Conservative Management of Intraperitoneal Urinary Bladder Perforation with Enterovesical Fistula
Debansu Sarkar1, Akash Agrawal2, Dilip Kumar Pal3
1 Associate Professor, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
2 Post Doctoral Trainee, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
3 Professor and Head, Department of Urology, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dilip Kumar Pal, 244, AJC Bose Road, Kolkata-700020, West Bengal, India.
E-mail: urologyipgmer@gmail.com
Surgical repair is usually done in intraperitoneal bladder perforation, whereas in genitourinary trauma reports of conservative management exist. We hereby, present a case of an old man with carcinoma prostate having intraperitoneal urinary bladder perforation with enterovesical fistula that was successfully managed non-operatively and conservatively.
Bladder trauma, Intraperitoneal perforation, Non surgical treatment
Case Report
An 81-year-old gentleman was diagnosed to have Adenocarcinoma of Prostate (Gleason 4+5) after Trans Urethral Resection of Prostate (TURP) six years back. He did not receive any androgen deprivation therapy following TURP. Voiding symptoms recurred after a few months and a bladder neck incision and bilateral orchidectomy was done three months after first TURP. Patient was asymptomatic with controlled Prostate Specific Antigen (PSA) in March of 2018, when he developed painless gross haematuria. He underwent a cystoscopy in some other health care centre. It revealed a grade III prostatomegaly, the bladder having substantial clots and a large perforation was noted at the dome of the bladder. During the procedure; there was acute abdominal distention, pain, and severe respiratory distress. The procedure was abandoned and an intraperitoneal drain was placed. The tube instantly drained about 1 litre of serosanguinous fluid, which decreased to 10 to 20 mL/day over a period of 3-4 days.
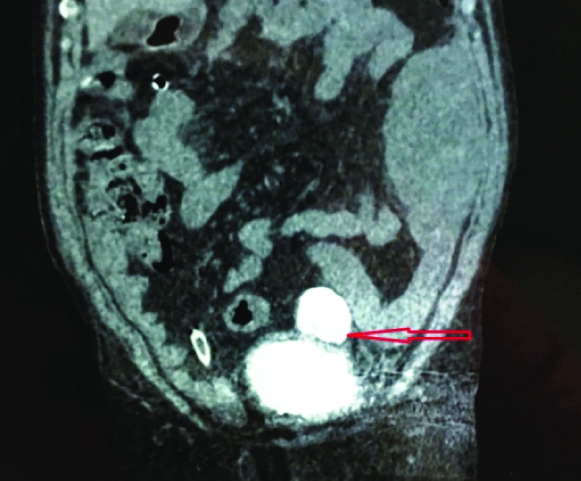
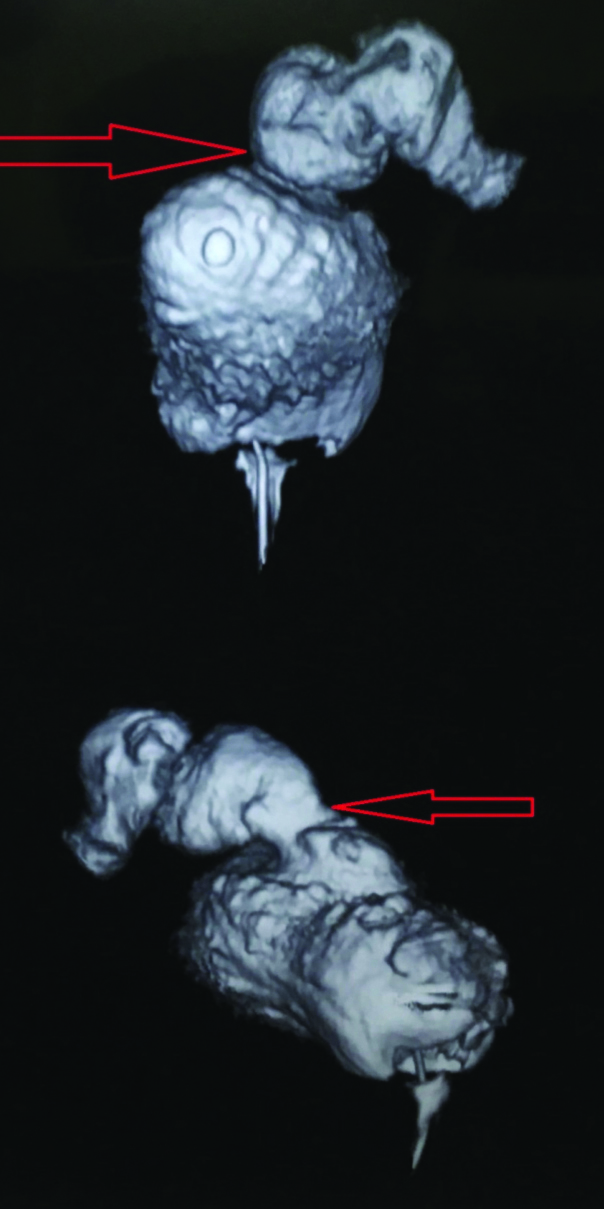
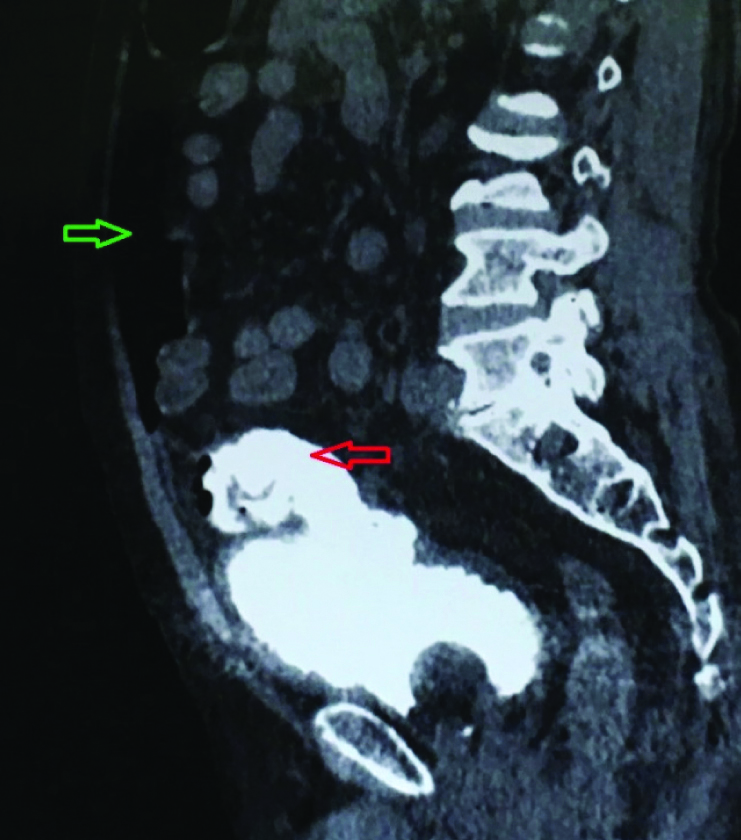
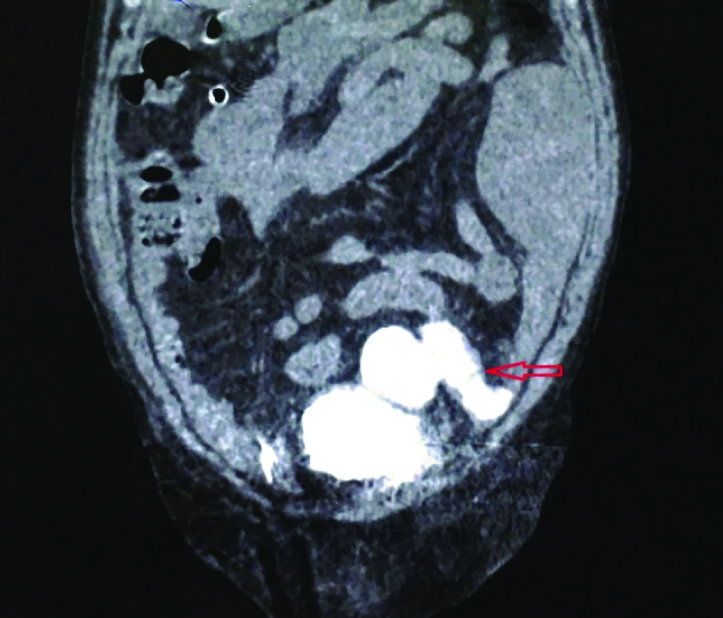
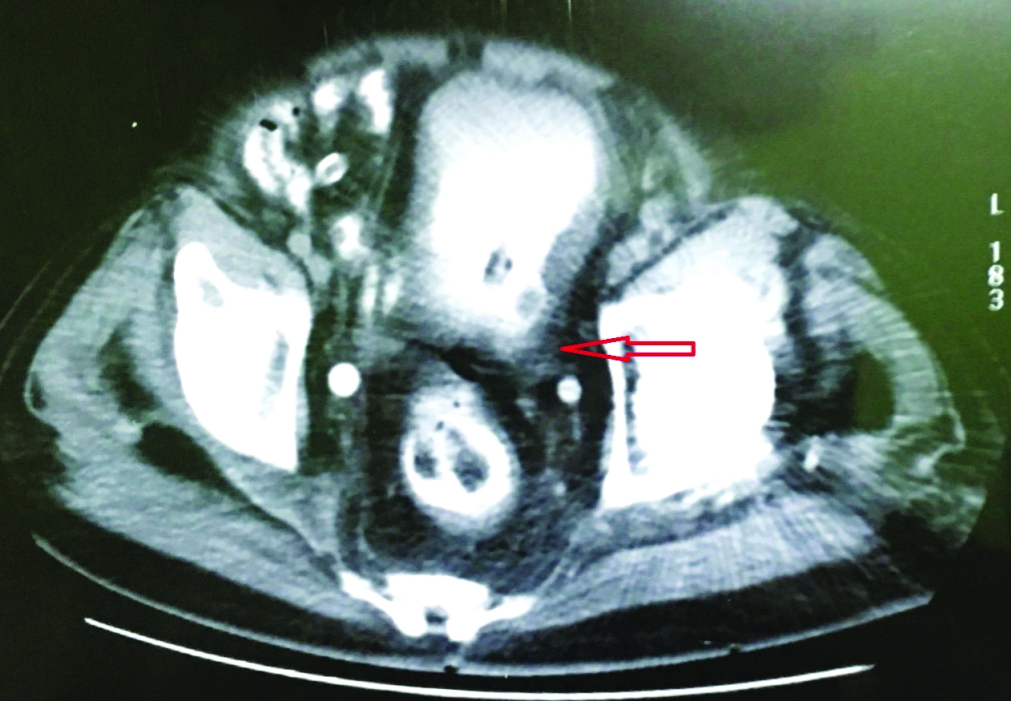
Patient was referred to us, on his second postoperative day. On examination, abdomen was soft, non distended and non tender, vitals were stable. Drain fluid creatinine was measured and found to be 56 mg/dL. Simultaneous serum creatinine was 1.5 mg/dL. Contrast “enhanced” CT scan was done which revealed intraperitoneal bladder perforation, pneumoperitoneum and a cysto-enteric fistula with contrast going into the small intestine [Table/Fig-1,2,3 and 4]. Though, it was an intraperitoneal bladder rupture with a cysto-enteric fistula a conservative management was planned, as there were no abdominal signs with stable vitals. In further course, patient developed a left lumbar lump containing purulent material, which was drained subsequently.
CT showing intraperitoneal bladder perforation.
3D CT showing enterovesical fistula.
CT showing bladder perforation (red arrow) and urinary ascites (green arrow).
Coronal view showing enterovesical fistula.
Subsequent CECT KUB with delayed film after two weeks did not reveal any bladder perforation or cysto-enteric fistula [Table/Fig-5]. Per urethral catheter was kept for three weeks. After catheter removal, patient passed urine spontaneously and doing well till the last follow-up prior to the publication of this paper.
CT showing resolution of perforation and enterovesical fistula.
Discussion
Trauma is the most common cause of bladder rupture which includes blunt, penetrating, and iatrogenic injuries comprising about 96% of cases. Other causes are spontaneous rupture (<1%) and intoxication (2.9%). Extra-peritoneal rupture occurs in approximately 60 to 65% of cases, and intraperitoneal rupture in 25%. Over 80% of patients with bladder rupture also have pelvic fracture, bowel injury, or intraperitoneal solid organ injury [1].
Extra-peritoneal ruptures result in extravasation of urine in the confines of space of Retzius and are usually managed conservatively by long term catheter drainage with or without placement of extra-peritonel drain [2]. On the contrary, intraperitoneal ruptures are usually managed surgically. These ruptures are often much larger than suggested on cystogram and are unlikely to heal spontaneously. Urinary ascites may result in biochemical/electrolyte abnormalities (hyperkalemia, hypernatraemia, uraemia and acidosis) and fatal peritonitis. But there are patients who may not have any florid clinical signs of peritonitis or patients with very high risk for any surgical intervention may force the surgeon for conservative treatment of intraperitoneal bladder rupture. The concept of conservative treatment of intraperitoneal rupture probably came from these clinical situations [3].
In the 1970s, Mulkey AP et al., Richardson JR et al., and Robards VL et al., published three papers (case reports), respectively, about the non-operative management for intraperitoneal perforation and concluded surgical repair might not be the only choice [4-6]. Pansadoro A et al., reported the successful management of two cases of intraperitoneal perforation following transurethral resection of bladder tumour using intraperitoneal drain and indwelling transurethral Foley catheters [7]. Basiri A et al., conservatively treated for the first time a case of spontaneous intraperitoneal rupture of the urinary bladder due to prostate cancer [8]. Osman Y et al., performed a study involving eight paediatric patients with post-traumatic intraperitoneal bladder rupture, in which the patients were grouped equally for open surgical repair and conservative treatments [9]. All the children receiving conservative treatments demonstrated significant improvement in general condition within a few hours of the bladder and peritoneal drainage and intraperitoneal tube drains were removed at 1 to 4 days. The mean indwelling catheter duration was 11.8 days. Likewise, in the present case drain was kept for four days and catheter duration was 21 days.
In this case, patient presented to us on second postoperative day. He had stable general condition, few clinical signs of peritonitis and was not in acute surgical emergency. Considering his age, co-morbidities, stable general condition, paucity of abdominal signs and minimal drainage of intraperitoneal drain we decided to go for conservative therapy, being mentally ready for intervention if there was any sign of deterioration. Diagnosing a vesico-enteric fistula on CT scan was an additional surprising radiological finding. Still, we could continue with conservative therapy based on the principle of management of controlled enteric fistulas.
We opine that, the most important component in the management of intraperitoneal bladder perforation and vesico-enteric fistula is drainage. This drainage can be percutaneous intraperitoneal drainage and drainage of the bladder with Foleys catheter. However, the indications for surgical repair should be kept in mind; improper bladder drainage, deterioration of general condition, prolonged urinary drainage through the peritoneal drain, lack of clinical or laboratory improvement, and concomitant injuries that need laparotomy.
Present case illustrates that even a conservative approach in the treatment of small intraperitoneal ruptures and vesicoenteric fistulas may be considered if a number of conditions are maintained: urinary antibiotic prophylaxis and continued urinary drainage through an indwelling catheter for a minimum of two weeks until the closure of the perforation and fistula are evident on CT cystogram. Although the intraperitoneal bladder perforation and vesicoenteric fistula treatment procedure has not changed much for more than 30 years, it can be suggested from this case report that; conservative management has its own place in highly selective patients.
Conclusion
Urinary ascites should be considered in the differential diagnosis of ascites in patients who have had bladder surgery or any transurethral procedure in their past surgical history. Serum and ascitic fluid biochemistry in conjunction with CT cystography are key to diagnosis. Though surgery is the primary mode of treatment, a conservative approach is also possible, even in cases with vesicoenteric fistula. Nevertheless, we recommend strict vigilance for development of any periteoneal signs, continued antibiotic prophylaxis and continuous bladder drainage via an indwelling catheter until there is objective evidence of healing.
[1]. Morey AF, Genital and lower urinary tract trauma. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editorsCampbell-Walsh Urology 2011 10th edPhiladelphia, PASaunders:2513 [Google Scholar]
[2]. Kong JPL, Bultitude MF, Royce P, Gruen RL, Cato A, Corcoran NM, Lower urinary tract injuries following blunt trauma: a review of contemporary managementReviews in Urology 2011 13(3):119-30. [Google Scholar]
[3]. Geng J, Chang H, Chung S, Chen P, Chiu B, Tsai C, Nonoperative treatment for intraperitoneal bladder ruptureUrological Science 2014 25(2):70-72.10.1016/j.urols.2013.05.012 [Google Scholar] [CrossRef]
[4]. Mulkey Jr AP, Witherington R, Conservative management of vesical ruptureUrology 1974 4:426-30.10.1016/0090-4295(74)90012-0 [Google Scholar] [CrossRef]
[5]. Richardson Jr JR, Leadbetter Jr GW, Non-operative treatment of the ruptured bladderJ Urol 1975 114:213-16.10.1016/S0022-5347(17)66988-X [Google Scholar] [CrossRef]
[6]. Robards Jr VL, Haglund RV, Lubin EN, Leach JR, Treatment of rupture of the bladderJ Urol 1976 116:178-79.10.1016/S0022-5347(17)58736-4 [Google Scholar] [CrossRef]
[7]. Pansadoro A, Franco G, Laurenti C, Pansadoro V, Conservative treatment of intraperitoneal bladder perforation during transurethral resection of bladder tumorUrology 2002 60:682-84.10.1016/S0090-4295(02)01843-512385934 [Google Scholar] [CrossRef] [PubMed]
[8]. Basiri A, Radfar MH, Conservative management of early bladder rupture after postoperative radiotherapy for prostate cancerUrol J 2008 5:269-71. [Google Scholar]
[9]. Osman Y, El-Tabey N, Mohsen T, El-Sherbiny M, Nonoperative treatment of isolated posttraumatic intraperitoneal bladder rupture in children-is it justified?J Urol 2005 173:955-57.10.1097/01.ju.0000152220.31603.dc15711348 [Google Scholar] [CrossRef] [PubMed]