Highways are important for the development of a country. As highways are expanding and getting improved, many toll plazas are being installed to collect the taxes, while doing so, the health hazards of the toll collectors due to the air pollution are not being looked into.
Exposure to the air pollutants due to vehicular exhausts causes cough, sputum production and decreased lung function [3]. In India, all 462 toll plazas (as on August 2018) are manually operated and each toll plaza has around 150 to 200 personnel working in 3 shifts, 8 hours/day [4]. Only a couple of pulmonary function studies have been done on toll personnel, whereas more number of studies have been reported on traffic policemen [2,5,6].
The present study was aimed to carry out dynamic PFT on the toll personnel of the Sriperumbudur toll plaza, Tamil Nadu, India, using a computerised spirometer and identify any ventilatory defects.
Materials and Methods
Study Subjects
This observational study was conducted at Sriperumbudur toll plaza, Tamil Nadu, India, during May 2017 which is the summer season in Tamil Nadu. The test subjects included toll collectors, supervisors and security personnel who were continuously exposed to the vehicular traffic. The study was conducted on 44 subjects (Male n=35, Female n=9). Human ethical committee clearance was obtained prior to the study from the institution 15/mmchri/2017(A).
Inclusion and Exclusion Criteria
We included toll personnel working at the toll plaza for more than one month, aged 18 to 60 years (Mean and SD 26±7.7) and ready to give a written informed consent.
We excluded the following toll personnel; who were smokers, or had any history of childhood asthma, history of allergies before joining the toll plaza, any cardiac co-morbid conditions, chest wall and spine deformities, history of surgeries of the thorax, ongoing respiratory tract infections and not willing to give informed consent.
Methodology
Written informed consent was obtained after explaining the objectives of the study in the native language of the subject. Subjects were questioned about pre-employment check-ups and regular health check-ups. They were also questioned whether protective gear, like facemasks were provided or not. Height in centimetres (nearest to 0.1 cm) and weight in kilograms (nearest to 0.1 kg) were measured. Weight was measured using an Omron digital weigh scale (model HN-286) with minimal clothing and without footwear. History and vital parameters (pulse rate, respiratory rate, SpO2, blood pressure) were recorded. Pulse rate was recorded manually for a minute, and while still palpating the pulse, the respiratory rate was counted visually for a minute to prevent the subject from being aware of his/her breathing. SpO2 was measured with Easycare pulse oximeter (model ECPO-250E) and blood pressure was measured using Omron automatic blood pressure monitor (model HEM-7111). All vital signs were recorded in a relaxed and seated position. General and clinical examination was done to exclude any respiratory and cardiac conditions. Eligible subjects were taken up for PFT, and the tests were conducted using RMS Helios 401 (Recorders & Medicare Systems Pvt., Ltd.,) in makeshift cabins at the Toll Plaza itself. The PFT were conducted with hygiene precautions around 0800 hours to 1100 hours. Prior to the PFT, the subjects were briefed about the procedure and a demonstration was done by the technician. The subjects were instructed to take a full inspiration (to total lung capacity), exhale forcefully and completely into the mouthpiece, and then inspire forcefully and fully back to total lung capacity (to complete the flow volume loop). The subjects were given trials and minimum three test attempts but not more than eight. Acceptable manoeuvres were taken for interpretation. Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 second (FEV1), Ratio of FEV1/FVC (FEV1/FVC), Forced expiratory flow 25-75% (FEF25-75%), Peak Expiratory Flow Rate (PEFR) were recorded. The reports were interpreted in the Department of Tuberculosis and Chest medicine, of the institution.
Statistical Analysis
The Spirometry test parameters were compared with the predicted values (generated in the RMS Helios 401 software version-3.1.39 using Indian Predicted equations) by paired t-test with the help of Quickcalcs by GraphPad Software. Statistical significance was indicated by p-value <0.05. Correlation analysis (Pearson’s) was done to find any relationship between the duration of exposure with spirometry parameters and respiratory rate.
Results
The data of vital parameters is depicted in [Table/Fig-1]. PFT were recorded from the toll collectors (n=34), supervisors (n=5) and security personnel (n=5) and interpreted by the chest physician for any ventilator defects.
Vital parameters of the participants.
| Parameters | Height (cm) | Weight (Kg) | Pulse rate(/min) | Systolic Blood Pressure (mmHg) | Diastolic Blood Pressure (mmHg) | SpO2 (%) |
|---|
| Mean±SD | 162.8±9.4 | 60.6±12.7 | 80.6±12.2 | 127.1±13.9 | 78.5±11 | 98.14±1.3 |
Observed FVC (2.73±0.614) and PEFR (6.88±1.59) in the Toll plaza personnel was statistically less than the expected values FVC (3.2±0.6225) and PEFR (8.14±1.543) respectively (p<0.0001). The FEV1/FVC (96.93±4.48) in the Toll personnel statistically increased than the expected value FEV1/FVC (85.11±2.65) (p<0.001) [Table/Fig-2].
Comparison of PFT parameters between predicted and observed.
| Parameter | Case (Mean±SD) (n=44) | p-value |
|---|
| A=Predicted | B=Test |
|---|
| FVC (L) | 3.2±0.623 | 2.73±0.614 | <0.0001* |
| FEV1 (L) | 2.73±0.566 | 2.65±0.594 | 0.1819 |
| FEV1/FVC % | 85.11±2.65 | 96.93±4.480 | <0.0001* |
| FEF25-75(L/s) | 4.11±0.771 | 4.16±1.146 | 0.7436 |
| PEFR (L/s) | 8.14±1.543 | 6.88±1.588 | <0.0001* |
*Statistically significant by paired student t-test, FVC (L)=Forced vital capacity (litres), FEV1 (L)=Forced expiratory volume in one second (litres), FEF25-75 (L/s)=Forced expiratory flow 25-75 (litres/second), PEFR (L/s)=Peak expiratory flow rate (litres/second), SD=Standard deviation
Pearson’s Correlation analysis of working years (15 subjects were working for 1 to 6 months, 7 subjects working 6 months to a year and 22 subjects working more than a year) with spirometry parameters FVC and FEV1 showed that there was a negative correlation of -0.172 and -0.034 respectively, which was not statistically significant. Correlation analysis between the working years with PEFR and FEF25-75% showed a positive correlation of 0.025 and 0.156, whereas only FEV1/FVC showed a significantly positive correlation [Table/Fig-3].
Correlation between working years and spirometry parameters.
| FVC | FEV1 | PEFR | FEV1/FVC | FEF25-75% |
|---|
| R value | -0.172 | -0.034 | 0.025 | 0.362 | 0.156 |
| p-value | 0.264 | 0.825 | 0.873 | 0.016* | 0.311 |
*Correlation is significant at the 0.05 level (2-tailed)
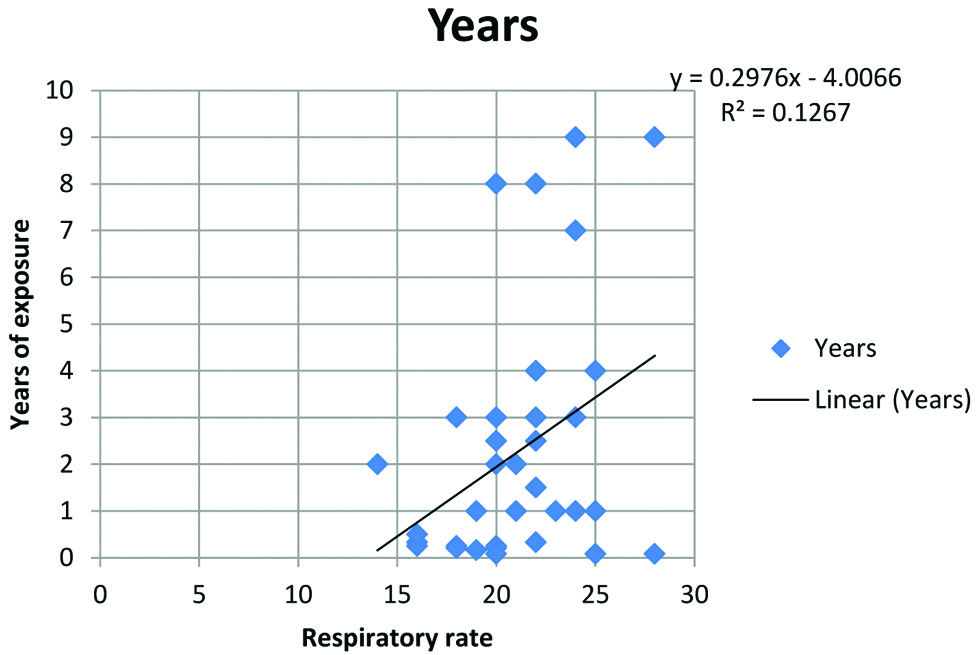
Pearson’s Correlation analysis of respiratory rate with years of working in toll plaza showed that there was a positive correlation of 0.356 (R value) which was significant (p=0.0177). Hence, we may infer that there is a significant increase in the respiratory rate as the period of exposure increases. Persons working at the toll Plaza had a mean respiratory rate of 21±3 (Range 14 to 28) [Table/Fig-4].
Correlation between respiratory rate and years of exposure*.
*Statistically significant at p<0.05, R value=0.356
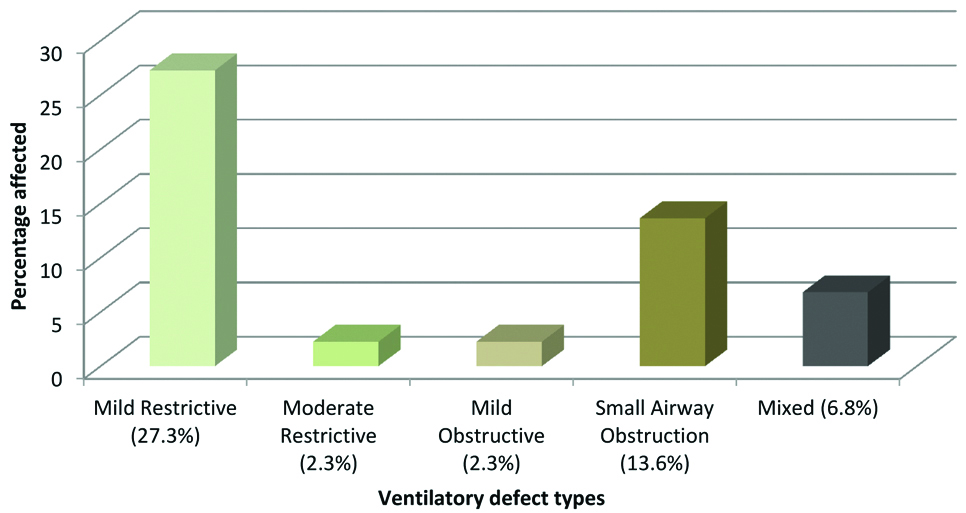
Interpretation of the PFT revealed that 47.73% of the test subjects had normal pulmonary function tests, while 52.27% had ventilatory defects. Observed type of ventilator defects were predominantly mild restrictive pattern (27.3%) (n=12) followed by small airway obstruction (13.6%) (n=6) [Table/Fig-5].
Graph showing the percentage of various ventilatory defects observed.
Discussion
In this study a total of 44 toll plaza personnel were included. Mean duration of working in the toll plaza was 2.24 years. None of the test subjects wore protective masks during work. Certain PFT parameters were less than the predicted values.
The decreased pulmonary function parameters may be due to numerous pollutants from the vehicular exhausts like Carbon monoxide, sulphur dioxide, particulate matter. These substances cause oxidative stress on the lungs leading to chronic bronchitis, emphysema, fibrotic lung diseases and cancer [5]. Toxic gases and chemicals from the vehicular exhaust cause allergy and irritation in the airways and lungs of the persons exposed to them for a long time, similar to the subjects of the present study, the toll plaza personnel [6]. Air quality monitoring carried out at highway toll plazas, municipality toll plazas and control sites in the National Capital Region of Delhi, revealed high level of air pollution at almost all locations with particulate matter 2.5 (PM2.5) values exceeding the national permissible limit except at a few control sites [7]. Reactive oxygen species of bronchial epithelial cells and macrophages due to organic extracts of diesel emissions are targeted by the particulate matter in the lung. These reactive oxygen species activate stimulators of chemokines and cytokines by certain proteins like activator protein-1 and nuclear factor-kappa B signalling pathways leading to allergic inflammation. Apoptosis and necrosis via mitochondrial pathway in the bronchial epithelial cells is triggered by the organic diesel exhaust substances [8,9]. Inhalation of chemical components like poly-aromatic hydrocarbons, which are major components of diesel exhaust cause increased production of Immunoglobulin E and also leads to lung and airway inflammation [10-12]. These might be the reasons for the decreased observed values of FVC and FEV1 compared to the predicted values suggesting a restrictive ventilatory defect in the toll plaza personnel. The diagnosis of restriction is based upon the finding of a normal FEV1/VC and reduced VC in the setting of a decreased TLC [13].
Regarding small airway obstruction, abnormal values for FEF25-75%, in conjunction with normal values for FVC and FEV1, are often useful in identifying small-airway disease [13]. Diesel exhaust particles are very small, with diameters ranging from 0.02 nm to 0.2 nm and larger surface area to mass ratio, carry a large fraction of toxic substances like hydrocarbons and metals on their surface. Chronic exposure to them can lead to chronic inflammation of the small airways and lung parenchyma [14,15].
FEV1/FVC indicates the condition of the bronchial musculature [16]. In our study FEV1/FVC was increased in the toll plaza personnel and was statistically significant when compared with the predicted values (refer [Table/Fig-1]). This finding was similar to a previous study conducted on Traffic Policemen (Test FEV1/FVC %=88.33±9.83, Predicted FEV1/FVC %=80.27±2.10) [16]. To differentiate obstructive pattern from restrictive pattern, FVC, FEV1 and FEV1/FVC was used. In obstructive lung diseases FEV1 is reduced disproportionately more than FVC, so FEV1/FVC ratio is reduced. In restrictive lung diseases, FEV1 is disproportionately less reduced than FVC, so FEV1/FVC ratio is increased [17].
The normal rate of respiration in a relaxed adult is about 14-16 breaths per minute [18]. In this study the subjects had a mean respiratory rate of 21 breaths per minute. Persons with restrictive ventilator disorders adopt a breathing pattern that is characterised by small tidal volumes and a rapid respiratory rate, often with little apparent effort. This pattern is seen in patients with a decrease in the distensibility of the lung or chest wall or with reduction of the vital capacity from any other cause [19]. This might be the reason for the increased respiratory rate in the present study subjects.
Correlation analysis of FVC, FEV1 with years of working in toll plaza showed that there was a negative correlation of -0.172 and -0.034 respectively, which was not statistically significant. Another study also showed negative correlation but were statistically significant [16]. This might be due to a small number of test subjects in the present study.
Limitation
The sample size was less in this study. Obtaining permission for the study from the toll administration people was difficult, and hence the low number. The effect of other confounding factors like smoking, asthma etc., was not assessed in the present study which can be done later.
This study can be done with controls in the future and can be expanded to the other toll plazas, if permission is granted by the toll administration. The study is planned to be followed up after a year on the same subjects to see any deterioration in their lung function.
Conclusion
From the above study, it might be inferred that the vehicular emissions cause decreased lung function in the toll personnel. During the study, the subjects revealed that there was no pre-employment medical examination done and the subjects did not use masks even when provided. The toll collectors were seated in cabins that were not properly ventilated. So it may be suggested that pre-employment and periodic medical examination with computerised PFT will help identifying at risk persons and preventive care can be started at the early stage of the disease. Face masks, reduced duty timings, air monitoring and proper ventilated cabins with positive pressure will help in decreasing the exposure to the air pollutants.
*Statistically significant by paired student t-test, FVC (L)=Forced vital capacity (litres), FEV1 (L)=Forced expiratory volume in one second (litres), FEF25-75 (L/s)=Forced expiratory flow 25-75 (litres/second), PEFR (L/s)=Peak expiratory flow rate (litres/second), SD=Standard deviation
*Correlation is significant at the 0.05 level (2-tailed)