Ayurvedic Treatment Protocol for Chronic Pelvic Pain in Endometriosis
Anjaly Muraleedharan1, Parvathy Unnikrishnan2, Priyadarshana Narayan3, Hemavathi Shivapura Krishnaraja Bhatt4
1 Assistant Professor, Department of Prasutitantra and Striroga, Amrita School of Ayurveda, Amrita Vishwa Vidyapeetham, Amritapuri, Kerala, India.
2 Assistant Professor, Department of Prasutitantra and Striroga, Amrita School of Ayurveda, Amrita Vishwa Vidyapeetham, Amritapuri, Kerala, India.
3 Assistant Professor, Department of Prasutitantra and Striroga, Maria Ayurveda Medical College and Hospital, Kanyakumari, Tamil Nadu, India.
4 Professor and Head, Department of Prasutitantra and Striroga, Amrita School of Ayurveda, Amrita Vishwa Vidyapeetham, Amritapuri, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemavathi Shivapura Krishnaraja Bhatt, Professor and Head, Department of Prastitantra and Strroga, Amrita School of Ayurveda, Clappana, P.O-690525, Kollam, Kerala, India.
E-mail: drhemavathi.sk@gmail.com
Chronic pelvic pain presents as a main symptom in 71%-87% cases with endometriosis, a disease in which the endometrial glands and stroma grow outside the uterine cavity. The management modalities to cope with the long-standing, frustrating pelvic pain are still not reassuring. Ayurveda can provide an effective pain management protocol, though a single correlation of endometriosis cannot be made from the classical background. In the present case, a 44-year-old woman who was suffering from severe chronic pelvic pain since 20 years was managed using a definite Ayurvedic treatment protocol including shodhana (cleansing) procedure for 21 days and shamana (internal medications) for two months. The whole treatment period spanned for a total of nine months including a follow-up of six months. The patient reported a considerable improvement in her condition after the treatment.
Satapuspa taila, Uttarabasti, Vatiki yonivyapad, Yogabasti
Case Report
A 44-year-old female reported to the Outpatient Department (OPD) in February 2014 for the management of 20 years of chronic pelvic pain diagnosed as endometriosis, requiring continuous medication. Previous specialised evaluations included Magnetic Resonance Imaging (MRI) which demonstrated small uterine fibroid and right complex ovarian cyst that possibly be a haemorrhagic/endometriotic cyst.
The patient said that the pelvic pain starts 5-6 days prior to menstruation and stops 1-2 days after onset of bleeding, since 20 years. The pain is most severe on the first day of the menstrual cycle. She also had passage of clots during menstruation since 21 years. She was diagnosed with having ovarian cyst and advised to take Oral Contraceptive pills (OC pills) in the year 1997 which she continued for 1½ years. On medication, she got temporary relief from the symptoms which reappeared on stoppage of OC pills.
She denied taking OC pills and resorted to Over The Counter (OTC) Non-Steroidal Anti-Inflammatory Drug (NSAID) for the management of pain, from 1999 to 2012. The pain aggravated and she was advised for an MRI scan in April 2013 which showed an ovarian cyst (endometriotic cyst/haemorrhagic cyst) and small uterine fibroid. After which she was advised by the gynaecologist to have OC pills for three months. The chronic unbearable pain made her visit OPD on first week of February 2014 and got admitted on 17th February 2014.
She was diagnosed with depression and was under Selective Serotonine Reuptake Inhibitor (SSRI) group of antidepressants (VENLAFAXINE 300 mg) and vitamin B12 since 2004. She underwent appendicectomy in 1989 and cholecystectomy in 1999.
She was unmarried but a non-virgin without having any habits or addictions. Her family history revealed that her mother was advised for hysterectomy for uterine fibroid and Stage 1 ovarian carcinoma. Her personal history revealed a constipated bowel habit and disturbed sleep. She attained menarche at the age of 15 years with duration of 3-4 days and an interval of 25-32 days. Her Last Menstrual Period (LMP) was on 13/2/2014. Amount of bleeding was excessive on second day evident from the usage of four to five heavily soaked pads.
On examination, she was calm and pain-free. Her blood pressure was 120/80 mmHg, pulse rate 70/minute and BMI 23.3 kg/m2. She is of vata pitta prakriti, (constitution based on bodily humour) with madhyama satva (mental constitution). Her physical examination didnot reveal any abnormal findings. External genitalia didn’t reveal any abnormal findings. Her laboratory results for CA-125 was 26 U/mL. Per speculum examination showed a healthy nulliparous cervix without any significant abnormality. Bimanual examination revealed an anteverted mobile uterus with a negative Cervical Motion Tenderness (CMT). Medical history of the patient are detailed in [Table/Fig-1].
| Year | Clinical events and intervention |
|---|
| 1989 | Appendicectomy |
| 1995 | Onset of passage of clots during menstruation |
| 1996 | Onset of pelvic pain which begins 5-6 days prior to menstruation was under OTC analgesics |
| 1997 | Diagnosed of ovarian cyst and started OC pills for 1½ years |
| 1999 | Cholecystectomy |
| 1999-2012 | Pelvic pain associated with menstruation still persisted for which she took OTC analgesics |
| 2013 | Pelvic pain aggravated and underwent MRI and took OC pills for three months |
| 2014 | Started taking Ayurvedic treatment |
OTC: Over the counter; OC: Oral contraceptives; MRI: Magnetic resonance imaging
A probable diagnosis, vatiki yonivyapat/udavartini yoni vyapat (gynaecological conditions in Ayurveda which includes painful menstruation) was drawn out from the presenting complaints and the previous medical reports produced by the patient during the first OPD visit on 2nd February 2014. She was advised for admission on the fifth day of next menstrual cycle. General Quality Of Life (QOL) was measured by Endometriosis Health Profile Questionnaire (EHP-30 core questionnaire) [1] and pain intensity of the first day of menstrual cycle by using Visual Analogue Scale (VAS) [2] was done on the day of admission, 17th February 2014. Her baseline VAS grading (of 1st day of menstrual cycle) was 10 and QOL was 87% impaired.
Therapeutic plan was to perform shodhana karma (cleansing therapies) after correcting her agni (digestive fire) by purvakarma (preparatory therapies). Initially, Vaishvanara churna (12 g) [3] was given for improving the digestive fire prior to cleansing therapy for two days. Oral administration of Mahanarayana taila [4] was started thereafter with a dosage of 25 mL and the dose was incremented based on the digestive fire, continued until it reached 140 mL on the seventh day. Virechana (purgation) [5] was performed with the administration of Trivrit leha [6]. After purgation therapy, she was subjected to yogabasti [7] (medicated enema) and uttarabasti [8] (intrauterine installation of medicated formulation).
After completion of cleansing therapy, she was discharged from the hospital after 21 days and was advised to take Satapuspa taila [9] (oil prepared out of Anethum sowa) orally 5 mL twice daily before food for two months [Table/Fig-2] [10-12].
Treatment protocol {shodhana (cleansing procedure}.
| Treatment procedure | Method of administration | Treatment duration |
|---|
| Dipana, pachana [10], with Vaisvanara curna | 10 g twice daily before food with warm water | Day 1-2 |
| Snehapana [11] with Mahanarayana taila | Arohana krama after assessing Agni and Koshtha, maximum dose was 140 mL | Day 3-8 |
| Snehana and svedana [12] | Sarvanga abhyanga with Dhanvantara taila followed by nadi sveda. | Day 9-11 |
| Mridu virechana with trivrt leha | Trivrt leha -25 g given at 7 am | Day 12 |
| Rest | | Day 13 |
| Yogabasti | Niruha basti with 750 mL of Dasamula kshara basti and Anuvasana basti with 75 mL of Dhanvantara taila and 75 mL of Sahacaradi taila | Day 14-21 |
| Uttarabasti | Uttarabasti with 3 mL Satapuspa taila into the uterine cavity on the day of Anuvasana vasti |
Primary outcome measure change from baseline (before treatment value), in intensity of chronic pelvic pain of 1st day of menstrual cycles were measured by VAS grading (at baseline and at 1st, 2nd, 3rd menstrual cycles after inclusion in to the clinical study) on the fifth day of menstrual cycle as shown in [Table/Fig-3]. QOL as measured by EHP 30 core questionnaire during first second and third menstrual cycles (after treatment) were 4%, 12%, 12% respectively.
Intensity of pain assessed with visual analogue scale: Before Treatment (BT)=10.
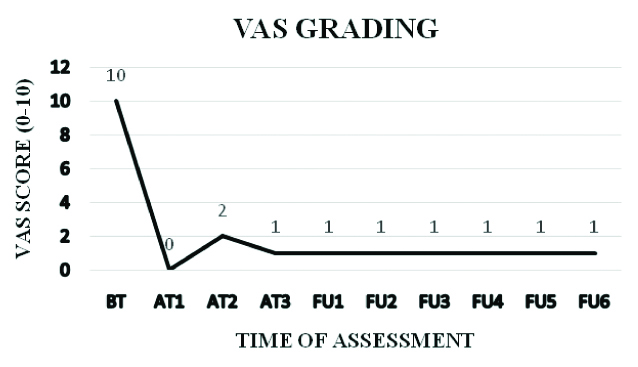
After six months of follow-up, there have been no further episodes of pelvic pain and the assessment was repeated at six menstrual cycles (at 4th, 5th, 6th,7th, 8th and 9th menstrual cycles without medicines), shown in [Table/Fig-3]. On her 3rd follow-up, an MRI was repeated which showed normal right and left ovary with a dominant follicle in the right ovary.
After 1st month Treatment (AT1)=0; After 2nd month Treatment (AT2)=2; After 3rd month Treatment (AT3)=1; 1st Follow-Up (FU1)=1; 2nd Follow-Up (FU2)=1; 3rd Follow-Up (FU3)=1, 4th Follow-Up (FU4)=1, 5th Follow-Up (FU5)=1, 6th Follow-Up (FU6)=1.
Discussion
The gynaecological reasons of chronic pelvic pain are diverse. This diversity ends in the clinical diagnosis of endometriosis in about one-third of the cases during their reproductive period [13].
Based on the evidence that bodily metabolism can play a vital role in the management of pain, there is an increasing trend among the chronically ill patients approaching the alternative system of medicine [14]. Endometriosis cannot be codified under a single disease entity according to Ayurveda classics. our Acarya’s have emphasised on lakshanas like shula, ruk throughout the striroga prakarana, among which vatiki yoni vyapad [15], udavartini yoni vyapad [15] bear close resemblance to the clinical picture of endometriosis, which makes finding an effective, validated treatment protocol for the management of pain in endometriosis.
After a definitive diagnosis of endometriosis has been made out for those suffering from chronic pelvic pain, the patients are forced to travel through the traumatic paths of long-term medication leading to frustration and depression. One of the greatest challenges faced by the physicians and patients alike is lack of awareness on effective pain management described in the Ayurveda texts. Ayurveda has been viewing infertility associated with endometriosis more seriously in recent years. However, there is a wider area of research open for an effective pain management associated with endometriosis. The present case report emphasises the importance of an Ayurvedic treatment protocol for the management of pelvic pain connected with endometriosis. Though, laparoscopy has been accepted as the ultimate in diagnosis and assessment of the disease, it was avoided in the present case report due to the concern of the patient. The treatment protocol aims for a pacification of vata dosha and correction of digestive fire thereby abolishing the chronic pelvic pain associated with endometriosis. The site-specific action of Mahanarayana taila with its shulahara property (analgesic) which was used for internal oleation can be attributed as an added advantage for the further cleansing therapies. Due to the unavoidable role of vata-dosha in the present disease entity, the cleansing therapies like purgation and enema procedures hold prime importance for the pacification of vata dosha. A course of medicated enema with intrauterine instillation of medicated formulation has been selected after purgation giving due importance to the analgesic properties of the drugs. The usage of oil prepared out of Anethum sowa internally which possess a cleansing action on channels can be attributed for the subsidence of pain in the subsequent menstrual cycles.
Conclusion
The Ayurvedic management protocol was effective in managing the chronic pelvic pain associated with endometriosis. The present case as a stepping stone for future research works on Ayurvedic pain management in gynaecological cases.
OTC: Over the counter; OC: Oral contraceptives; MRI: Magnetic resonance imaging
[1]. Jones G, Kennedy S, Barnard A, Wong J, Jenkinson C, Development of anendometriosis quality-of-life instrument: the Endometriosis Health Profile-30Obstet Gynaecol 2001 98:258-64.10.1016/S0029-7844(01)01433-8 [Google Scholar] [CrossRef]
[2]. Larroy C, Comparing visual-analog and numeric scales for assessing menstrual painBehav Med 2002 27:179-78.10.1080/0896428020959604312165972 [Google Scholar] [CrossRef] [PubMed]
[3]. Krishnan Vaidyan, Sahasrayogam 2009 28th editionAlappuzhaVidyarambham Publishers:190 [Google Scholar]
[4]. Mishra Siddhinandana, editor. Bhaishajya Ratnavali of Govinda Dasa Sen, repr. Chikitasthana, chapter 26, Verse.325-336. Chaukhambha Samskrita Sansthana, Varanasi, 2011. Pp. 547 [Google Scholar]
[5]. Acharya YT, Charaka Samhita of Acharya Agnivesa 2010 VaranasiChaukamba Surabharathi Prakashana:537 [Google Scholar]
[6]. Kunte Moreshwar Anna. Ashtanga Hrudaya of Vagbhata, Chaukamba Surabharathi Prakashana; Varanasi, 2017. p. 742 [Google Scholar]
[7]. Mitra Jyothi, Ashtanga samgraha of Vridha Vagbhata4th editionVaranasiChaukhambha Sanskrit Series Office:221 [Google Scholar]
[8]. Acharya YT, Susruta Samhita of Susruta 2005 8th editionVaranasiChaukhambha Orientalia:539 [Google Scholar]
[9]. Tewari PV, Kashyapa Samhita of Vridha Jeevaka 2004 VaranasiChaukhambha Viswa Bharati:348 [Google Scholar]
[10]. Murthy Srikantha, Sarangadhara Samhita of Sarangadhara 2012 VaranasiChaukhambha Orientalia:17 [Google Scholar]
[11]. Acharya YT, Charaka Samhita of Agnivesha 2011 VaranasiChaukamba Surabharathi Prakashana:677 [Google Scholar]
[12]. Sharma PV, Charaka Samhita of Agnivesha 2010 VaranasiChaukhambha Orientalia:15 [Google Scholar]
[13]. Triolo O, Laganà AS, Sturlese E, Chronic pelvic pain in endometriosis: an overviewJ Clin Med Res 2013 5(3):153-63.10.4021/jocmr1288w23671540 [Google Scholar] [CrossRef] [PubMed]
[14]. Doty E, Attaran M, Managing primary dysmenorrheaJ Pediatr Adolesc Gynaecol 2006 19:341-44.10.1016/j.jpag.2006.06.00517060018 [Google Scholar] [CrossRef] [PubMed]
[15]. Acharya YT, Charaka Samhita of Agnivesha 2004 VaranasiChaukamba Surabharathi Prakashana:635 [Google Scholar]