Dupuytren’s Contracture: Epidemiological Patterns and Results Following Radical Fasciectomy
Swagat Mahapatra1, Sachin Awasthi2, Pankaj Aggarwal3, SS Tripathy4, Rajiv Ratan Singh Yadav5, Chandrasekhar Verma6, Siddharth Tiwari7
1 Assistant Professor, Department of Orthopaedics, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
2 Associate Professor, Department of Orthopaedics, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
3 Assistant Professor, Department of Orthopaedics, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
4 Associate Professor, Department of Emergency Medicine, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
5 Associate Professor, Department of Emergency Medicine, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
6 Senior Resident, Department of Orthopaedics, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
7 Senior Resident, Department of Orthopaedics, Dr RML Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sachin Awasthi, Gomti Nagar, Lucknow-226010, Uttar Pradesh, India.
E-mail: sachinavasthi4778@gmail.com
Introduction
Dupuytren’s disease is a debilitating condition, affecting the palmar fascia of the hand. Patients develop a flexion contracture and have difficulties in activities of daily living. Treatment is usually surgical, and a wide range of options are available.
Aim
To study the epidemiological parameters associated with Dupuytren’s contracture and to study the results following Radical Fasciectomy.
Materials and Methods
This was a prospective, interventional, institutional based study conducted at Dr RML Institute of Medical Sciences. A total of 26 patients with Dupuytren’s disease, fulfilling the inclusion criteria, were treated with radical fasciectomy. Epidemiological parameters and postoperative improvement in form of Digitopalmer Distance (DPD), extension lag and Quick DASH scores were recorded. Data was analysed using SPSS version 21 software. Continuous data was analysed by student’s t-test and categorical data was analysed by chi-square test and p-value less than 0.05 was considered as significant.
Results
Mean age of involvement in the present study was 54.82±7.34 years. An 84% (22 patients) of patients were male and 16% (4 patients) female. Bilateral hand involvement was seen in 84.61% and single hand involvement was seen in 15.38%. Dominant hand involvement was seen in 69.23% cases, nondominant hand in 15.38% cases and bilateral hands equally in 15.38% cases. Thenar Band and Commissural Band was noticed in 19% of cases. A total of 27% of all cases were diabetics, and 15% were known smokers. One patient in the entire series was a known epileptic on medications. DPD following surgery at two weeks and three months postoperatively was satisfactory as more than 60% of patients had full closure and more than 90% had a DPD of less than two centimeters. Extension Lag at MCP and PIP joints was found to be satisfactory as full opening at both MCP and PIP joints was found in more than 80% patients postoperatively at two weeks and three months.
Conclusion
Outcomes following radical fasciectomy are very encouraging in terms of functional results as well as patient satisfaction. Intensive hand therapy during the first two weeks in the postoperative period gives best functional results.
Epidemiology, Flexion contracture, Palmer fascia
Introduction
Dupuytren’s Disease has been described as a fibromatosis of the palmar fascia of the fingers and hand, which usually leads to loss of full extension. Patients may develop problems using their hands in daily activities. The cause of this condition is not yet completely understood. However, smoking, excessive alcohol consumption, male gender, diabetes mellitus, epilepsy and possibly performing heavy manual labor increase the chances of getting the disease [1].
Dupuytren’s disease is an ancient affliction of unknown origin. The disease has been described to have originated with the Viking and spread through Northern Europe and other continents. Dupuytren’s disease was named in the early 1800’s after a famous French surgeon, Baron Guillaume Dupuytren [1]. The disease has high preponderance in the Scandinavian population of northern Europe [2]. Dupuytren’s is rare in Indian and African populations [2]. It was first medically described by Dr. Felix Platter, a French surgeon [1]. Initially, conditions like Dupuytren’s, Ledderhose, Peyronie’s and Garrod’s Pads were all viewed as separate diseases [3]. In 1902 Janssen described a fibromatous diathesis, with the understanding that these similar conditions were due to the same underlying cause, often grouped as Dupuytren’s diathesis [4-7]. Surgical techniques have evolved from simple dermo-fasciotomy (cutting through skin and cord) to a much wider range of options. Closed fasciotomy, open fasciotomy, partial fasciectomy, dermo-fasciectomy and many choices in-between. Radiotherapy as a method of treatment was introduced in Germany. It is used in the early stages, with only nodules without contractures [8]. Collagenase injections were first described by Badalamente MA et al., and have been commercially available since the early part of last decade [9]. Myofibroblasts producing TGF β have been implicated in the pathogenesis of this condition in recent literature [10,11]. This study has been done to study the epidemiological parameters associated with this disease and also study the results following Radial Fasciectomy. All methods of treatment of Dupuytren’s disease have high recurrence rates. Radical fasciectomy involves complete removal of all diseased fascia from the involved palm using multiple incisions if required. Theoretically, it has lesser recurrence rate but has higher postoperative morbidity. This study throws a light on the epidemiological associations as well as the functional results following fasciectomy.
Materials and Methods
This study was conducted at Dr. Ram Manohar Lohia Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. It was a prospective, interventional, institutional study. After adequate institutional review board clearance, study was undertaken. All patients presenting to orthopaedic Outpatient department from January 2016-December 2017 with Dupuytren’s contracture and consenting for surgery were included. Written consent was taken from every patient prior to surgery. We reviewed 26 patients with Dupuytren’s Contracture who had been treated with radical Fasciectomy. Dupuytren’s being a relatively less common entity; all the patients who presented to our setup were considered as the sample size. We collected information as to the age and sex distribution, patterns of involvement of the fingers, associated co-morbidities, occupation, etc. The data were collected from charts, physical assessment slips, and discharge summaries.
The Inclusion criteria were Total Passive Extension Deficit (TPED) of at least 30 degrees (MCP, PIP OR DIP) and the existence of a well-defined cord preoperatively. The exclusion criteria included patients who had surgery for Dupuytren in the same hand, patients unfit for surgery and patients opting for any other specific modality of treatment. The Tubiana Classification [12] of Dupuytren’s Contracture of the fingers was used as the scoring system [Table/Fig-1].
Tubiana classification of dupuytren’s contracture.
| Tubiana I | TPED of 0-45° |
| Tubiana II | TPED of 45-90° |
| Tubiana III | TPED of 90-135° |
| Tubiana IV | TPED of ≥135° |
| TPED=PEDMCP+PEDPIP+PEDDIP |
TPED: Total passive extension deficit; PED: Passive extension deficit; MCP: Metacarpophalangeal; PIP: Proximal interphalangeal; DIP: Distal interphalangeal joint
The deficit in flexion was recorded by measuring the distance between distal palm crease and fingertips while making a fist. Sensibility was tested using Semmes-Weinstein monofilaments. Also, the presence of knuckle pads; the presence or absence of fatty tissue between the cord and the skin distal to the distal palmar crease, indicating that the digital nerve possibly was relocated by a spiral cord; and the presence or absence of foot and penis involvement were recorded. After adequate blood investigations and pre-anesthetic clearance, patients were operated by radical palmar fasciectomy by standard approach [Table/Fig-2,3,4,5,6,7 and 8]. The patients were kept admitted in the ward for five days postoperatively when wound inspections were done, and daily bedside therapy was started. Following discharge, patients were followed up in hand therapy for two weeks daily. Following that patients were asked to review every month for first three months followed by every three months for a year. During follow-up, the patients were asked to fill the Abbreviated DASH questionnaire and extension Lag, and Finger Closure by DPD was measured. The full DASH consists of 30 questions. Also, there are two optional scales of the DASH (sport/music and work). Each item in the disability/symptom scale has 5 responses. If at least 27 of the 30 items are completed, a score can be calculated.
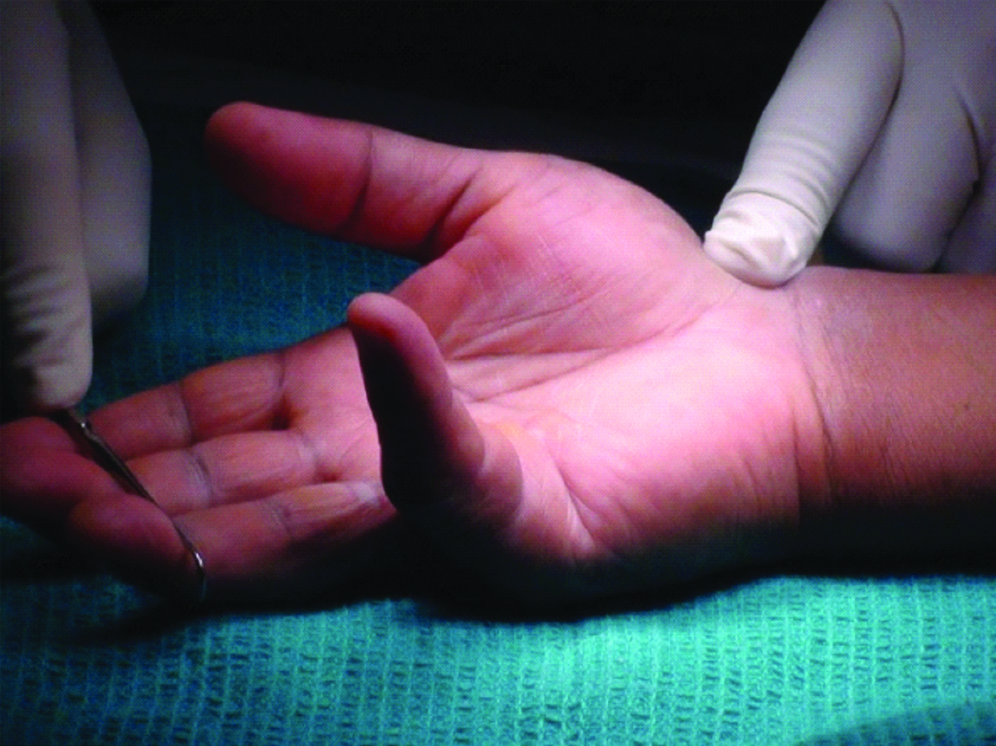
Preoperative deformity of right little finger.
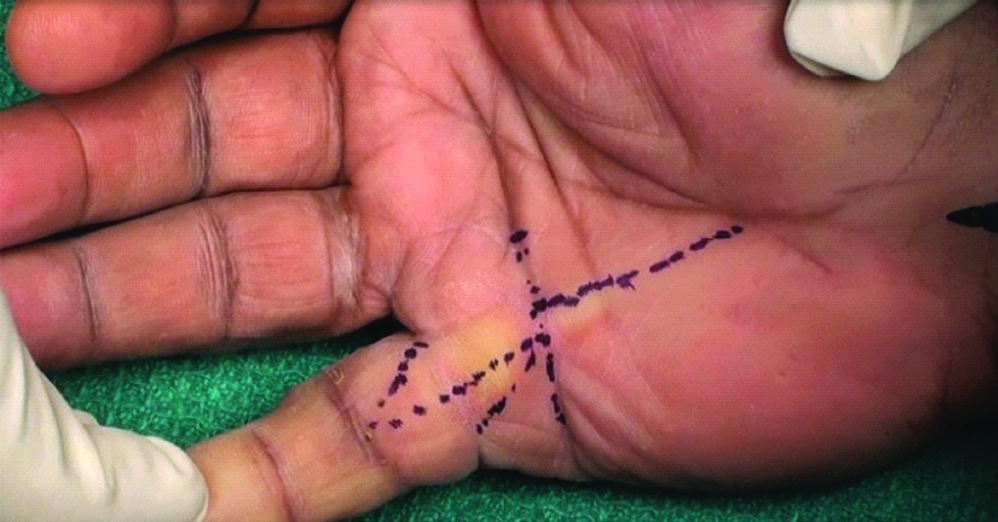
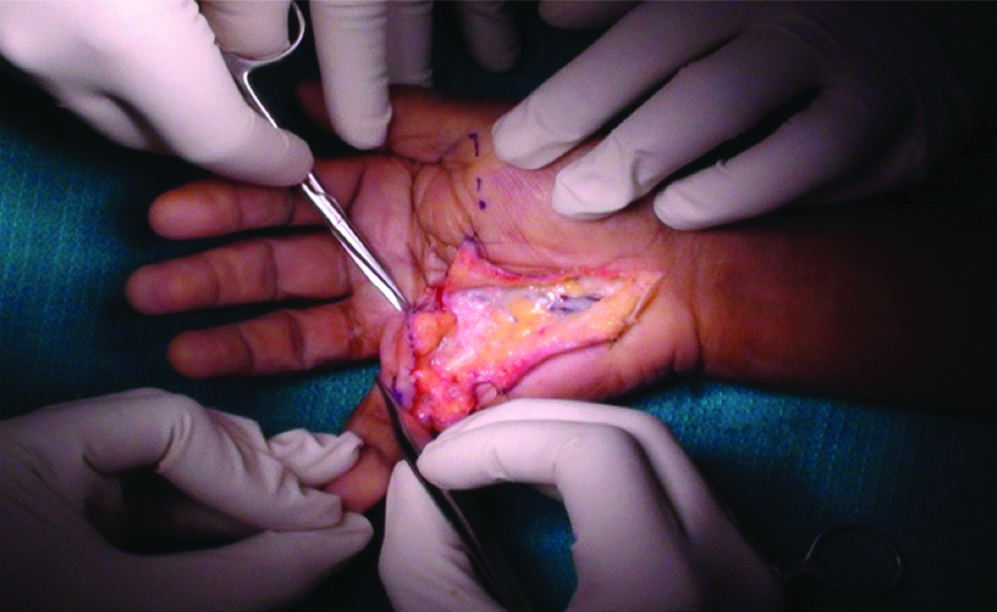
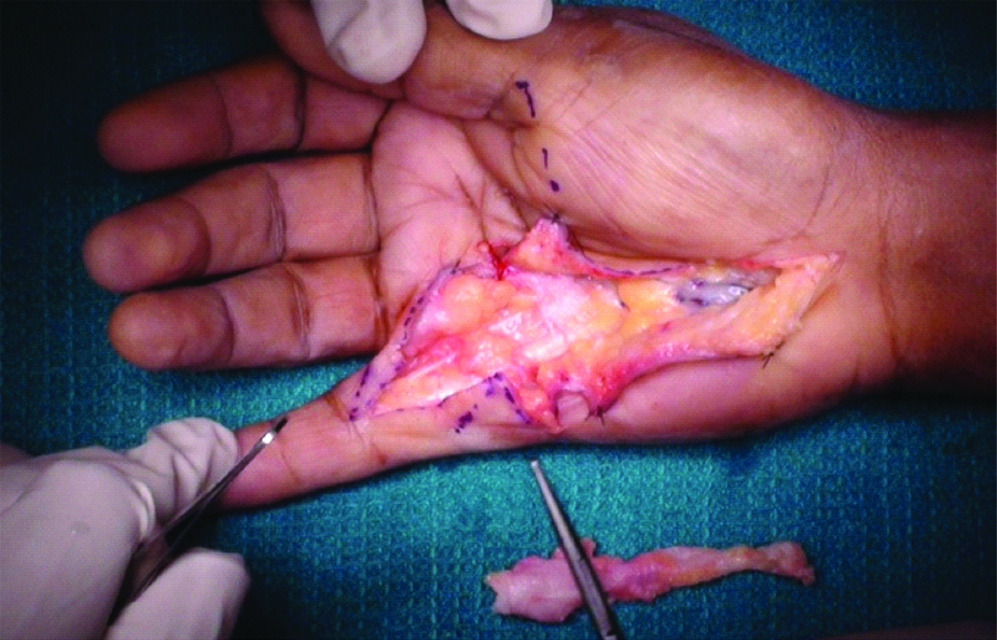
Offending cord identified and dissected.
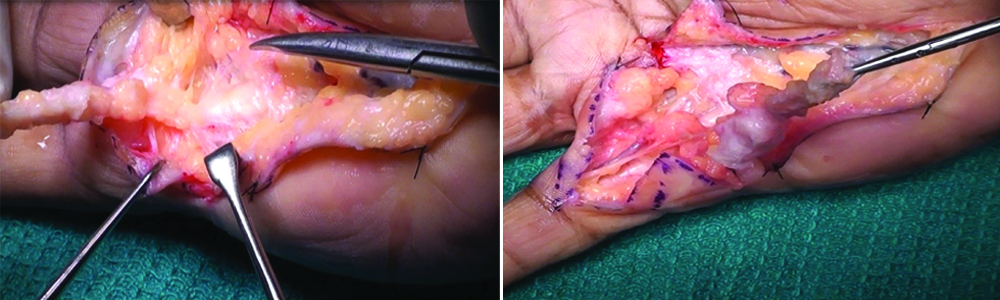
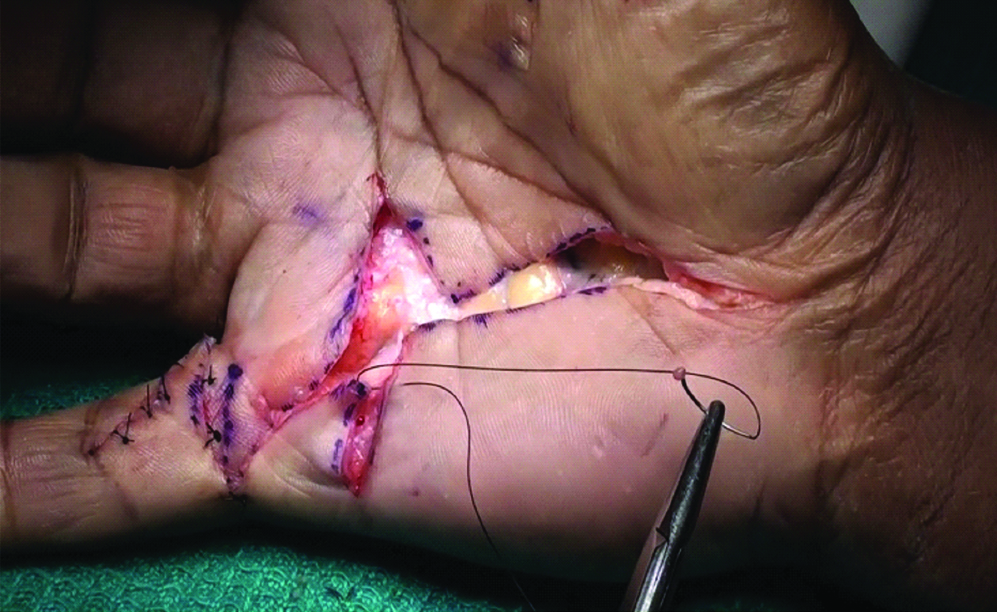
Offending cord excised and passive correction checked.
Quick DASH has 11 items. To calculate a score at least 10 out of the 11 questions must be answered. Each question has 5 response options. Scale scores are calculated, ranging from 0 (no disability) to 100 (most severe disability) [13].
Statistical Analysis
Data was entered into excel sheets, and statistical analysis of the data was done using SPSS version 21 software. Continuous data were reported as mean±standard deviation. Categorical data were reported as numbers and percentages and were analysed using Chi-square test or Fisher’s-exact test as appropriate. The value p<0.05 was considered statistically significant.
Results
A total of 26 patients who fulfilled the inclusion criteria were included in the study. Mean age of involvement in the present study was 54.82±7.34 years. The youngest patient was 38 years old, and the oldest was 65-year-old [Table/Fig-9]. There were 84.61% (22 patients) male patients and 15.38% (4 patients) female patients [Table/Fig-9]. Bilateral hand involvement was seen in 84.61% (22 cases) and single hand involvement was seen in 15.38% (4 cases) [Table/Fig-10]. The disease was seen to affect the dominant hand in 69.23% cases (18 patients), non-dominant hand in 15.38% cases (4 patients) and bilateral hands equally in 15.38% cases (4 patients) [Table/Fig-10]. Thumb involvement in the form of Thenar Band and Commissural Band was noticed in 19% of cases [Table/Fig-10]. Regarding associations, 27% of all cases were diabetics [Table/Fig-9], and 15% were known smokers [Table/Fig-9]. Only one patient in the entire series was a known epileptic on medications and also a known case of Bipolar Disorder on Lithium [Table/Fig-9]. The DPD was calculated post surgery at two weeks and three months and values recorded in centimetres [Table/Fig-11]. The chi-square statistic was 0.7865. The p-value was 0.940244. The result was not significant and p>0.05 showing that there was no appreciable change of the DPD with time. The extension lag at metacarpophalangeal joint [Table/Fig-11] and proximal interphalangeal joint [Table/Fig-11] was measured in degrees at two weeks and three months postoperatively and recorded. The result was not significant at p>0.05 in both tables, showing that there is no appreciable change of the extension lag with time. These insignificant p-values suggest that the initial correction achieved during surgery and intensive therapy in the first two weeks were maintained. There was no appreciable improvement or worsening after that. Quick-DASH scores were calculated for all patients preoperatively and at six months follow-up [Table/Fig-12]. A higher quick-DASH score depicted worse outcome. The chi-square statistic was 30.2105 and the p-value was <0.00001, the result is significant at p<0.05. This denotes the improvement of patient outcomes as per quick-DASH scores after surgery.
Baseline characteristics of patients.
| Variable | Value |
|---|
| Age in years | Mean-54.82±7.34 |
| 11-20 | 0 |
| 21-30 | 0 |
| 31-40 | 2 |
| 41-50 | 9 |
| 51-60 | 9 |
| 61-70 | 6 |
| Sex Distribution | |
| Male | 22 (84.61%) |
| Female | 4 (15.38%) |
| Diabetic Association | |
| Diabetic | 7 (27%) |
| Non-Diabetic | 19 (73%) |
| Smoking Association | |
| Smoker | 4 (15.38%) |
| Non Smoker | 22 (84.61%) |
| Epilepsy Association | |
| Epileptic | 1 (3.84%) |
| Non Epileptic | 25 (96.15%) |
| Variable | Value |
|---|
| Hand Involvement | |
| Single Hand | 4 (15.38) |
| Both Hands | 22 (84.61) |
| Hand Dominance | |
| Dominant | 18 (69.23%) |
| Non Dominant | 4 (15.38%) |
| Both Equally | 4 (15.38%) |
| Thumb Involvement | |
| Thumb Involved | 5 (19.23%) |
| Thumb Not Involved | 21 (80.76%) |
Digitopalmar distance (DPD) and extensor lag (MCP joint and PIP joint) at post op 2 weeks and 3 months.
| Digitopalmar Distance | No of Pts 2 Weeks Post Op | No of Pts 3 Months Post Op | p-value |
|---|
| Full Closure (0 cm) | 13 | 16 | The chi-square statistic is 0.7865. The p-value is 0.940244. The result is not significant at p>0.05. |
| 0-1 cm | 7 | 5 |
| 1-2 cm | 4 | 3 |
| 2-3 cm | 1 | 1 |
| >3 cm | 1 | 1 |
| Extensor Lag (Degrees)-MCP | No of Pts 2 Weeks Post Op | No of Pts 3 Months Post OP | p-value |
| Full Opening-0° | 21 | 20 | The chi-square statistic is 0.3577. The p-value is 0.98579. The result is not significant at p>0.05 |
| 0-10° | 2 | 2 |
| 10-20° | 1 | 2 |
| 20-30° | 1 | 1 |
| >30° | 1 | 1 |
| Extensor Lag (Degrees)-PIP | Post Op -2 Weeks | Post Op- 3 Months | p-value |
| Full Opening-0° | 21 | 20 | The chi-square statistic is 1.2308. The p-value is 0.873007. The result is not significant at p>0.05. |
| 0-10° | 2 | 2 |
| 10-20° | 1 | 2 |
| 20-30° | 1 | 1 |
| >30° | 1 | 1 |
The chi-square statistic is 0.7865. The p-value is 0.940244. The result is not significant at p>0.05.
Quick-DASH scores at long term follow-up.
| Quick-Dash Score | No. of Patients-Pre Op | No. of Patients-Post Op |
|---|
| 0-25 | 1 | 18 |
| 26-50 | 4 | 5 |
| 51-75 | 4 | 2 |
| 76-100 | 17 | 1 |
| Total | 26 | 26 |
The chi-square statistic is 30.2105. The p-value is <0.00001. The result is significant at p<0.05.
Discussion
Contrary to the previous opinion that Dupuytren’s contracture is rare in the Indian subcontinent; our observation in this geographical area was different. This is probably the largest of the series reported from India. The earlier one being reported by Srivastava S et al., comprising of ten cases [14]. There have been 49 studies since 1951 regarding the epidemiology and prevalence of Dupuytren’s disease in various geographic areas with different observations [4]. The highest prevalence has been found in Scandinavia and the British Isles as per Gudmundsson KG et al., in the Reykjavik study [15]. In this study, bilateral hand involvement in 85% cases and one hand in another 15% was found. The dominant hand is involved more commonly in our study. Similar to this, a predilection for the right hand has also been reported by Mansur HC et al., [16]. Zeajic D et al., observed that changes were equally found in both hands in women, but were found more than three times as often in the right hand as compared to the left in men [17]. Thumb involvement has not been reported much in literature. In the present study, 19% of cases have thumb involvement in the form of thenar band and commissural band. Our study shows no correlation between disease process and smoking. This is similar to conclusion of Bergenudd H et al., [18]. However, Burge P et al., have shown a correlation between smoking habits and Dupuytren’s [19]. Many studies by Gudmundsson KG et al., and Burge P et al., reported a relationship between alcohol consumption and Dupuytren’s disease [15,19]. In this study and few other studies like Bergenudd H et al., no significant correlation between alcohol consumption and Dupuytren’s disease was found [18]. Around 27% of cases in our study suffered from Diabetes mellitus. This is similar to findings of Arkilla PE et al., and Hart MG et al., who have shown a strong association of Dupuytren’s with Diabetes [20,21]. One case of Dupuytren’s associated with Epilepsy was recorded. This is usually explained by the fact that long-term use of antiepileptic drugs causes the peripheral stimulation of tissue growth factors. This has been shown by Hart MG et al., in their study on antiepileptics and Dupuytren’s [21]. There are no similar studies which have analysed the functional results following Radical fasciectomy. Functional results following Radical Fasciectomy in Dupuytren’s in this study has been seen by measurement of DPD and extension Lag at MCP joints and PIP joints. DPD following surgery at two weeks postoperatively and three months postoperatively was satisfactory as more than 60% of patients had full closure and more than 90% had a DPD of less than two centimeters. However, on comparing the number of patients in a particular range of DPD at two weeks and three months, we obtained a p-value which was non-significant, denoting that, maximum correction and return of function were achieved postoperatively and within the first two weeks of therapy. There was not much appreciable improvement after that. The other indicator used was the Extension Lag at MCP and PIP joints, and that too was found to be satisfactory as full opening at both MCP and PIP joints was found in more than 80% patients at postoperative two weeks and three months. A similar trend was observed in Extension lag measurement when compared at two weeks and three months postoperatively. At both MCP and PIP joints the p-values were non-significant. This also confirms our theory that maximum correction and return of function was achieved postoperatively and within the first two weeks of therapy. There was significant improvement in QuickDASH scores postoperatively showing appreciable patient satisfaction as well as functional recovery.
Limitation
The sample size of present study was small. But Dupuytren’s contracture being a relatively uncommon disease and also highly neglected, the number of patients seeking treatment is less. Also, the epidemiological associations noticed in the present study could have been better analysed if data were collected in multiple centers over a wider geographical distribution instead of a single centre.
Conclusion
Present study is probably the most extensive series reported from India. It can be concluded from this study that Dupuytren contracture is found predominantly in males and bilateral involvement is common. Association with smoking, alcohol is uncommon. Patterns of affection are similar as in other populations, but thumb involvement with thenar band is more common in Indian community. The maximum correction and return of function are achieved immediately postoperatively and within the first two weeks of therapy. So good patient counseling and intensive hand therapy is very essential in the immediate postoperative period for better outcomes. Results following radical fasciectomy are very encouraging in terms of functional results as well as patient satisfaction.
TPED: Total passive extension deficit; PED: Passive extension deficit; MCP: Metacarpophalangeal; PIP: Proximal interphalangeal; DIP: Distal interphalangeal joint
The chi-square statistic is 0.7865. The p-value is 0.940244. The result is not significant at p>0.05.
The chi-square statistic is 30.2105. The p-value is <0.00001. The result is significant at p<0.05.
[1]. Elliot D, The early history of Dupuytren’s diseaseHand Clin 1999 15:1-19. [Google Scholar]
[2]. Mikkelsen OA, Epidemiology of a Norwegian population. In: McFarlane RM, McGrouther DA, Flint MH, editorsDupuytren’s Disease: Biology and Treatment 1990 New YorkChurchill Livingstone:191 [Google Scholar]
[3]. Whaley DC, Elliot D, Dupuytren’s disease: a legacy of the northJ Hand Surg [Br] 1993 18:363-67.10.1016/0266-7681(93)90065-N [Google Scholar] [CrossRef]
[4]. Hindocha S, McGrouther DA, Bayat A, Epidemiological evaluation of Dupuytren’s disease incidence and prevalence rates in relation to etiologyHand (NY) 2009 4(3):256-69.10.1007/s11552-008-9160-919145463 [Google Scholar] [CrossRef] [PubMed]
[5]. Rayan GM, Ali M, Orozco J, Dorsal pads versus nodules in normal population and Dupuytren’s disease patientsJ Hand Surg Am 2010 35:1571-79.10.1016/j.jhsa.2010.06.00120800974 [Google Scholar] [CrossRef] [PubMed]
[6]. Trybus M, Bednarek M, Budzyński P, Gniadek M, Lorkowski J, Concomitance of Ledderhose’s disease with Dupuytren’s contractureOwn experience. Przegl Lek 2012 69(9):663-66. [Google Scholar]
[7]. Gudmundsson KG, Jónsson T, Arngrímsson R, Association of MorbusLedderhose with Dupuytren’s contractureFoot Ankle Int 2013 34(6):841-45.Epub 2013 Feb 510.1177/107110071347535223386754 [Google Scholar] [CrossRef] [PubMed]
[8]. Keilholz L, Seegenschmiedt MH, Sauer R, Radiotherapy for prevention of disease progression in early-stage Dupuytren’s contracture: initial and long-term resultsInt J Radiat Oncol Biol Phys 1996 36(4):891-97.10.1016/S0360-3016(96)00421-X [Google Scholar] [CrossRef]
[9]. Badalamente MA, Hurst LC, Enzyme injection as nonsurgical treatment of Dupuytren’s diseaseJ Hand Surg Am 2000 25(4):629-36.10.1053/jhsu.2000.691810913202 [Google Scholar] [CrossRef] [PubMed]
[10]. Bisson MA, McGrouther DA, Mudera V, Grobbelaar AO, The different characteristics of Dupuytren’s disease fibroblasts derived from either nodule or cord: expression of alpha-smooth muscle actin and the response to stimulation by TGF-beta1J Hand Surg Br 2003 28(4):351-56.10.1016/S0266-7681(03)00135-9 [Google Scholar] [CrossRef]
[11]. Wong M, Mudera VJ, Feedback inhibition of high TGF-beta1 concentrations on myofibroblast induction and contraction by Dupuytren’s fibroblastsHand Surg Br 2006 31(5):473-83.10.1016/J.JHSB.2006.05.00716875762 [Google Scholar] [CrossRef] [PubMed]
[12]. Tubiana R, Dupuytren’s disease of the radial side of the handHand Clin 1999 15(1):149-59. [Google Scholar]
[13]. Beaton DE, Wright JG, Katz JN, Development of the QuickDASH: comparison of three item-reduction approachesJ Bone Joint Surg Am 2005 87:1038-46.10.2106/JBJS.D.0206015866967 [Google Scholar] [CrossRef] [PubMed]
[14]. Srivastava S, Nancarrow JD, Cort DF, Dupuytren’s disease in patients from the Indian sub-continent report of ten casesJ Hand Surg [Br] 1989 14:32-34.10.1016/0266-7681(89)90009-0 [Google Scholar] [CrossRef]
[15]. Gudmundsson KG, Arngrimsson R, Sigfusson N, Bjornsson A, Epidemiology of Dupuytren’s Disease. Clinical, serological and social assessment. The Reykjavik StudyJ Clin Epidemiol 2000 53:291-96.10.1016/S0895-4356(99)00145-6 [Google Scholar] [CrossRef]
[16]. Mansur HC, Oliveira ED, Gonçalves CB, Epidmiological analysis of patients with Dupuytren’s diseaseRev Bras Ortop 2018 53(1):10-14.10.1016/j.rbo.2016.08.01229367900 [Google Scholar] [CrossRef] [PubMed]
[17]. Zerajic D, Finsen V, Dupuytren’s disease in Bosnia and herzegovnia-An Epidemiological studyBMC Musculoskeletal Disorders 2004 5:1010.1186/1471-2474-5-1015050031 [Google Scholar] [CrossRef] [PubMed]
[18]. Bergenudd H, Lindgarde F, Nilsson BE, Prevalence of Dupuytren’s and its correlation with degenerative changes of hands and feet and with criteria of general healthJ hand Surg 1993 18[Br]:254-57.10.1016/0266-7681(93)90123-W [Google Scholar] [CrossRef]
[19]. Burge P, Holy G, Regan P, Milne R, Smoking, alcohol and risk factor of dupuytren’s contractureJBJS Br 1997 79B:206-10.10.1302/0301-620X.79B2.6990 [Google Scholar] [CrossRef]
[20]. Arkilla PE, Kantola IM, Vikari JSA, Dupuytren’s disease: association in chronic diabetic complicationsJ Rheumatology 1997 24:153-59. [Google Scholar]
[21]. Hart MG, Hooper G, Clinical associations of Dupuytren’s diseasePostgraduate Medical Journal 2005 81:425-28.10.1136/pgmj.2004.02742515998816 [Google Scholar] [CrossRef] [PubMed]