The Gleason System is one of the most robust predictors of prognosis in prostatic carcinomas [1]. It is a parameter that has timelessly played a prime role in prostatic cancer clinical decision making, as evidenced in the Partin’s tables, Kattan nomogram or CAPRA (Cancer of the prostate risk assessment) [2]. The conventional Gleason system was introduced in 1966 and consists of a five-tiered grading system that was based solely on the architectural pattern of the tumour and combines two elements to give a combined Gleason Score i.e., the sum of the two most prevalent patterns. Over time, this system has undergone revisions in 1977 by Mellinger and subsequently at the ISUP in 2005 [3].
As outlined by Epstein J, the urgent need for a more substantial revision arose primarily for the following reasons [1]: Grading on needle cores or multiple cores from different sites of the prostate was not an issue of relevance in the Gleason era as biopsy techniques consisted of thick gauge needle biopsies in an area with palpable abnormality. Prostatic cancer and treatment has changed in leaps and bounds; Prostate Specific Antigen (PSA) screening, immunohistochemistry have made their foray and newer histopathologic variants of prostatic carcinomas have been described.
The 2005 ISUP Modified Gleason System has made substantial revisions to the original, the most important of which is scoring based on sum of the most predominant and the worst pattern in needle biopsies exhibiting a tertiary pattern as well as doing away with the threshold of 5% for higher grade tumour patterns [2].
Studies undertaken by various researchers have consistently shown that the modified grade on needle biopsies correlates better with modified grade on radical prostatectomy specimens as compared to the Conventional Gleason System. This is a welcome departure from the Conventional Gleason system wherein often there is a poor level of agreement between core biopsy and radical prostatectomy specimens. Secondly, it has been noted that there has been a trend of upgrading of tumours that were graded with the modified system compared to the Conventional Gleason System [1].
The objective of the present study is to compare histopathologic grade of prostatic carcinomas using conventional and 2005 ISUP Modified Gleason System and demonstrate whether there is a change in the grade of prostatic carcinomas, originally classified using the Conventional Gleason system, when the 2005 ISUP Modified Gleason System is employed.
Materials and Methods
This was a retrospective review of data collected from the clinical database of Father Muller Medical College Hospital, Mangalore. The data collected was time bound from January 2014 to May 2016.
This study was performed on core biopsy specimens and transurethral resection of prostate specimens that after being submitted for histopathologic examination in the Department of Pathology have been formalin fixed, embedded in paraffin and stained with haematoxylin and eosin histochemical stains. For Transurethral Resection of Prostate (TURP) specimens, the sampling protocol followed was in accordance with recommendations by the College of American Pathologists. Accordingly, those samples weighing 12g or less were submitted in their entirety. For specimens that weighed more than 12g, the initial 12g were submitted in 6 to 8 cassettes, and thereafter for every additional 5g of remaining tissue 1 cassette was submitted.
The Inclusion Criteria for this study were all core biopsy and TURP specimens with histopathologic diagnosis of Conventional acinar adenocarcinoma. All radical prostatectomy specimens, specimens received from patients with history of previous chemotherapy or instrumentation, as well as all other histopathologic types of prostatic carcinomas were excluded.
Variants of acinar adenocarcinoma already have traditionally assigned patterns such as 4 for mucinous variant, 5 for comedo carcinoma, signet ring cell, while for certain other variants such as lymphoepithelioma like carcinoma, grading cannot be applied. The same rationale also applies to non acinar carcinoma variants of prostatic carcinoma wherein pattern 5 has been assigned for neuroendocrine, sarcomatoid and ductal carcinomas with necrosis [4]. Grading cannot be applied for adenoid cystic/basal cell carcinoma. Hence, these were also excluded from the current study.
A total of 30 cases diagnosed with adenocarcinoma prostate between January 2014 to May 2016 were analysed.
This was an observational analytic study wherein two independent observers assessed all the specimens. The first observer graded the cases according to the Conventional Gleason System and the second observer graded the cases according to the 2005 ISUP Modified Gleason System.
Step 1: The specimens were first analysed using the Conventional Gleason Grading System, based on the five architectural patterns as described below:
“Very well-differentiated, small, closely packed, uniform glands in essentially circumscribed masses;
Similar to pattern 1 but with moderate variation in size and shape of glands and more atypia in the individual cells; cribriform pattern may be present, still essentially circumscribed, but more loosely arranged;
Similar to pattern 2 but marked irregularities in size and shape of glands, with tiny; glands or individual cells invading stroma away from circumscribed masses or solid cords and masses with easily identifiable, glandular differentiation within most of them;
Large clear cells growing in a diffuse pattern resembling hypernephroma; may show gland formation;
Very poorly differentiated tumours; usually solid masses or diffuse growth with little or no differentiation into glands [3]”;
Gleason score was assigned based on the most common and second most common patterns.
Step 2: The specimen slides were then analysed by the second observer using the 2005 ISUP Modified Gleason System. Criteria are listed below:
“Circumscribed nodule of closely packed, but separate, uniform, rounded to oval, medium sized acini (larger glands than pattern 3);
Like pattern 1, fairly circumscribed, but at the edge of the tumour nodule, there may be minimal infiltration; glands are more loosely arranged and not quite as uniform as Gleason pattern 1;
Discrete glandular units: typically, smaller glands than seen in Gleason patterns 1 or 2; infiltrates in and among non-neoplastic prostate acini; marked variation in size and shape; smoothly circumscribed, small, cribriform nodules of tumour;
Fused microacinar glands: ill-defined glands with poorly formed glandular lumina; large, cribriform glands; cribriform glands with an irregular border; hypernephromatoid;
Essentially no glandular differentiation, composed of solid sheets, cords, or single cells; comedocarcinoma with central necrosis surrounded by papillary, cribriform, or solid masses [3]”;
Modified Gleason score was assigned based on the primary pattern and the worst pattern.
Step 3: The scores obtained using the Conventional Gleason and 2005 ISUP Modified Gleason Systems were compared.
Cross tabulation of scores obtained via the Conventional Gleason and 2005 ISUP Modified Gleason System was used to analyse whether there has been a change in the Gleason score of the cases reviewed.
Results
Of the 30 cases reviewed, the primary pattern changed in the 2005 ISUP Modified Gleason System in 57% of the cases and remained constant in 43% of the cases. The distribution of changes in the primary pattern is summarised in the [Table/Fig-1] below.
Percentage of cases exhibiting change in the primary pattern.
| Primary Pattern Conventional Gleason System | Primary Pattern 2005 ISUP Modified Gleason System | Number of Cases (%) |
|---|
| 3 | 4 | 8 (47) |
| 3 | 5 | 7 (41) |
| 4 | 5 | 1 (6) |
Out of the 30 cases reviewed, 13 cases were accorded Gleason score 6 (3+3) in the Conventional Gleason system, all of which were upgraded to scores 7-10 in the 2005 ISUP Modified Gleason System. A majority of the cases in this group (69%) were upgraded to Score 9 {53.8% (5+4) pattern and 15.3% (4+5) pattern}. The findings are summarised in [Table/Fig-2].
Percentage of cases originally categorised as Score 6 in the Conventional Gleason System that changed when regraded using the 2005 ISUP Modified Gleason.
| Conventional Gleason System Score 6 | Modified Gleason Score | Number of Cases (%) | Pattern |
|---|
| All categorised as 3+3 | 7 | 1 (7.7) | 3+4 |
| 8 | 1 (7.7) | 4+4 |
| 9 | 2 (15.3) | 4+5 |
| 7 (53.8) | 5+4 |
| 10 | 2 (15.3) | 5+5 |
Seven cases were accorded Gleason score 7 in the Conventional Gleason system {three of which were (4+3) pattern and four of which were (3+4) pattern}. In the 2005 ISUP Modified Gleason System, a majority of the cases (70%) were upgraded to scores 8-10, while one remained the same and another was downgraded to score 6. The findings are described in [Table/Fig-3] below.
Percentage of cases originally categorised as Score 7 in the Conventional Gleason System, that changed when regraded using the 2005 ISUP Modified Gleason System.
| Conventional Gleason System Score 7 | Modified Gleason Score | Number of Cases (%) | Pattern |
|---|
| 3 cases categorised as 4+34 cases categorised as 3+4 | 7 | 1 (14.2) | 4+3 |
| 8 | 2 (28) | 4+4 |
| 9 | 2 (28) | 4+5 |
| 10 | 1 (14.2) | 5+5 |
Seven cases were accorded Gleason score 8 in the Conventional Gleason system {four were (3+5), one was (4+4) and two were (5+3)}. In the 2005 ISUP Modified Gleason System, yet again, 71% cases were upgraded to scores 9-10, while two remained the same. The findings are outlined in [Table/Fig-4] below.
Percentage of cases originally categorised as Score 8 in the Conventional Gleason System that changed when regraded using the 2005 ISUP Modified Gleason System.
| Conventional Gleason System Score 8 | Modified Gleason Score | Number of Cases (%) | Pattern |
|---|
| 4 cases categorsed as 3+51 case categorised as 4+42 cases categorised as 5+3 | 8 | 1 (14.2)1 (14.2) | 4+43+5 |
| 9 | 2 (28)1 (14.2) | 5+44+5 |
| 10 | 2 (28) | 5+5 |
Two cases were accorded Gleason score 9 and one case was accorded Gleason score 10 in the Conventional Gleason System. The Gleason scores of these two categories remained unchanged in the 2005 ISUP Modified Gleason System.
Overall, there was an upgrade in 76% of prostatic carcinomas. The percentage of high grade carcinomas (i.e., Gleason score 8-10) increased from 32.9% in the Conventional Gleason System to 89.93%, a rise of 57%. We also noted a decrease in the number of cases with Score 6, 7 and 8 by 40%, 17.3% and 6.7% respectively. The number of cases with Score 9 and Score 10 increased by 46.73% and 17% respectively. The details of these are summarised in [Table/Fig-5].
Total percentage of cases with scores 6 through 10 in the Conventional and 2005 ISUP Modified Gleason Systems.
| Score | Number of Cases in Conventional Gleason System (%) | Number of Cases in 2005 ISUP Modified Gleason System (%) |
|---|
| 6 | 13 (43) | 1 (3) |
| 7 | 7 (23.3) | 2 (6) |
| 8 | 7 (23.3) | 5 (16.6) |
| 9 | 2 (6.6) | 16 (53.3) |
| 10 | 1 (3) | 6 (20) |
Discussion
The change in primary pattern seen in 57% of the cases overall, with a majority (47%) being accorded pattern 4 in the Modified Gleason system from pattern 3 in the Conventional was on expected lines. This change can be attributed to the revised definition of pattern 4 that now includes virtually all cribriform patterns unless round, well circumscribed, same size as normal glands or associated with necrosis. Secondly, clusters of glands with poorly formed lumina where tangential sectioning was ruled out, were also accorded pattern 4. The second category of change in the primary pattern (41%) was seen in cases reported as pattern 3 in the Conventional Gleason System, now being graded pattern 5 in the 2005 ISUP Modified Gleason System. This could be attributed to the fact that individual cells are no longer allowed in Gleason 3 [Table/Fig-6,7,8,9 and 10].
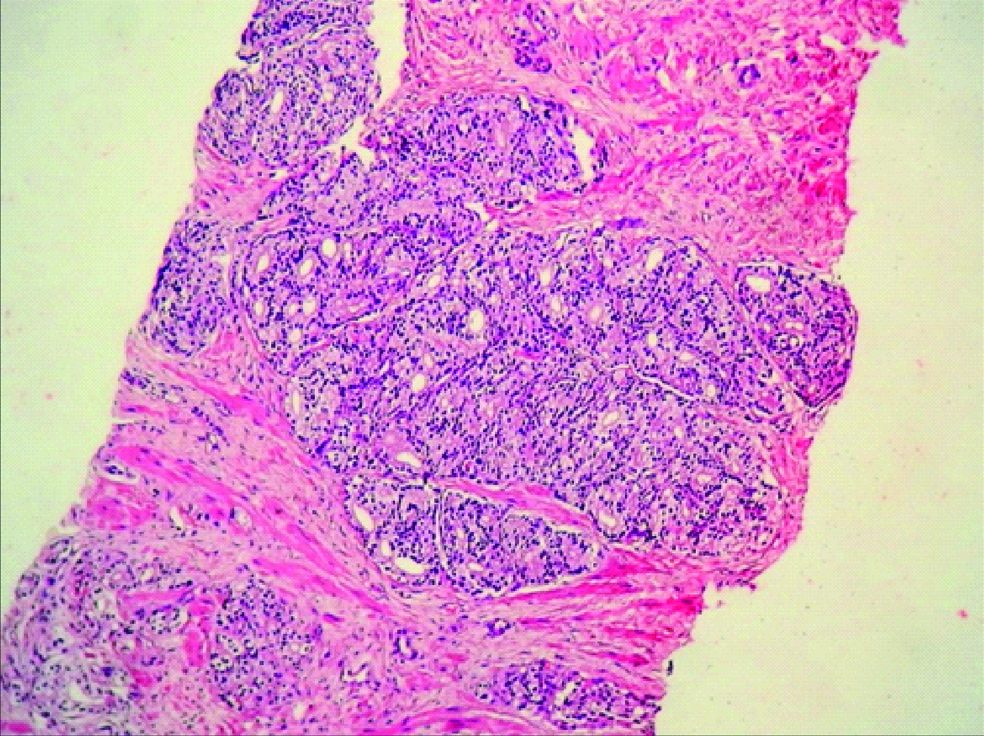
Tumor exhibiting well circumscribed small cribriform nodules, (H&E, 100X).
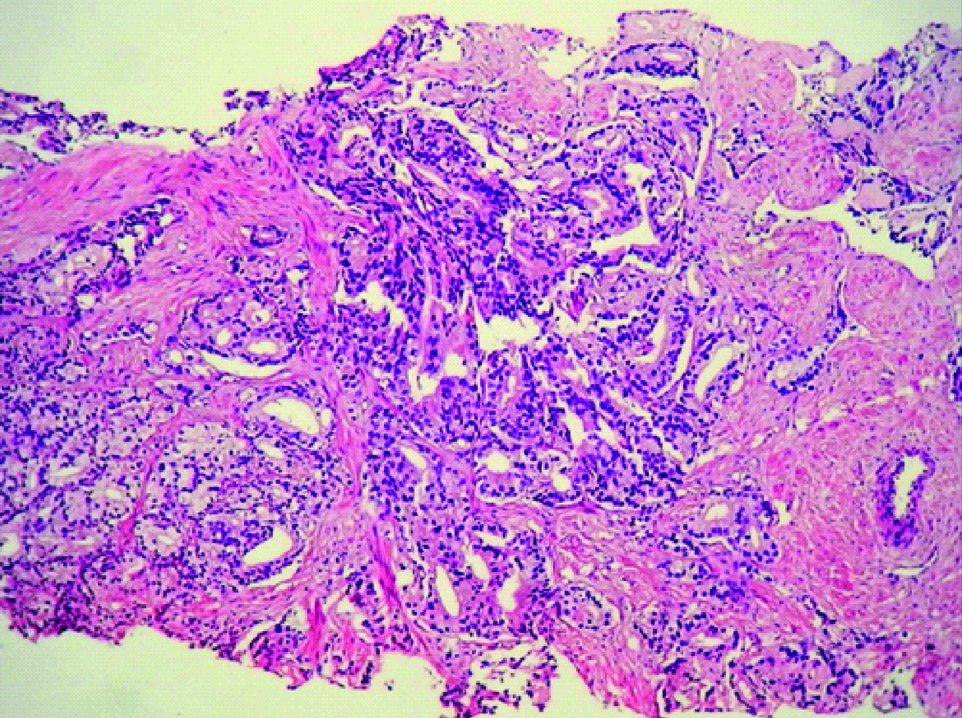
Tumour exhibiting large cribriform glands with an irregular border (H&E,100X).
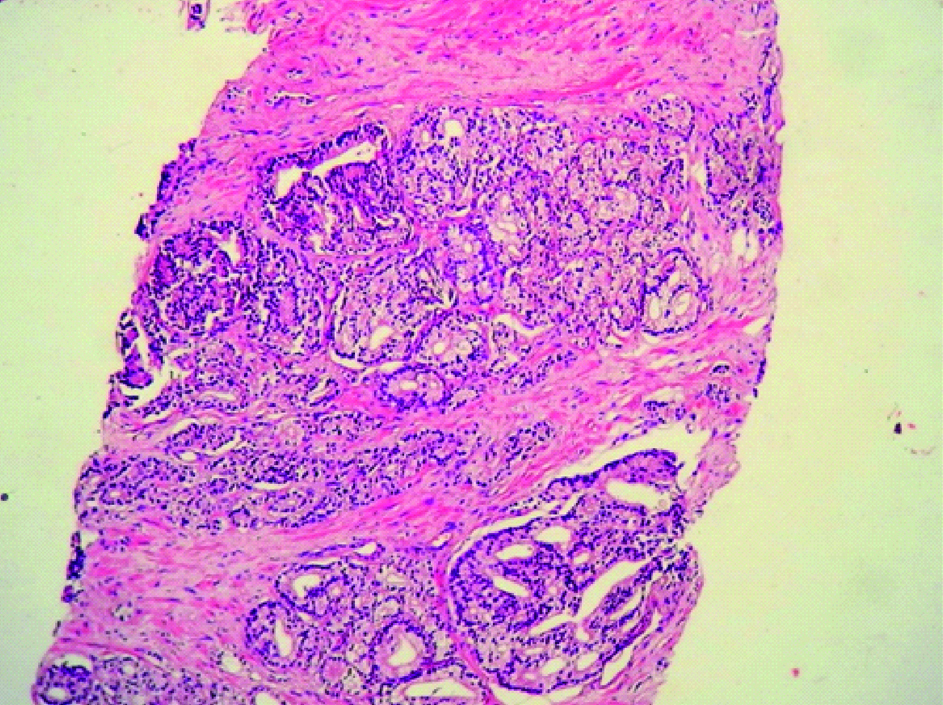
Bottom portion of the image shows tumour with glomeruloid features with transition to cribriform glands (H&E, 100X).
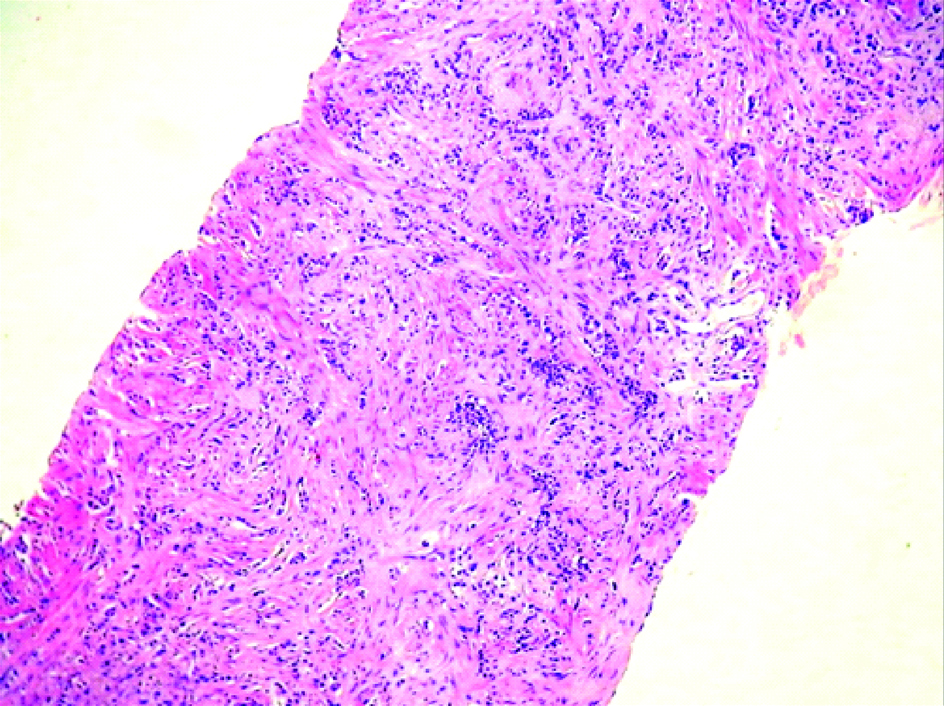
Tumour with ill-defined glands without lumina, arranged as cords and singles (H&E, 100X).
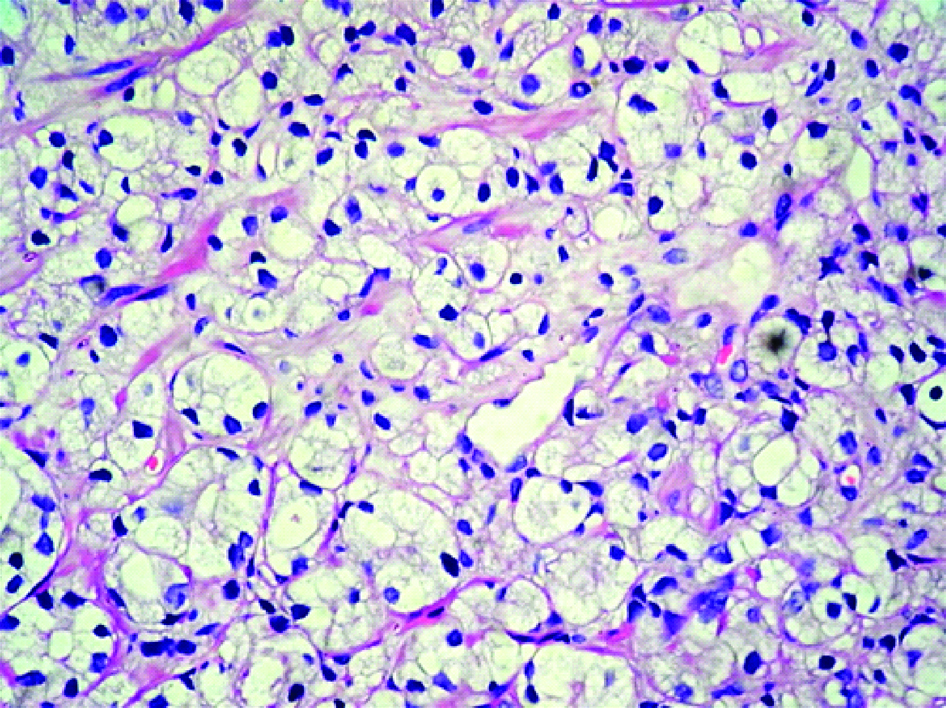
Hypernephromatoid pattern of prostatic adenocarcinoma (H&E, 400X).
The predominant primary pattern in Conventional Gleason System was pattern 3 (70%) with 43% cases exhibiting 3+3 as the commonest patterns occurring in combination.
The predominant primary pattern in 2005 ISUP Modified Gleason System was pattern 5 (46%) followed closely by pattern 4 (40%). The commonest pattern (36.66%) occurring in combination was the (5+4).
The decrease in Gleason score 6 in the 2005 ISUP Modified Gleason System by 40% seen in our study is similar to the results of a study conducted by Al Suhaibani E et al., who in their study on 40 samples found that use of the 2005 ISUP modified Gleason system, resulted in a decrease in score 6 cancers from 25 to 17.5% [5].
The 57% increase in grade of prostatic carcinomas to higher grade tumours (Gleason score 8-10) seen in our study was similar to a study conducted by Dong F et al., who studied 622 patients and demonstrated an upgrading in 34% [6].
A significant departure from the Conventional Gleason System was that tertiary pattern is assigned over the secondary pattern if higher and the absence of a 5% threshold for secondary or tertiary pattern. This finding is very well demonstrated in our study. We found that in the Conventional Gleason System, the 5% threshold rule resulted in exclusion of a tumour of higher grade type in seven cases (23%). The biggest increase occurred in Score 9 which while accounting for 16 cases, exhibited (5+4) pattern in nine cases and (4+5) pattern in five cases. The biggest decrease occurred in Score 6 which, in the Conventional Gleason System exhibited predominantly 3+3 pattern but in the 2005 ISUP Modified Gleason System was shown to demonstrate higher grade patterns, 5+4 being the most common type.
Ten cases demonstrated a single primary pattern in the Conventional Gleason System of which eight cases were of Pattern 3 type. In the 2005 ISUP Modified Gleason System, only four cases exhibited Pattern 3 as the sole primary pattern. Thus a 50% decrease was seen in the reporting of cases with Pattern 3 as the sole pattern type. Pattern 4 was seen as the sole primary pattern in four cases in the Conventional Gleason System while 12 cases exhibited the same in the 2005 ISUP Modified Gleason System, thus exhibiting a 27% increase in total number of tumours exhibiting pattern 4 as the primary pattern. This finding could be attributed to the limitation of definition of Pattern 3 and a more expanded and revised definition of what constitutes Pattern 4 in the 2005 ISUP Modified Gleason System.
As outlined by Egevad L et al., Pattern 4 includes neoplastic glands that exhibit an irregular contour, large glands, irregular distribution of lumina, slit like lumina, large glands, number of glands and small lumina [3]. The revised definition of Pattern 3 cribriform glands is limited to glands with regular contour, small glands, regular distribution of lumens and uniform round lumens.
The ISUP came up with new grading guidelines in 2014 which was accepted for inclusion by the WHO in the 2016 edition of Pathology and Genetics: Tumours of the Urinary System and Male Genital Organs. It is therefore worthwhile to briefly comment on how the 2014 guidelines differ from the Modified 2005 Gleason System. Few of their major conclusions were as follows:
i) “Cribriform glands should be assigned a Gleason pattern 4, regardless of morphology. [7]”. {This differed from the Modified 2005 Gleason System wherein smoothly circumscribed, small, cribriform nodules of tumour were assigned to grade 3 and large, cribriform glands; cribriform glands with an irregular border were assigned to grade 4}.
ii) “Elimination of the term hypernephromatoid cancer [7]”. {In the Modified 2005 Gleason System, this term was included in pattern 4}.
iii) “Assignment of tumours exhibiting glomeruloid glands to Pattern 4 irrespective of their morphology [7]”.
In the 2005 Modified Gleason system, this morphology was a sticking point, with no consensus reached on how to grade glomeruloid glands. While there was a general agreement on assigning larger glomeruloid structures to Gleason pattern 4, for the rare cases with a score of 3+3=6, but containing a few small glomeruloid glands, the score remained 3+3=6 according to one school of thought. Another school of thought wanted all glomeruloid structures labelled as pattern 4 [8]. A further direction of research will be to assess the impact of change in grading from the Modified 2005 Gleason System to the 2014 WHO/ISUP modified Gleason scores.
The change in grading from the Conventional Gleason system to the 2005 ISUP Modified Gleason system has also demonstrated clinical implications. In a study of 38 cases labelled as Gleason score 6 in the conventional Gleason system but showed biochemical progression, Miyamoto H et al., reviewed these cases using the 2005 guidelines and found that many of these were under graded [9]. They concluded that in cases of prostatic carcinoma that were truly Gleason score 6 as per the 2005 Modified Gleason System and lacked any element of pattern 4, patients could be told that their risk of progression is very rare. Ross H et al., in their review found that patients with Gleason score 6 using the Modified Gleason system did not metastasise to pelvic lymph nodes, thereby implying better prognosis [10].
Limitation
The main limitation of the present study is the small sample size.
Conclusion
In this study, the employment of the 2005 ISUP Modified Gleason System resulted in an upgrading of prostatic carcinoma. We may safely conclude that the 2005 ISUP Modified Gleason System serves as an effective tool that provides more accurate prognostic information while planning treatment, given its widespread use and proven reliability. Keeping abreast with and attempting to accurately undertake histopathologic grading of prostatic carcinomas as the Gleason system continues to evolve, is a challenge for every pathologist. It must nevertheless be accepted willingly as we strive to arm our clinical counterparts with the most reliable tool for clinical decision making and treatment planning.