique. Significant CAD was diagnosed if there was 50% diameter stenosis in at least one major epicardial coronary artery. The severity of CAD was determined by the number of significantly diseased coronary arteries. Vessel disease was defined as the presence of 50% luminal diameter stenosis in at least one major coronary artery. Multivessel coronary disease was defined as the presence of 50% luminal diameter stenosis involving at least two major epicardial coronary arteries. Left main coronary artery narrowing of 50% was considered as 2-vessel disease [18]. The stenosis <50% was considered mild CAD. The Gensini score [12] was calculated for each patient from the coronary angiogram by assigning a severity score to each coronary stenosis as 1 for 1% to 25% narrowing, 2 for 26% to 50%, 4 for 51% to 75%, 8 for 76% to 90%, 16 for 91% to 99%, and 32 for a completely occluded artery. The score is then multiplied by a factor according to the importance of the coronary artery. The multiplication factor was 5 for a left main coronary artery, 2.5 for proximal left anterior descending artery and proximal circumflex artery, 1.5 for a mid-left anterior descending artery, and 1 for distal left anterior descending artery, mid or distal circumflex artery, and right coronary artery.
Serum Lp(a) estimation was performed using quantitative Latex-enhanced Immunoturbidimetric test using human Lp(a) kit (Human Gesselschaft, Weisbaden, Germany). Strict external quality control using sera with known values was performed to validate the results.
The CHADS2 nomenclature represents congestive heart failure (C), HT (H), age (A), DM (D), and stroke (S). The CHADS2 score was calculated by assigning 1 point each for the presence of chronic heart failure, HT, age 75 years, and DM and by assigning 2 points for history of stroke or TIA. The CHA2DS2-VASc score is a modification of the CHADS2 score and extends the latter by including additional common stroke risk factors including vascular disease (V), age 65 to 74 years (A), and female gender (as a sex category {Sc}). In the CHA2DS2-VASc score, age 75 years (A2) is assigned 2 points. The CHA2DS2-VASc-HSLp(a) score comprises Hyperlipidemia (HL), smoking and lipoprotein-a (Lpa) in addition to the components of the CHA2DS2-VASc score and male gender instead of female gender. The maximum CHA2DS2-VASc and CHA2DS2-VASc-HSLp(a) scores were 9, and 12, respectively [Table/Fig-1].
The new CHA2DS2-VASc-HSLp(a) scoring System. Maximum score 12 points.
| Code | Risk factor | Points |
|---|
| C | Congestive heart failure | 1 |
| H | Hypertension | 1 |
| A2 | Age >75 yrs | 2 |
| D | Diabetes mellitus | 1 |
| S2 | Previous stroke or TIA | 2 |
| V | Vascular disease | 1 |
| A | Age 65-74 yrs | 1 |
| Sc | Sex category (male gender) | 1 |
| H | Hyperlipidemia | 1 |
| S | Smoker | 1 |
| Lp(a) | Lipoprotein-a level > 25 mg/dL | 1 |
CHA2DS2-VASc, CHA2DS2-VASc-HSLp(a) scores and Framingham Coronary Heart Disease Risk Scores were calculated before angiography. After CAG, Gensini score was calculated to stratify severity of coronary artery stenosis. Different risk scores were compared with coronary artery stenosis severity determined by Gensini scoring system and number of diseased vessels.
The study was approved by the local Ethics Committee on the basis of strict maintenance of participant anonymity, and individual informed consent was obtained from all subjects.
Statistical Analysis
Continuous data were presented as mean±SD and/or median (minimum to maximum). Kruskal-Wallis tests were used to compare the three groups. Differences in continuous variables between two groups were determined by Mann-Whitney U-test. To predict cut-off value of Gensini score for FRS, CHA2DS2-VASc and indicate higher risk of CAD, Receiver Operating Characteristics (ROC) curve analysis was performed. The ROC curve was also used to demonstrate the sensitivity and specificity of CHA2DS2-VASc-HSLp(a) score and its cut-off value for predicting severe CAD. A p-value <0.05 was considered as significant. Statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS 16.0) for Windows (SPSS Inc., Chicago, Illinois).
Results
The study included 400 male and 116 female patients (M:F ratio=1.0:0.29). A 2.75% of male patients had normal coronaries as compared to 17.24% of similar findings in female patients. Single vessel disease affected 33.25% of males and only 12.1% of females. One or more vessel disease was seen in 97.25% of males as compared to 82.75% of females in present study population. This difference was significant with a p-value of <0.001 which clearly states that the coronary vessel disease had a sex predilection and affects males more than females.
Correlation of various baseline characteristics with severity of CAD is depicted in [Table/Fig-2].
Correlation of baseline characteristics with severity of CAD.
| Variables | Normal Coronaries | SVD | DVD | TVD | p-value |
|---|
| Age (years) mean±SD | 54.19±5.27 | 53.45±11.66 | 58.03±6.78 | 56.33±10.78 | 0.06 |
| SBP (mmHg) mean±SD | 119.48±11.67 | 140.71±19.55 | 143.97±21.63 | 135.45±20.20 | <0.001 |
| DBP (mmHg) mean±SD | 76.52±6.96 | 86.42±10.96 | 85.17±12.74 | 82.00±8.67 | <0.001 |
| LDL (mg/dL) mean±SD | 81.52±38.12 | 90.73±25.05 | 117.79±29.18 | 112.75±45.08 | <0.001 |
| Lipoprotein(a) (mg/dL) median (minimum to maximum) | 17.9 (10.5-37) | 16.90 (12.4-29.0) | 21.3 (12-58) | 33.5 (24-42) | <0.001 |
SVD: Single vessel disease; DVD: Double vessel disease; TVD: Triple vessel disease; SBP: Systolic blood pressure; DBP: Diastolic blood pressure
Mean FRS [Table/Fig-3] in present study was 5.10±4.585 with median 1 (1-10) for normal coronaries and gradually increased from 1% to 20% as severity of CHD increases from SVD to multi-vessel disease with significant association (p<0.001).
Comparison of the FRS, CHA2DS2-VASc, and CHA2DS2-VASc-HSLP(a) scores against number of diseased vessels.
| Variables | Normal Coronaries | SVD | DVD | TVD | p-value |
|---|
| FRS* | 5.10±4.581 (1-10) | 9.38±7.805 (3-12) | 14.29±8.7920 (10-20) | 11.72±8.3012 (2-20) | <0.001 |
| Total CHA2DS2-VASc Score* | 0.55±0.501 (0-1) | 1.77±1.052 (1-3) | 2.05±1.582 (1-3) | 2.19±1.042 (1-3) | >0.05 |
| Total CHA2DS2-VASc-HSLp(a) score* | 1.00±1.091 (0-2) | 2.49±1.243 (1-3) | 3.08±1.604 (1-4) | 3.66±1.384 (3-5) | <0.001 |
*Data are expressed as mean±SD and median (minimum to maximum).
SVD: Single vessel disease; DVD: Double vessel disease; TVD: Triple vessel disease
In the present study, the mean CHA2DS2-VASc score in patients with normal coronaries, SVD, DVD, and TVD groups were 0.55±0.506, 1.77±1.054, 2.05±1.584 and 2.19±1.048 respectively. This difference between the groups was statistically not significant (p>0.05).
The mean CHA2DS2-VASc-HSLp(a) score in patients with normal coronaries, SVD, DVD, and TVD groups were 1.00±1.095, 2.49±1.246, 3.08±1.609 and 3.66±1.386 respectively. This difference between the groups was highly statistically significant (p<0.001).
After analysing the entire study population [Table/Fig-4] based on FRS, CHA2DS2-VASc, and CHA2DS2-VASc-HSLp(a) scores, patients with FRS ≥10, CHA2DS2-VASc scores of ≥2 and CHA2DS2-VASc-HSLp(a) score of ≥2 had significantly higher Gensini scores with p-value <0.001.
Comparison of Gensini score according to FRS, CHA2DS2-VASc, and CHA2DS2-VASc-HSLP(a) subgroups.
| FRS <10 | FRS >10 | p-value |
|---|
| Gensini score | 42.71±35.5629(8-60) | 64.51±41.9461(29-104) | <0.001 |
| CHA2DS2-VASc score <2 | CHA2DS2-VASc score ≥2 | p-value |
| Gensini score | 36.18±33.7029(5-56) | 67.47±40.3861(30-108) | <0.001 |
| CHA2DS2-VASc-HSLp(a) score <2 | CHA2DS2-VASc-HSLp(a) score ≥2 | p-value |
| Gensini score | 25.34±27.4616(3-54) | 64.791±39.8860(29-104) | <0.001 |
*Data are expressed as mean±SD and median (minimum to maximum).
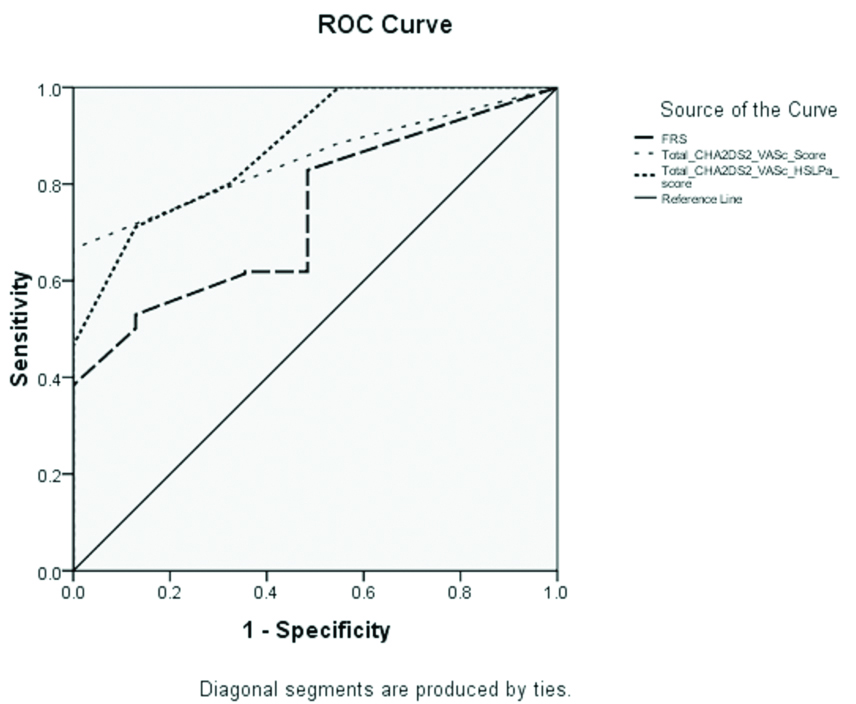
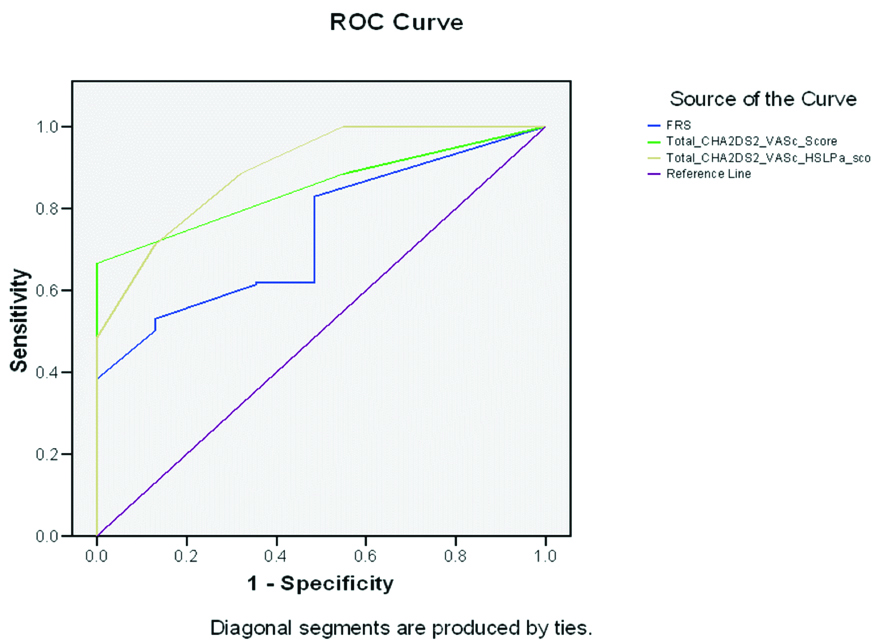
According to [Table/Fig-5] for the prediction of severe CAD, the cut-off value of FRS was 7.00 with a sensitivity of 61.9% and specificity of 64.5% (AUC 0.738, 95% confidence interval 0.665 to 0.811, p<0.001) and the cut-off value of CHA2DS2-VASc score was 2.0 with a sensitivity of 66.6% and specificity of 100% (AUC 0.851, 95% confidence interval 0.809 to 0.893, p<0.001) whereas the cut-off value of CHA2DS2-VASc-HSLp(a) score was 2.0 with a sensitivity of 80% and specificity of 67.7% (AUC 0.802, 95% confidence interval 0.822 to 0.932, p<0.001). The AUC comparisons of these scoring systems were performed based on significant CAD [Table/Fig-6]. According to these results, the CHA2DS2-VASc-HSLp(a) score was found to be the better scoring scheme to predict CAD. If authors optimise cut-off limit for Lp(a) from ≥25 mg/dL to ≥19 mg/dL it will increase sensitivity from 80.7% to 88.7% without affecting the specificity [Table/Fig-7].
Sensitivity and Specificity of risk scores for severe CAD.
| AUC (95% CI) | p-value | Cut of point | Sensitivity (%) | Specificity (%) |
|---|
| FRS | .738(.665-.811) | <0.001 | 7.00 | 61.9 | 64.5 |
| Total CHA2DS2 VASc Score | .851(.809-.893) | <0.001 | 2.0 | 66.6 | 100 |
| Total CHA2DS2 VASc-HSLp(a) score (with Lp(a) cut off ≥25 mg/dL) | .877(.822-.932) | <0.001 | 2.0 | 80.0 | 67.7 |
| Total CHA2DS2 VASc-HSLp(a) score (with optimum Lp(a) cut off ≥19 mg/dL) | .896(.845-.948) | <0.001 | 2.0 | 88.7 | 67.7 |
Comparison of ROC curves according to coronary stenosis of 50% in at least 1 vessel with Lp(a) cut-off value of ≥25 mg/dL in CHA2DS2-VASc-HSLp(a) score.
Comparison of ROC curves according to coronary stenosis of 50% in at least 1 vessel with optimum Lp(a) cut-off value of ≥19 mg/dL in CHA2DS2-VASc-HSLp(a) score.
Discussion
In this study, in the group of patients with the total CHA2DS2-VASc score <2, 16.1% patients had normal coronary vessels, 30% had single vessels involved, 16.1% had two vessels involved and 37.8% had involvement of three vessels. In contrast, when the total CHA2DS2-VASc is ≥2, none of the patients had normal coronaries, 31.45% had single vessel involved, 15.51% had two vessels involved and 67.14% had triple-vessel disease. The results have a p-value of <0.001 and are significant. Cha MJ et al., conducted a study “The association between asymptomatic CAD and CHADS2 and CHA2DS2-VASc scores in patients with stroke” [19]. In their multivariate analysis, after adjusting for confounding factors, CHADS2 and CHA2DS2-VASc scores ≥2 were independently associated with CAD. The CHA2DS2-VASc score was a better predictor of the presence of CAD than the CHADS2 score on area under the curve analysis. CHADS2 and CHA2DS2-VASc scores were predictive of the presence and severity of CAD in patients with stroke. When a patient has high CHADS2 or CHA2DS2-VASc scores, physicians should consider coronary artery evaluation [19].
The newly defined score CHA2DS2-VASc-HSLp(a) of present study was found to be better predictor of severity of CAD. According to present study, when the total CHA2DS2-VASc-HSLp(a) score<2, 17.7% patients had normal coronaries, 39.9% of patients had single-vessel disease, 21.2% had double-vessel disease and 21.2% had triple-vessel disease, whereas when the respective score was ≥2, the percentage of patients with normal coronary vessels was only 2.5%, single-vessel disease was present in 25.2%, double-vessel disease in 12.5% and triple-vessel disease in 59.8%; this difference was highly significant (p<0.001). As risk factors for the development of CAD, and thromboembolism are almost similar, CHADS2 and CHA2DS2-VASc scores may provide valuable information regarding both of these.
Cetin M et al., conducted a study similar to present study which also gave results consistent with present study and suggested that the CHADS2, CHA2DS2-VASc, and especially CHA2DS2-VASc-HS scores could be considered predictive of the risk of severe CAD [20]. As authors added an important risk factor for Indians i.e., lipoprotein(a) and made a modified CHA2DS2-VASc-HSLp(a) Score which was found to be useful for prediction of severe CAD in Indians.
In this study, correlation of the different coronary risk assessment scores including Framingham risk score, CHA2DS2-VASc score and CHA2DS2-VASc-HSLp(a) scores, were assessed for number of affected vessels and Gensini score. The FRS, CHA2DS2-VASc, and Total CHA2DS2-VASc-HSLp(a) Score correlated significantly with the number of significant diseased vessels (r=0.157, p<0.001; r=0.279, p<0.001; and r=0.461, p<0.001, respectively). In addition, the FRS and CHA2DS2-VASc scores correlated significantly with the Gensini score (r=0.194, p<0.001 and r=0.459, p<0.001, respectively). The correlation between the CHA2DS2-VASc-HSLp(a) Score and Gensini scores was greater than that between the FRS and CHA2DS2-VASc scores (r=0.587, p<0.001). These findings of present study are similar to that of Cetin M et al., study which showed that the CHADS2, CHA2DS2-VASc, and CHA2DS2-VASc-HS scores correlated significantly with the number of significant diseased vessels (r=0.406, p<0.001; r=0.308, p<0.001; and r=0.533, p<0.001, respectively) [20]. In addition, the CHADS2 and CHA2DS2-VASc scores correlated significantly with the Gensini score (r=0.383, p<0.001 and r=0.300, p<0.001, respectively). The correlation between the CHA2DS2-VASc-HS and Gensini scores was greater than that between the CHADS2 and CHA2DS2-VASc scores (r=0.500, p<0.001) [20].
In present study, the mean CHA2DS2-VASc score in patients with normal coronaries, SVD, DVD, and TVD group were 0.55±0.506, 1.77±1.054, 2.05±1.584 and 2.19±1.048 respectively. This difference between the groups was statistically not significant (p-value >0.05). Therefore, this score is not useful in predicting CAD in Indian population of present study. Similar results were found in study by Cetin M et al., in which mean CHA2DS2-VASc score in normal coronaries group of patients was 1, patients with single-vessel disease had a mean score of 1.5, also the patients with double and triple-vessel disease had a mean score of 2 [20].
In present study, the mean CHA2DS2-VASc-HSLp(a) score in patients with normal coronaries, SVD, DVD, and TVD groups were 1.00±1.095, 2.49±1.246, 3.08±1.609 and 3.66±1.386 respectively. This difference between the groups was highly statistically significant (p<0.001). This score has a better correlation than CHA2DS2-VASc score with the severity of CAD because of addition of important risk factors of CAD in Indian population i.e., hyperlipidemia, smoking and lipoprotein(a). Therefore this score can be used in predicting CAD and its severity in Indian population. Present study was similar to the study by Cetin M et al., in which they found mean CHA2DS2-VASc-HS score two in patients with normal coronaries or SVD, three in DVD and four in TVD [20].
After analysing the entire present study population based on FRS, CHA2DS2-VASc, and CHA2DS2-VASc-HSLp(a) scores, patients with FRS ≥10, CHA2DS2-VASc scores of ≥2 and CHA2DS2-VASc-HSLp(a) score of ≥2 had significantly higher Gensini scores with p-value <0.001.
In present study, for prediction of CAD, the cut-off value of FRS was 7.00 with a sensitivity of 61.9% and specificity of 64.5% (AUC 0.738, 95% confidence interval 0.665 to 0.811, p<0.001) and the cut-off value of CHA2DS2-VASc score was >2 with a sensitivity of 66.6% and specificity of 100% (AUC 0.851, 95% confidence interval 0.809 to 0.893, p<0.001) whereas the cut-off value of CHA2DS2-VASc-HSLp(a) score was >2 with a sensitivity of 80% and specificity of 67.7% (AUC 0.802, 95% confidence interval 0.822 to 0.932, p<0.001). So, by adding hyperlipidemia, smoking, and lipoprotein (a) the sensitivity increased but specificity decreased which makes it a more useful screening tool for prediction of CAD severity.
According to these results, the CHA2DS2-VASc-HSLp(a) score was found to be the better scoring scheme to predict CAD. The newly defined score {CHA2DS2-VASc-HSLp(a)} included additional important risk factor for CAD in Indians i.e., Lp(a) to CHA2DS2-VASc-HS score and had a better correlation with the severity of CAD.
Strength
Because of higher sensitivity compared to other scores, this score can be used as a screening tool prior to angiography.
Limitation
The appropriate selection of real cases for coronary angiography resulted in less number of normal coronary cases which was responsible for lower specificity. Further larger group study needed for appropriately estimating specificity.
Conclusion
FRS, CHA2DS2-VASc, and especially CHA2DS2-VASc-HSLp(a) scores could be considered predictive of the risk of severe CAD. The CHA2DS2-VASc-HSLp(a) score was found to be the better scoring scheme to predict CAD severity in Indian population. According to these results, the newly defined CHA2DS2-VASc-HSLp(a) score should be considered to predict CAD severity. Also large scale population based cohort studies should be undertaken.
SVD: Single vessel disease; DVD: Double vessel disease; TVD: Triple vessel disease; SBP: Systolic blood pressure; DBP: Diastolic blood pressure
*Data are expressed as mean±SD and median (minimum to maximum).
SVD: Single vessel disease; DVD: Double vessel disease; TVD: Triple vessel disease
*Data are expressed as mean±SD and median (minimum to maximum).