In the management of large radicular cysts, especially on an aesthetic region, it is essential to obtain information by means of three-dimensional images. They provide proper definition of the extension and of the relationship with important anatomical structures. This case report aims to describe the role of the Cone Beam Computed Tomography (CBCT) on diagnosis, endodontic approach, surgical treatment, as well as follow-up of a large radicular cyst. The patient came to the Dental Clinic of the State University of Maringá, showing asymptomatic enlargement in the anterior maxilla. Tooth 11 was non-vital. CBCT presented a cystic lesion, measuring about 20.69×17.18×16.75 mm, in the periapical region of 11, with involvement of the left nasal fossa floor and incisive canal. Based on clinic and tomographic examinations, the provisional diagnosis was radicular cyst. The treatment plan consisted of endodontic treatment of 11 and enucleation of the lesion, under local anaesthesia. Histopathological examination confirmed the diagnosis. The patient was followed-up clinically and radiographically for two years. We concluded that CBCT contributed a lot to the success of this case, as an important tool for proper diagnosis, surgery, endodontic treatment, as well as follow-up.
Case Report
A 38-year-old male presented to the Dental Clinic of the State University of Maringá, with a chief complaint of volume enlargement in the front teeth for more than three months. According to the patient’s history, a trauma has occurred two years earlier and was the cause of two teeth loss (21 and 22) in this area. One year after this trauma, a swelling appeared and progressed, accompanied by pain, about whose features the patient was unable to give details. At the time he looked for dental assistance, there was no more pain, but the swelling was still present in the maxillary left side. The patient brought the panoramic radiograph required by another professional [Table/Fig-1]. The panoramic radiograph showed radiolucent lesion in the anterior maxilla.
Panoramic radiograph showing radiolucent lesion in the maxilla.

Intraoral clinical examination revealed a significant enlargement, covered by normal mucosa, located over labial vestibular side of maxillary anterior region, in association with 11 and 23, and also a cantilever fixed partial denture with abutment on 11 [Table/Fig-2]. The involved teeth were not responsive to percussion. There were no discolored teeth around. Palpation showed the enlargement was hard in consistency and free of pain or heat. There was no nasal discharge as well. Negative and positive responses were obtained through cold test in 11 and 23, respectively.
a) Full-face photography; b) intraoral photography showing enlargement in the left maxillary region.

Based on history, radiographic and clinical findings, a provisional diagnosis of radicular cyst associated to 11 was given. The patient was then submitted to CBCT for further exploration, and to check for proximity or any involvement with important structures. CBCT showed a hypodense image in the periapical region of 11, measuring about 20.69×17.18×16.75 mm, with regular limits, disruption of vestibular cortical bone, involvement of incisive canal and left nasal floor, but without any membrane thickening [Table/Fig-3].
Initial CBCT: 3D reconstruction to illustrate the involvement of the lesion in the anterior region of maxilla (a); extension of the lesion and close contact with the apex 11 (d); the dimension, and disruption of the vestibular cortical bone (red arrow-b,c); involvement left nasal floor without any membrane thickening within the left nasal cavity (white arrow-b,f); involvement incisive canal (yellow arrow-c,e,f).

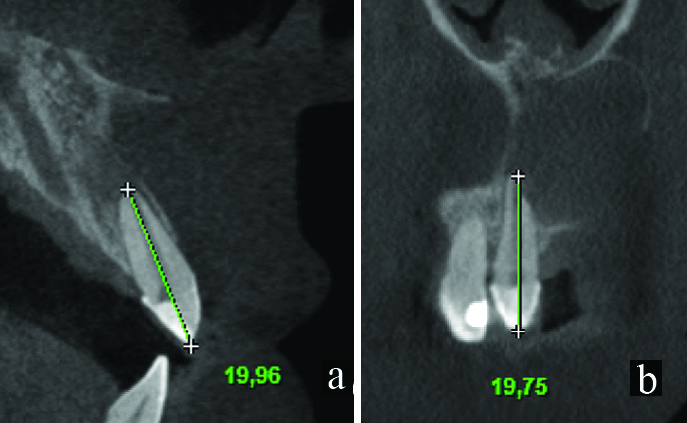
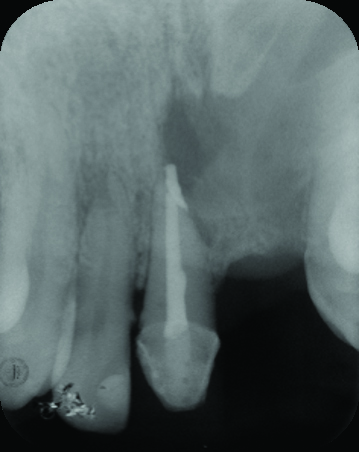
According to the patient’s needs and conditions, a treatment plan was elaborated and explained to him. Consent was obtained by taking signature of the patient. In the endodontic treatment of 11, the working length was determined by measuring on CBCT scan, in association with clinical measurements using electronic apex locator [Table/Fig-4]. The root canal was prepared with crown down technique by size 15-60 K-files, followed by gentle irrigation with sodium hypochlorite (2.5% NaOCl) and normal saline, under rubber dam isolation. No purulent exudate was found from the canal of the tooth. Calcium hydroxide intracanal medicament was used for one week. The obturation was completed by using customised Roll cone technique [Table/Fig-5].
CBCT sections showing the apical involvement of teeth 11 by the cystic lesion and the root canal length measured in the vestibular-lingual (sagital plane-a) and the mesiodistal (coronal plane-b) slices.
Final periapical radiograph of endodontic treatment.
Difficulty for patient to perform routine examination, risks of pathological fracture or of even more tissues damages, associated with cystic growth, were all considered. Marsupialisation, followed by complete enucleation, was presented to the patient as treatment choice, but he refused two-steps approach. Then, enucleation was performed as follows: intraoral antisepsis with 0.12% chlorhexidine digluconate solution; extraoral antisepsis with topical 10% povidone iodine; and infiltrative anaesthesia with 2% pivacaine with epinephrine 1:100,000. Mucoperiosteal flap of Neumann was performed involving 12, 11 and 23, using a 15 scalpel blade and periosteal dissector, exposing the large bone defect with the lesion. Cystic enucleation was performed with surgical curette, followed by apicoplasty of 11, and 3-0 silk flap closure [Table/Fig-6].
Neumann incision on the buccal mucosa (a), surgical specimen (b), surgical cavity after enucleation of the cystic lesion (c), sutures of the flap (d).

Prescribed medication consisted of a widely used Brazilian protocol [1,2] for postoperative pain control: 500 mg dipyrone, every six hours, for two days, in addition to mouthwash with 0.12% chlorhexidine gluconate, every 12 hours, for seven days.
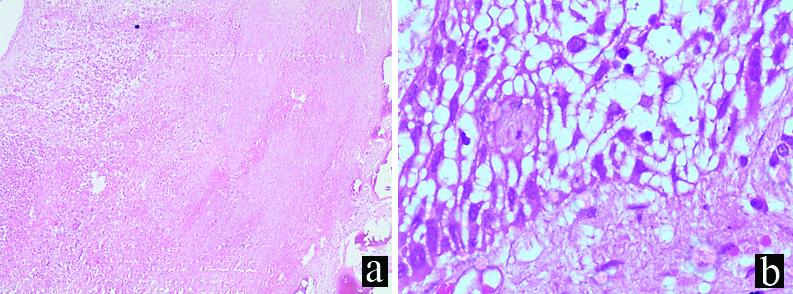
The specimen was sent to histopathological examination, confirmed the provisional diagnosis of a radicular cyst. It showed fragments of cystic capsule, recovered by stratified squamous epithelium, exhibiting mononuclear inflammatory infiltration and intra/intercellular oedema. The underlying connective tissue was chronically inflamed, with areas of haemorrhage [Table/Fig-7].
Photomicrography showing chronically inflamed cystic capsule with areas of haemorrhage (10X magnification-a), and stratified squamous epithelium with prominent inter and intracellular oedema (40X magnification-b).
The patient was followed-up by means of clinic and imaginologic examinations. A two-year postoperative CBCT was taken and prosthetic rehabilitation of the affected area was performed [Table/Fig-8]. It was possible to verify the regression of the lesion, since there is no longer interruption of the nasal fossa floor or cortical incisive canal; as well as a change from highly hypodense image to a new density one, compatible with soft tissue, suggesting fibrous scar.
Postoperative CBCT 3D reconstruction (a); CBCT images showing the lesion significant regression (b-d); hypodense residual area close to the 11 apex (e); continuity of the nasal fossa floor and the cortical incisive canal (e,f).

Discussion
Radicular cyst is the most common odontogenic cystic lesion of inflammatory origin. The frequency, on the permanent dentition, is about 7 to 54% [3]. These cysts occur associated to the apices of teeth with infected and necrotic pulps, usually as a consequence of trauma or dental caries progression [4]. Malassez epithelial rests are the source of radicular cysts lining. The responsible for these cysts’ growths, however, is a combination of several factors involving epithelial-stromal interaction [5]. Large radicular cysts are rare, probably because of their slow growth. They can also be avoided by simple approach of carious lesions or can be solved by endodontic treatment. When they reach large dimensions, they can lead to extensive erosion of adjacent bony structures [6], as occured in our case.
The initial approach must be the endodontic treatment of necrotic tooth [7,8]. According to previous study, 73.8% of cyst like periapical lesions healed after nonsurgical root canal treatment [9], with proper chemical-mechanical cleaning and infection control in the root. However, depending on the clinic and radiographic features and on the size of the lesion, the surgical treatment is also necessary [4,6,10]. Among the main methods of surgical approach of cysts, four modalities can be listed: enucleation, marsupialisation and decompression, as well as combination of marsupialisation or decompression and enucleation, and enucleation with curettage [11,12]. Marsupialisation and decompression are conservative interventions for large cysts, because they minimise the risk of damage to tissues [1,11]. These techniques have disadvantages, as the fact that the patient should proceed regular draining and cleaning of the cavity. Besides this, the pathologic tissue is left in situ and a second surgical procedure is generally required to remove the residual lesion [1]. The choice, in most cases, is enucleation, because the entire cyst is removed and complete pathological examination is undertaken, without postoperative discomfort for patients, since there is no need for irrigation or the risk of occlusion of the stent by detritus [11,12]. Accordingly, Diwan A et al., and Dikicier E et al., also presented cases that support the opinion that careful enucleation of large cysts can be done with success, without complications [6,11].
Large cysts, especially in the anterior maxilla, require long-term follow-up because complete reossification of the surgical area, in general, takes two years [13]. On conventional radiography, important anatomical sites of anterior maxilla are visualised with overlapping of adjacent tissues, including bony structures. The multiplanar 3D, axial, sagittal and coronal plane CBCT scans provide a high diagnostic capability for detection of all types of morphological changes, as well as complete visualisation of the healing area [8]. In our case, it was extremely important, since preoperative CBCT shows involvement of the adjacent necrotic tooth (11) and its length, extent of the hypodense lesion, as well as relationship with incisive canal and nasal fossa floor (without membrane thickening). These images, besides providing subsidies for surgery planning and endodontic treatment better than any conventional radiography, also contributed to the understanding of histopathological presentation of a radicular cyst, that although the size, maintains its features and can be differentiated from other entities.
In addition, CBCT has been shown to provide high dimensional accuracy, without bias, because the CBCT images are isotropic and the reconstructed slices are geometrically accurate [14]. In the Liang YH et al., study, there was no difference among measurements done on CBCT images and in the actual physical lesions performed in human mandibles [15]. Furthermore, CBCT software may be used to maximise the diagnostic yield of the captured data [14]. Villoria EM et al., reported two cases in which CBCT was used to evaluate periapical lesions following endodontic treatment. It could confirm lesion regression by volumetric analysis [8]. In our case, comparing measurements obtained on CBCT, preoperative and postoperatively, it was possible to see significant regression. Then, with the contribution of CBCT, before and after clinical approach, we were able to manage successfully this challenger case. Bone tissue regenerated in the nasal floor, incisive canal and periapical region of 11. The patient remains asymptomatic, after two years.
Conclusion
Multidisciplinary approach involving endodontics and surgery is necessary in cases of large radicular cysts. The CBCT turned out to be an important tool to improve diagnosis, endodontic treatment quality, surgical procedures planning and accuracy, as well as wound healing during follow-up period, especially in large cystic lesions in anterior maxilla, where there are aesthetic demand and important structures.
[1]. Endo MS, Eidt JMS, Danieletto CF, Iwaki Filho L, Pavan NNO, Management of radicular cyst: endodontic retreatment associated to marsupialization and enucleationDent Press Endod 2016 6(3):18-25.10.14436/2358-2545.6.3.018-025.oar [Google Scholar] [CrossRef]
[2]. Moore RA, Wiffen PJ, Derry S, Maguire T, Roy YM, Tyrrell L, Non-prescription (OTC) oral analgesics for acute pain-an overview of Cochrane reviewsCochrane database Syst Rev [Internet] 2015 (11):CD010794Available from: http://www.ncbi.nlm.nih.gov/pubmed/2654467510.1002/14651858.CD010794.pub2PMC6485506 [Google Scholar] [CrossRef] [PubMed]
[3]. Mahesh BS, P Shastry S, S Murthy P, Jyotsna TR, Role of cone beam computed tomography in evaluation of radicular cyst mimicking dentigerous cyst in a 7-year-old child: a case report and literature reviewInt J Clin Pediatr Dent 2017 10(2):213-16.10.5005/jp-journals-10005-143828890627 [Google Scholar] [CrossRef] [PubMed]
[4]. Kadam NS, Ataide IDN De, Raghava P, Fernandes M, Hede R, Management of large radicular cyst by conservative surgical approach: a case reportJ Clin Diagn Res 2014 8(2):239-41.10.7860/JCDR/2014/5763.406924701544 [Google Scholar] [CrossRef] [PubMed]
[5]. Bernardi L, Visioli F, Nör C, Rados PV, Radicular cyst: an update of the biological factors related to lining epitheliumJ Endod 2015 41(12):1951-61.10.1016/j.joen.2015.08.03626603778 [Google Scholar] [CrossRef] [PubMed]
[6]. Diwan A, Bhagavaldas MC, Bagga V, Shetty A, Multidisciplinary approach in management of a large cystic lesion in anterior maxilla-a case reportJ Clin Diagn Res [Internet] 2015 9(5):ZD41-43.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2615558910.7860/JCDR/2015/13540.599226155589 [Google Scholar] [CrossRef] [PubMed]
[7]. Ghorbanzadeh S, Ashraf H, Hosseinpour S, Ghorbanzadeh F, Nonsurgical management of a large periapical lesion: a case reportIran Endod J 2017 12(2):253-56. [Google Scholar]
[8]. Villoria EM, Lenzi AR, Soares RV, Souki BQ, Sigurdsson A, Marques AP, Post-processing open-source software for the CBCT monitoring of periapical lesions healing following endodontic treatment: Technical report of two casesDentomaxillofacial Radiol 2016 46(1):2016029310.1259/dmfr.2016029327936918 [Google Scholar] [CrossRef] [PubMed]
[9]. Calişkan MK, Prognosis of large cyst-like periapical lesions following nonsurgical root canal treatment: a clinical reviewInt Endod J 2004 37(6):408-16.10.1111/j.1365-2591.2004.00809.x15186249 [Google Scholar] [CrossRef] [PubMed]
[10]. Dicker GJ, Tuijt M, Koolstra JH, Van Schijndel RA, Castelijns JA, Tuinzing DB, Static and dynamic loading of mandibular condyles and their positional changes after bilateral sagittal split advancement osteotomiesInt J Oral Maxillofac Surg. International Association of Oral and Maxillofacial Surgery 2012 41(9):1131-36.10.1016/j.ijom.2012.03.01322525894 [Google Scholar] [CrossRef] [PubMed]
[11]. Dikicier E, Dikicier S, Karacayli U, Surgical approach for a large maxillary radicular cyst: a case reportInt J Oral Maxillofac Surg [Internet]. International Association of Oral and Maxillofacial Surgery 2015 44:e203Available from: http://linkinghub.elsevier.com/retrieve/pii/S090150271500356210.1016/j.ijom.2015.08.065 [Google Scholar] [CrossRef]
[12]. Yaman Z, Suer BT, Clinical comparison of ultrasonic surgery and conventional surgical techniques for enucleating jaw cystsInt J Oral Maxillofac Surg. International Association of Oral and Maxillofacial Surgery 2013 42(11):1462-68.10.1016/j.ijom.2013.05.00323769149 [Google Scholar] [CrossRef] [PubMed]
[13]. Martin SA, Conventional endodontic therapy of upper central incisor combined with cyst decompression: a case reportJ Endod 2007 33(6):753-57.10.1016/j.joen.2007.01.01317509421 [Google Scholar] [CrossRef] [PubMed]
[14]. Venskutonis T, Plotino G, Juodzbalys G, Mickevičienė L, The importance of cone-beam computed tomography in the management of endodontic problems: a review of the literatureJ Endod 2014 40(12):1895-901.10.1016/j.joen.2014.05.00925287321 [Google Scholar] [CrossRef] [PubMed]
[15]. Liang YH, Jiang L, Gao XJ, Shemesh H, Wesselink PR, Wu MK, Detection and measurement of artificial periapical lesions by cone-beam computed tomographyInt Endod J 2014 47(4):332-38.10.1111/iej.1214823815501 [Google Scholar] [CrossRef] [PubMed]