Rotational Malalignment after Intramedullary Fixation of Trochanteric Fractures
Rajendra Annappa1, Harramb Mittal2, Surendra Umesh Kamath3, Santhosh Rai4, Pooja Kundapur Suresh5, Nabeel Mohammed6
1 Assistant Professor, Department of Orthopaedics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Resident, Department of Orthopaedics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor, Department of Orthopaedics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 Associate Professor, Department of Radiology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 Associate Professor, Department of Pathology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
6 Resident, Department of Orthopaedics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajendra Annappa, Assistant Professor, Department of Orthopaedics, Kasturba Medical College, Manipal Academy of Higher Education, Manipal-576104, Karnataka, India.
E-mail: rajendra.orthopaedics@gmail.com
Introduction
Rotational malalignment after intramedullary fixation of fractures of the shaft of femur and tibia has been assessed by many studies but less frequently after intramedullary fixation of intertrochanteric fractures. Intertrochanteric fractures are managed by closed reduction in a traction table and fixation either by dynamic hip screw or proximal femoral nail under image intensifier. Reduction is checked intraoperatively by antero-posterior and lateral views with image intensifier in which rotational alignment cannot be assessed.
Aim
To study the rotational malalignment in the operated limb compared to normal limb by computed tomography (CT).
Materials and Methods
A prospective study was conducted on 70 patients at Kasturba Medical College and allied hospitals with intertrochanteric fractures with intramedullary fixation and with normal anatomy on opposite side. Postoperative CT with pelvis and knee was done and compared for rotational alignment.
Results
The mean anteversion on the normal side was 13.20. The mean anteversion on the operated side was 15.70. The mean rotational malalignment was 9.70; there was internal rotational deformity in 41 cases (58.6%) and external rotational deformity in 29 cases (41.4%) with Grade III malrotation in 17 (24.3%) cases.
Conclusion
Rotational malalignment postoperatively is frequently present and needs to be corrected intraoperatively by improving assessment methods.
Computed tomography evaluation, Proximal femoral nailing, Torsional deformity
Introduction
Orthopaedic surgeons frequently come across intertrochanteric fractures in day to day practice. Most patients with these fractures are elderly with osteoporosis and multiple co-morbidities. The goal of management plan is to achieve union with minimal complications [1]. Poor bone quality, compliance of patient and co-morbidities affect the functional outcomes but surgeons should minimise the morbidity associated with the fracture. This can be achieved by reasonable choice of implant for fracture type, identifying complex fracture patterns and performing proper reduction with ideal implant placement with a care for cost of treatment.
Intramedullary fixation is being done more commonly for intertrochanteric fractures. The use of cephalomedullary nails has increased, whereas use of dynamic hip screws has decreased although evidence in literature does not support that intramedullary devices give better results. Extramedullary dynamic hip screws were the choice of fixation from the 1950s to the 1990s, but many surgeons now prefer cephalomedullary nails with compression and anti-rotation screws in the femoral head. There has been an increasing trend to use of intramedullary nails, more than 20 fold since 1999 and about two-thirds of new orthopaedic surgeons now prefer them over sliding hip screw [1,2]. Different designs are available which are marketed by different manufacturers, each varying in length, diameter, neck-shaft angle and number of locking screws. Newer designs with ability to slide and/or compress and ability to control rotation are available [2].
In proximal femur fractures, displacement of fracture is based on fracture pattern. There is flexion and external rotation of proximal fragment due to pull of iliopsoas and abduction due to muscle action of glutei and external rotators. Hip adductors, flexors and extensors pull the distal fragment proximally resulting in a varus and external rotation. Due to this, there is possible internal malrotation if fracture is not adequately reduced intraoperatively [3].
Rotational malalignment or torsional deformity of the femur is expressed as a difference in femoral anteversion between the operated and normal limb. Postoperatively it can be measured clinically, by radiography, ultrasound and CT. CT has been proved to be a highly accurate method for rotational assessment by various studies [3-6]. Although torsional deformity after femoral shaft fracture fixation has been published by many authors, very few studies are done to assess rotational malalignment after cephalomedullary fixation of trochanteric fractures.
Variations in femoral anteversion have been well known in populations. However, a difference in femoral anteversion in right and the left side of any individual is minimal. When literature is reviewed for intertrochanteric fractures there are very few studies and exact incidence cannot be reported.
Materials and Methods
A prospective study was conducted in a tertiary care hospital, Kasturba Medical College and allied hospitals on 70 cases of intertrochanteric fractures with intramedullary fixation by proximal femoral nailing from June 2015 to January 2017. Pathological fractures, previous femoral neck or shaft fractures and patients not consenting for CT scan were excluded.
Patient was positioned supine on the traction table. Using image intensifier fluoroscopic images of normal hip and knee at same rotation of the C-arm were obtained and saved which could be used as a reference. Normal anteversion of the hip was determined which helped in assessing rotational alignment. Anteversion is the angle difference between the true lateral view of hip and knee. Fracture was reduced initially by traction along the longitudinal axis which distracted the fragments and corrected length and then by internal rotation. Once the fracture was provisionally reduced antero-posterior and lateral views were taken. In antero-posterior view, reduction of medial cortex and in lateral view, reduction of anterior cortex was assessed. Fractured extremity was placed in a boot with hip in 20-30 degrees of flexion. Any adjustments required for improving reduction were made by increasing or decreasing traction or altering abduction/adduction and internal/external rotation. Thorough evaluation of images was done to avoid the common malalignments: varus deformity, posterior sag and excessive internal rotation [5-7]. Varus deformity when present was corrected by abducting the limb. Posterior sagging of the distal fragment which was the sagittal plane deformity was corrected by applying anterior force to the posterior distal fragment before completing the reduction with traction and internal rotation [3,4].
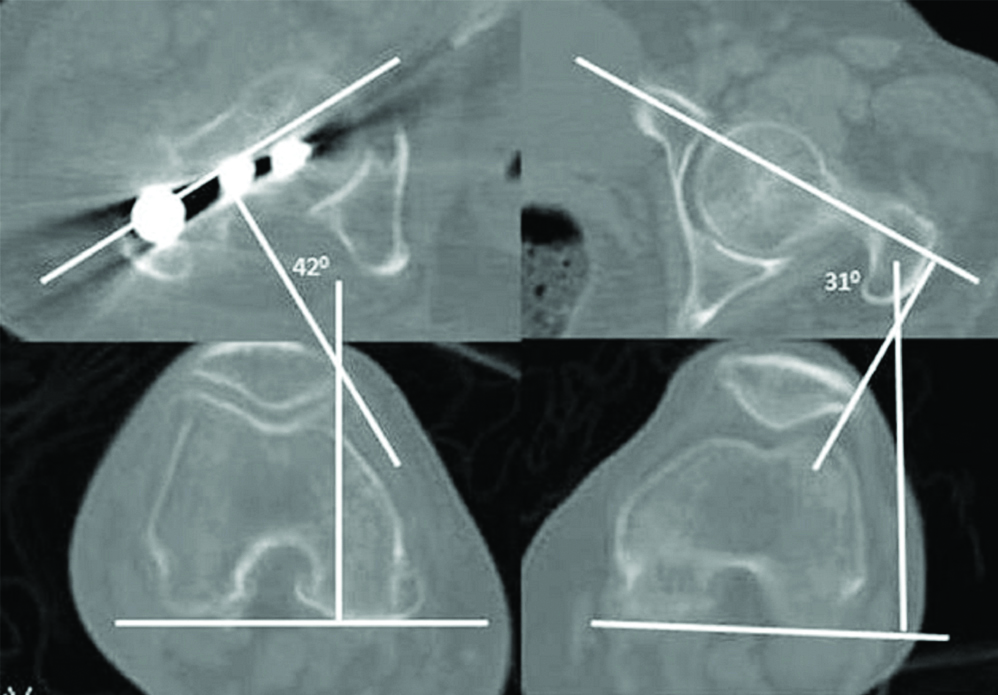
Closed reduction was done in all cases and long proximal femoral nail of same manufacturer with two proximal locking screws in the femoral head was used for fixation in all cases. Procedure was performed by the same team. Steps of surgery followed were as per established standard described method. Patient was mobilised on the day after surgery with quadriceps exercises and weight bearing as tolerable. Once the patient was pain-free and comfortable postoperative CT of pelvis and knee joint was done and compared for rotational alignment against the normal opposite side. CT is considered highly accurate method with good reliability and position of the patient does not influence its accuracy. Measurement was done by technique described by Jeanmart L et al., by determining the angle between the line tangential to femoral condyles and a line drawn through the axis of femoral neck [5]. Malrotation is described as difference in angle between operated and normal side. Internal rotation is identified by increase in anteversion and decrease in anteversion of the femoral neck of the fractured side implies increased external rotation. In the present study, an average of three readings was taken in all cases.
Compliance with Ethical Standards
Ethical standards: Ethical clearance for the study was obtained from the Institutional Ethics Committee and study was conducted according to the Declaration of Helsinki.
Informed consent: All patients have given their informed consent for participation in this study.
Statistical Analysis
Statistical analysis was done by Student’s t-test and chi-square test. SPSS (version 22.0) was used for the statistical calculations. Statistical significance was determined at p<0.05.
The rotational difference of <10° compared to the normal side it was considered as Grade I (variations of normal), between 10° and 14° was considered as Grade II and torsional difference >15° as Grade III [Table/Fig-1] [8].
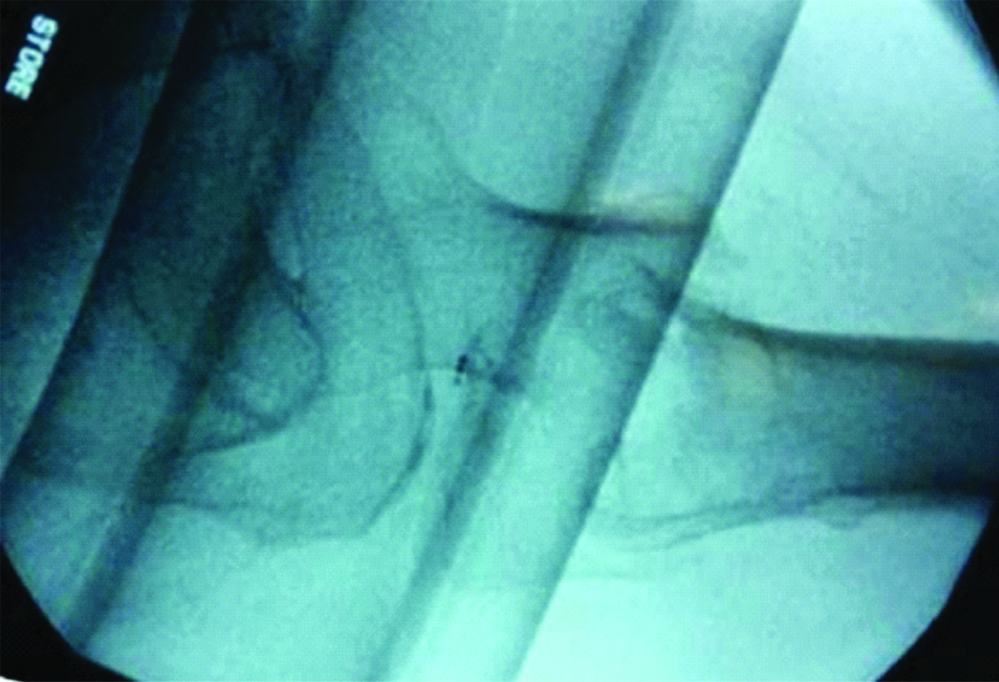
Postoperative assessment of rotational malalignment using CT images as described by Jeanmart L et al. On operated side there is an increase in rotation of 11° (42°,31°). This suggests internal rotational malalignment of 11°.
Results
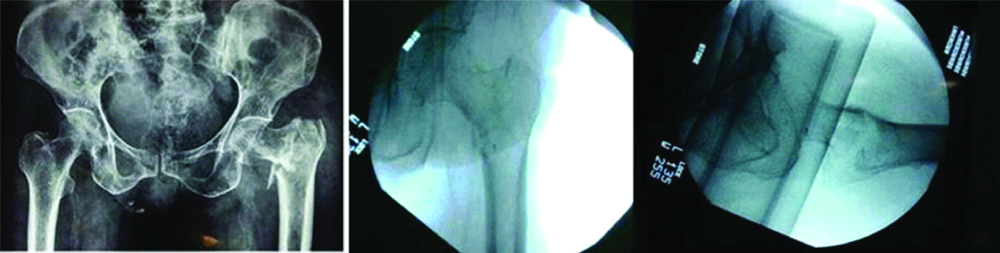
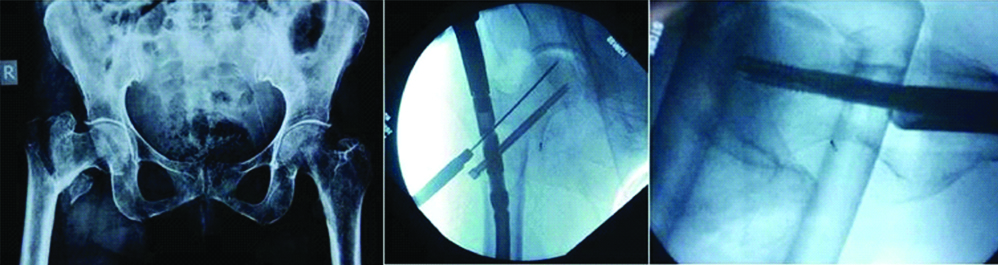
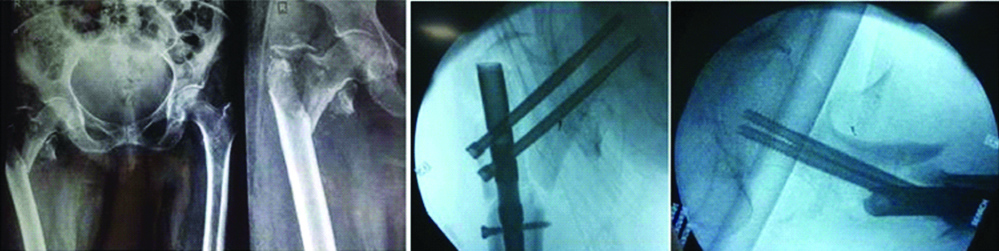
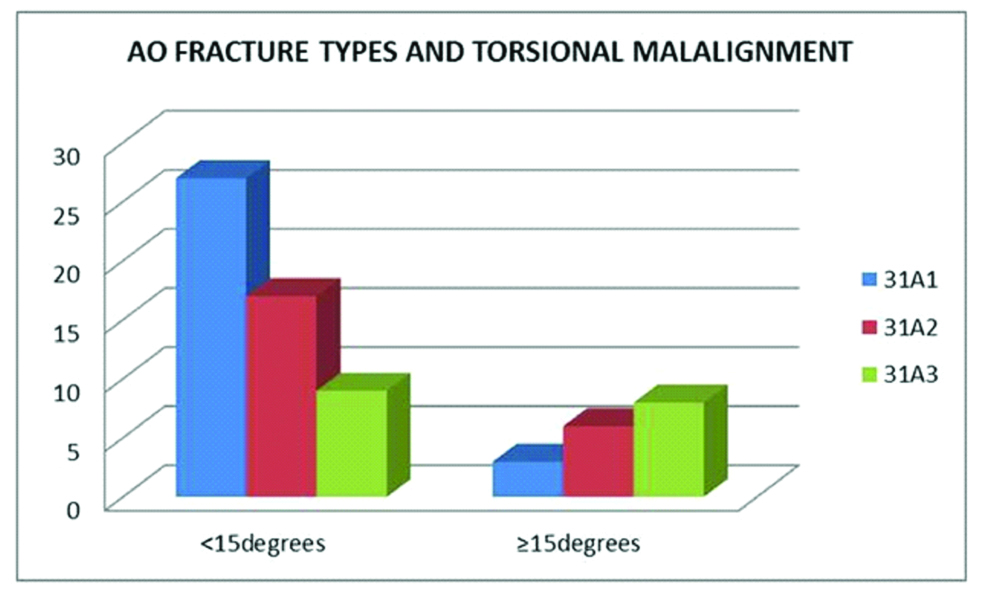
A total number of patients included was 70. Mean age of the patients was 67.22. Out of 70 patients, 42 were males and 28 females. Fracture was caused by fall in 58 cases (82.8%) and trauma in 12 cases (17.2%). Fracture was left sided in 41 cases and right sided in 29 cases. The AO/ASIF classification was used for the fracture classification. The mean anteversion on the normal side was 13.2±9.39°. The mean anteversion on the fixation side was 15.7±8.04°. The mean rotational malalignment was 9.72±5.78°. There was internal rotational deformity in 41 cases (58.6%) with a mean of 10.4±6.21° and external rotational deformity in 29 cases (41.4%) with a mean of 8.8±5.2°. Grade III malrotation was seen in 17 cases (24.3%). There were seven cases with age less than 50 years, two had malalignment of >15° and in both cases, fracture type was 31A3 [Table/Fig-2a,b,c,3,4 and 5].
Preoperative and intraoperative C-arm images of different grades of rotational malalignment in postoperative CT images; Grade I (<100).
Distribution of cases in different grades.
| Grade | Total | Internal rotation | External rotation |
|---|
| Grade I (<100) | 33 (47.1%) | 19 | 14 |
| Grade II (100-140) | 20 (28.6%) | 11 | 9 |
| Grade III (≥150) | 17 (24.3%) | 11 | 6 |
| Total | 70 | 41 (58.8%) | 29 (41.4%) |
Fracture types and postoperative malrotation.
Variables affecting postoperative torsional alignment.
| Variables | <15 Degrees | ≥15 Degrees | Odds Ratio (95%CI) | p-value |
|---|
| Age | 66.56±11.92 | 69.32±10.29 | 0.943 (0.3441 to 2.965) | 0.8370 |
| Sex: Male(Female) | 33 (20) | 9 (8) | 1.4667 (0.4870 to 4.4172) | 0.4960 |
| Side: Left/Right | 31/22 | 10/7 | 2.5564 (0.8364 to 7.8131) | 0.0996 |
| Mode of Injury Fall/RTA | 43/10 | 15/2 | 0.5773 (0.1126 to 2.9204) | 0.5030 |
| Fracture Type 31A1/31A2+31A3 | 27/26 | 3/14 | 4.8462 (1.2459 to 18.8494) | 0.0228 |
| Injury Surgery Interval (Days) | 3.86±2.47 | 5.11±3.01 | 2.6727 (0.8278 to 8.6290) | 0.1002 |
p<0.05
Discussion
Rotational malalignment can be measured by physical examination, radiography, ultrasonography and CT. Measurements of anteversion routinely by CT are considered highly accurate. A precise line should be drawn in the centre of femoral neck on a CT image which often is the reason for inaccurate measurement. This can be done by CT images with multiple slices and superimposition of slices and precisely drawing the line along the middle of the femoral neck. The accuracy can also be improved by taking the average of more measurements [3]. High incidence of rotational malalignment has been reported after intramedullary fixation of femur shaft fractures in CT studies. Significant malrotation of ≥15° has been reported as between 20 to 30% [9].
Ramanoudjame M et al., have reported torsional malalignment postoperatively to be as high as 40% and there was no difference between different types of osteosynthesis [10]. Kim TY et al., in their study found postoperative torsional deformity in 25.7% after internal fixation of intertrochanteric fractures and identified unstable fractures and a delayed operative time as the major factors. They suggested that unstable fractures when reduced with too much of internal rotation of distal fragment, caused malalignment [7]. In the present study when two-part fractures (31A1) were compared with fractures with communication (31A2 and 31A3) p-value was found to be statistically significant [Table/Fig-6].
Comparison of postoperative torsional deformity with other studies.
| Study | Total No. of Cases | Grade III | Internal Rotation | External Rotation |
|---|
| Ramanoudjame M et al., [10] | 40 | 16 (40%) | 14 (35%) | 2 (5%) |
| Kim TY et al., [7] | 109 | 28 (25.7%) | 19 (17.4%) | 9 (8.3%) |
| Present study | 70 | 17 (24.3%) | 11 (15.7%) | 6 (8.6%) |
Based on the present results, there is a need to achieve adequate intraoperative reduction and prevention of this complication. Authors were of the consensus that methods which can assess in anteversion accurately intraoperatively should solve this problem. Techniques have been described for clinical and radiological evaluation of rotational alignment during operation. In ‘hip rotation test’, the rotation of hip is compared with that of contralateral side. The cortices of the proximal and distal fragments appear to have different thickness in case of torsional deformity, described as ‘diameter difference sign’. In ‘lesser trochanter shape sign’, the size of the lesser trochanter of the injured side is compared with the normal side. The amount of lesser trochanter visible intraoperatively in C-arm posterior-anterior image can be used to estimate rotation [9,11]. It shows a small area of the lesser trochanter in internal rotation and a larger area in external rotation of the proximal part of the femur. This knowledge helps to obtain the neutral position of the proximal fragment of the fracture during surgery. Reproducing the profile of the lesser trochanter of the unaffected side increases the accuracy of reduction. This can be done easily in femoral shaft fractures but in many cases of trochanteric fractures lesser trochanter fracture is present which fails this method. In stable fractures, this can be used but in unstable fractures as in intertrochanteric fracture with subtrochanteric extension, four-part fractures, large posteromedial fragments and reverse oblique type fractures this method cannot be used. Tornetta P 3rd et al., used two C-arm images, first true lateral image of the femoral neck is obtained and the second image taken with the posterior condyles aligned. Angle of anteversion can be calculated by the difference in inclination of the position of the C-arm. Postoperative CT examination, recorded only 5° (0 to 8) of malalignment [12]. In trochanteric fractures posterior sag of shaft is seen in many cases in lateral view of images obtained which makes this method difficult. Besides, this method does not measure anteversion of normal side [Table/Fig-7].
Posterior sagging of distal fragment.
Recent advances in computer navigated systems allow a precise reduction of fractures. These are not regularly used in trauma surgeries because of their complexity, the high expense and increased surgical time [13]. Wilharm A et al., in their study on femoral shaft fractures reported a setting up time for the system average 33±11.5 minutes and additional fluoroscopy time of 36±22 seconds was needed to obtain reference X-rays and to verify pin placement [13]. The differences between anteversion assessed intraoperatively by the navigation system and torsional assessment with a postoperative CT were on average 5.4±3.5°. There are no studies with this system in intertrochanteric fractures.
Long-term clinical consequences of rotational deformities after trochanteric fixation are not known. Kim TY et al., in their study recorded VAS scores, functional consequences and recorded complication rates of 10.7% in malalignment group and 14.8% in control group. Authors did not observe any statistically significant difference between the groups in clinical outcomes at the end of 1 year [7].
The clinical and functional follow-up should have been correlated with torsional malalignment. Many studies are available for diaphyseal fractures but trochanteric fractures are different from diaphyseal fractures. The mean age, bone quality, mechanism of injuries and comorbidities differ in both groups. The demographic variables and functional expectations vary in these cases. Torsional malalignment may not significantly affect the clinical results in internal fixation of trochanteric fractures. When deformities are less than 150 patients have fewer complaints and less functional limitations [3,7,8].
Rotational deformities are compensated well and tolerated by patients rarely requiring any intervention. Persisting pain in hip and knee with restriction of movements may cause functional impairment [8]. Degenerative arthritis of knee and hip are noted long-term complications with rotational deformities [14] which also indicates that torsional deformity may aggravate pre-existing degenerative joint diseases in age group where trochanteric fractures are common. Further studies are required to confirm this issue. In young patients, deformities may require surgical correction for those involved in demanding activities such as labour and sports persons. Grade of malrotation determines clinical outcomes. Patients with increased postoperative external rotation perform poorly compared to those with internal rotational deformity, who compensate well and have fewer symptoms. This can be explained by increased retroversion of femoral neck when patient compensates for external rotation [3,10,12].
Limitation
The main limitation of the present study is, the functional consequences of malrotation has not been assessed.
Conclusion
Intertrochanteric fractures managed with intramedullary fixation have rotational malalignment postoperatively frequently present and was seen in 24.3% cases. This needs better intraoperative assessment and has to be corrected intraoperatively by improving assessment methods.
p<0.05
[1]. Haidukewych JG, Intertrochanteric fractures: ten tips to improve resultsJ Bone Joint Surg Am 2009 91:712-9. [Google Scholar]
[2]. Evaniew N, Bhandari M, Cochrane in CORR: Intramedullary nails for extracapsular hip fractures in adults (review)Clin Orthop Relat Res 2015 473:767-74.10.1007/s11999-014-4123-725560962 [Google Scholar] [CrossRef] [PubMed]
[3]. Jaarsma RL, van Kampen A, Rotational malalignment after fractures of the femurJ Bone Joint Surg Br 2004 86(8):1100-04.10.1302/0301-620X.86B8.15663 [Google Scholar] [CrossRef]
[4]. Riehl J, Widmaier J, Techniques of obtaining and maintaining reduction during nailing of femur fracturesOrthopedics 2009 (8):58110.3928/01477447-20090624-1719681545 [Google Scholar] [CrossRef] [PubMed]
[5]. Jeanmart L, Baert AL, Wackenheim A, Computer tomography of neck, chest, spine and limbs: atlas of pathologic computer tomography 1983 Vol. 3Berlin etcSpringer-Verlag:171-77.10.1007/978-3-642-68538-5 [Google Scholar] [CrossRef]
[6]. Weinlein JC, Fractures and dislocations of the hip. In: Canale ST, Beaty JH (eds)Campbell’s operative Orthopaedics 2013 12th editionMosbyPenslyvania:2737-48. [Google Scholar]
[7]. Kim TY, Lee YB, Chang JD, Lee SS, Yoo JH, Chung KJ, Torsional vmalalignment, how much significant in the trochanteric fractures?Injury 2015 46(11):2196-200.10.1016/j.injury.2015.07.01526303999 [Google Scholar] [CrossRef] [PubMed]
[8]. Braten M, Terjesen T, Rossvoll I, Torsional deformity after intramedullary nailing of femoral shaft fractures. Measurement of anteversion angles in 110 patientsJ Bone Joint Surg Br 1993 75:799-803.10.1302/0301-620X.75B5.83764448376444 [Google Scholar] [CrossRef] [PubMed]
[9]. Liodakis E, Kenawey M, Petri M, Zümrüt A, Hawi N, Krettek C, Factors influencing neck anteversion during femoral nailing: A retrospective analysis of 220 torsion-difference CTsInjury 2011 42(11):1342-45.10.1016/j.injury.2011.06.00421704996 [Google Scholar] [CrossRef] [PubMed]
[10]. Ramanoudjame M, Guillon P, Dauzac C, Meunier C, Carcopino JM, CT evaluation of torsional malalignment after intertrochanteric fracture fixationOrthopaedics & Traumatology: Surgery & Research 2010 96:844-48.10.1016/j.otsr.2010.05.00720822963 [Google Scholar] [CrossRef] [PubMed]
[11]. Krettek C, Miclau T, Grun O, Schandelmaier P, Tscherne H, Intraoperative control of axes, rotation and length in femoral and tibial fractures. Technical noteInjury 1998 29(Suppl. 3):C29-39.10.1016/S0020-1383(98)95006-9 [Google Scholar] [CrossRef]
[12]. Tornetta P 3rd, Ritz G, Kantor A, Femoral torsion after interlocked nailing of unstable femoral fracturesJ Trauma 1995 38:213-19.10.1097/00005373-199502000-000117869438 [Google Scholar] [CrossRef] [PubMed]
[13]. Wilharm A, Gras F, Rausch S, Linder R, Marintschev I, Hofmann GO, Navigation in femoral-shaft fractures-from lab tests to clinical routineInjury 2011 42(11):1346-52.10.1016/j.injury.2011.06.02321724185 [Google Scholar] [CrossRef] [PubMed]
[14]. Tönnis D, Heinecke A, Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritisJ Pediatr Orthop 1991 11:419-31.10.1097/01241398-199107000-000011860937 [Google Scholar] [CrossRef] [PubMed]