Tonsillectomy techniques include cold steel methods and hot methods. Commonly used methods are dissection and snare tonsillectomy, Coblation tonsillectomy, Cryosurgery and laser tonsillectomy. Despite newer techniques, the cold steel technique has remained the standard surgical technique for years [1]. It allows maximum preservation and less mechanical injury to oropharyngeal mucosa [2]. Laser tonsillectomy provides a maximum protection to the peritonsillar tissue and bleeding events gets significantly lowered [3]. Its characteristic tissue cutting and tissue ablation helps the patients in experiencing shorter recovery time [4]. Since laser tonsillectomy provides bloodless operative field, it can be used for patients with a bleeding diathesis. But thermal injury to mucosa delays healing, increases postoperative pain and bleeding [5]. The risk of transmission of infected particles like HIV or Hepatitis is less since laser technique is a no touch technique.
Complications of tonsillectomy are classified into immediate, intermediate and late. Among all these, despite various techniques, pain and haemorrhage after tonsillectomy remain the most important.
Since children cannot express the pain until they develop the ability to speak, it becomes necessary to have concrete tools for measuring their pain. To the best of our knowledge there are no studies comparing Laser and conventional tonsillectomy in Southern India. We undertook this study to evaluate and compare operating time, intraoperative blood loss and postoperative pain following tonsillectomy by CO2 LASER and conventional dissection methods. The primary outcome expected from this study was that laser tonsillectomy patients experience less intraoperative time, bleeding and postoperative pain when compared to that of dissection tonsillectomy.
Materials and Methods
This single centre double blinded randomised controlled trial was conducted in a tertiary care hospital in Southern India between August 2014 to August 2016. Ethical clearance was obtained from the Institute Ethics Committee (Human studies) JIP/IEC/2014/8/377, before recruitment of patients into the study. The trial registration number is CTRI/2017/09/009773. Sample size was estimated considering a mean difference in postoperative pain between the groups as 5 with a standard deviation of 10 with 5% level of significance and 95% power [6].
Patients with chronic tonsillitis, children and young adults of age group 7-18 years fulfilling Scottish Intercollegiate Guidelines Network criteria were included in the study. We excluded patients with suspected malignancy, patients aged >18 years and with bleeding disorders. Informed consent was obtained from the parents of all the participants. Simple random sampling was used. A total of 126 patients were recruited into our study. Randomisation was done by block randomisation sequence generated by computer with a fixed block size of ten into two groups (ratio 1:1) by an investigator with no involvement in the trial and allocation concealment was done by sequentially numbered opaque sealed envelopes.
Enrolment into the study was done by the outpatient department doctors and the group allocation was concealed from the principal investigator and the envelopes were opened only after the enrolled patients completed the baseline assessment and were ready for the procedure. In this study, patients were blinded with regards to the technique used. All the surgeries were done under general anaesthesia with oro-tracheal intubation after proper pre-medications. All surgeries were done by the same surgeon to avoid bias. The primary variable was operative time. The secondary variables were intraoperative bleeding and postoperative pain.
LASER tonsillectomy was performed by using LUMENIS CO2 LASER with all necessary precautions. The power was set between 10 to 15 watts and in continuous mode. Laser was used to separate the tonsil tissue from tonsillar bed. Bleeding was controlled using laser only. Dissection method was performed using blunt dissector to separate the tonsil from its bed and snare was used to remove the tissue. Bleeding was controlled using bipolar diathermy or tying knot using cotton suture material.
Surgical time was measured from the insertion of Boyle-Davis mouth gag to the removal of the gag after removal of tonsil tissue from the oral cavity. Intraoperative blood loss was measured by weighing the tonsil swab before and after the tonsillectomy and by measuring the amount of blood in the suction bottle. Cotton balls were weighed before and after the procedure. A 150 mL saline was used uniformly for the whole procedure. Then the saline that was taken in the bowl was sucked into the suction bottle. The suction tube was raised above the level of the suction bottle to ensure that all the fluid was emptied into the suction bottle. The quantity was measured by pouring it into the measuring cylinder. Amount of blood loss was measured by calculating the difference in weight of swabs before and after use and converted into milliliters by dividing the weight by specific gravity, which is 1.055 and then adding the total so obtained (1 gm=1 mL) to the volume of blood collected in the suction bottles. All the cotton balls and packs were kept on a weighing machine for measuring the weight, thereby measuring the amount of blood loss.
Postoperatively, pain scores were charted on day 1 and a week later during follow-up using standardised VAS in which 0 indicates no pain and 10 indicates very severe pain. Assessment of time, blood loss and pain scores were done by para-medical and nursing staffs not associated with the study. Syrup Ibuprofen and Paracetamol thrice a day was the standard pain control regime used in all the patients. Patients were discharged one or two days after the surgery. Patients were reviewed after one week in ENT OPD. Patients who failed to come for follow-up were interviewed through telephone.
Calculations
Weight of cotton balls before use=y g
Weight of the cotton balls soaked in blood=x g
Weight of the blood lost=x-y g
Specific gravity of blood=1.055
Quantity of blood lost=x-y/1.055 g
Amount of fluid (blood+known quantity of saline) collected in suction bottle=z mL
Amount of saline sucked in the bottle=150 mL
Quantity of blood in suction bottle=z-150 mL
Total quantity of blood lost=x-y/1.055 g+z-150 mL
Statistical Analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences (SPSS) software version 19. Continuous Variables like age, haemoglobin, bleeding time, clotting time, Intraoperative Time (IOT) (minutes), Intraoperative Bleeding (IOB) (mL) and Postoperative (POP) Pain score were checked for normal distribution assumption using Kolmogorov-Smirnov test. We found that normal distribution assumption was satisfied for all variables. The continuous variables were expressed as arithmetic mean, standard deviation and qualitative nominal variables like Sex was presented using number with a percentage. We used independent sample t-test to test the difference of means between the two groups with respect to the outcome variables. Levene test was used to check the homogeneity of variances among the two groups. Welch approximation was applied in the absence of homogeneity condition. Statistical analysis was carried out at 5% level of significance and a p-value of <0.05 was considered significant.
Results
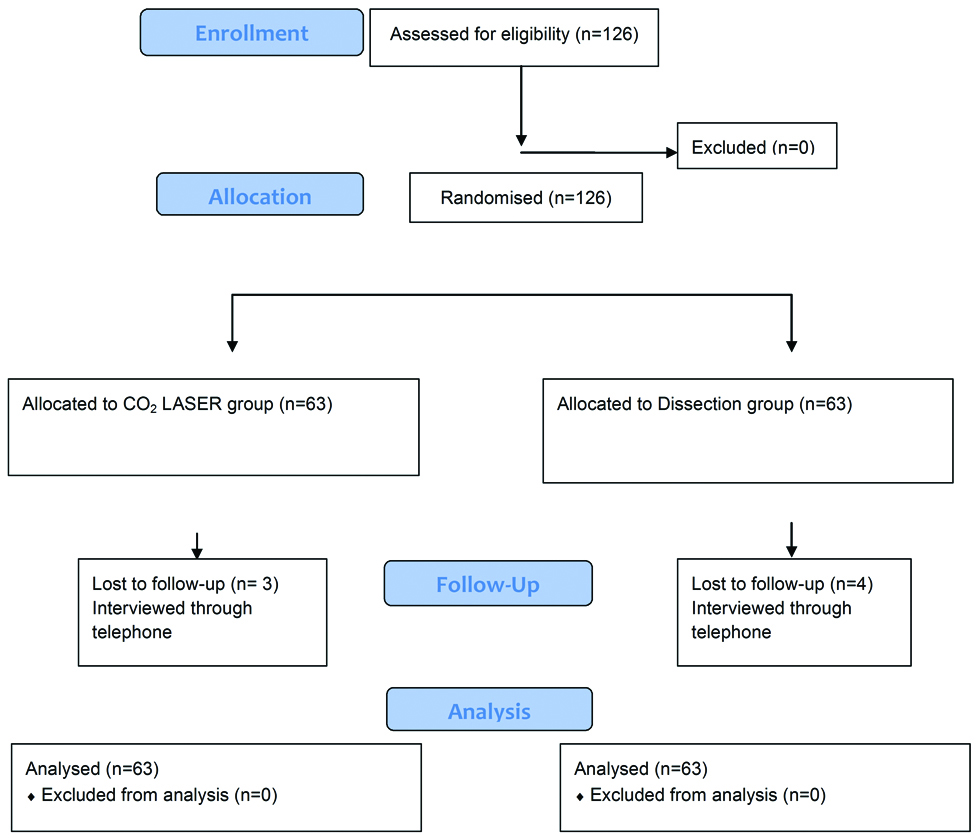
The recruitment for the study commenced from August 2014 and was completed by August 2016 once the requisite numbers of patients were included in the study [Table/Fig-1]. The baseline table was produced by comparing the summary statistics of continuous variables and categorical variables by two groups (CO2 LASER, Dissection) to assess randomisation. We found the two groups were similarly matched with respect to baseline variables.
Participant flow chart in the study.
The mean age was 10.75 years (range 7-18 years) for the CO2 LASER group and 9.89 years (range 7-18 years) for dissection group [Table/Fig-2]. All variables were normally distributed.
The mean operative time was significantly lower for CO2 LASER group. Similarly, the mean intraoperative bleeding for CO2 LASER group was significantly less. There was a statistically significant difference between the scores of the two groups on postoperative day 1 and 7, which was found to be statistically significant [Table/Fig-3].
Demographic and clinical characteristics for each group.
| Demographic data | CO2 Laser group (n=63) Mean (SD) | Dissection group (n=63) Mean (SD) |
|---|
| Age (years) | 10.75 (3.5) | 9.89 (3.1) |
| Haemoglobin (g%) | 12.1 (0.91) | 12.04 (0.92) |
| Bleeding time (minutes) | 2:11 (0:47) | 2:20 (0.41) |
| Clotting time (minutes) | 5:31 (1:16) | 6:32 (1:39) |
| Gender | n (%) | n (%) |
| Males | 26 (41.3) | 30 (47.6) |
| Females | 37 (58.7) | 33 (52.4) |
Comparison of operative time, intraoperative blood loss and postoperative pain score between the two groups.
| Variable | CO2 LASER group (n=63) Mean (SD) | Dissection group (n=63) Mean (SD) | Mean Difference and p-value |
|---|
| Intraoperative time (minutes) | 31.2 (6.64) | 53.9 (12.5) | 22.6p-value: <0.001 |
| Intraoperative bleeding (mL) | 40.8 (9.7) | 80.2 (18.3) | 39.3p-value: <0.001 |
| Postoperative pain on day 1 | 5.52 (1.1) | 4.87 (1.4) | 0.651p-value: 0.007 |
| Postoperative pain on day 7 | 2.65 (0.86) | 2.00 (0.54) | 0.65p-value: <0.001 |
Discussion
The purpose of this study was to compare CO2 LASER tonsillectomy and dissection tonsillectomy in terms of intraoperative time, intraoperative bleeding and postoperative pain on postoperative day 1 and postoperative day 7 using VAS. CO2 LASER tonsillectomy is associated with less intraoperative time, less intraoperative bleeding and comparable postoperative pain. Surgeons should select the technique that offers minimum morbidity in their hands. Ideal tonsillectomy should be quick, painless and associated with minimum blood loss. The characteristic of laser wounds is the absence of postoperative oedema because of its minimal operative trauma combined with vascular seal. Reflection and scattering are negligible with CO2 LASER and so thermal impacts are very minimal. The CO2 LASER used in the oral cavity and oropharynx shows more benefits over conventional technique. Reduced intraoperative time reduces the anaesthetic time and exposure to anaesthetic agents indirectly.
Intraoperative Time
In this study, operating time was noted from the insertion of Boyle-Davis mouth gag till its removal. Thus, the time taken to control the bleeding influenced the duration of surgery and the amount of blood loss. The mean intraoperative time in CO2 LASER group was 31.2 minutes and in dissection group was 53.9 minutes.
In a retrospective study by Jackel MC et al., it was found that LASER tonsillectomy provided a maximum protection for the peri tonsillar tissue and so severe bleeding events were reduced significantly when compared to in conventional group [3].
This study was similar to the study done by Sattar MA et al., prospective study among age group 7-12 years and found that intraoperative time was less in laser when compared to dissection method [7]. Ishlah LW et al., compared intraoperative time, intraoperative bleeding and postoperative pain between conventional and CO2 LASER tonsillectomy among 60 patients in a prospective randomised study and found a statistically significant difference in intraoperative bleeding and time in the LASER group [6]. The results are comparable with our study. But the postoperative pain was not significantly different between the two groups unlike in our study which showed significant postoperative pain in the LASER group.
Contrastingly, Strunk CL et al., found that LASER caused an increase in total intraoperative time because of increased set-up time and costs and in addition found that laser malfunctioning also poses a problem [8]. They did not find statistically significant difference in the level of postoperative pain between LASER and dissection groups. We did not face such problems like malfunctioning of laser during our study.
Intraoperative Blood Loss
It is difficult to measure intraoperative blood loss. Different methods like swab weighing, repeated volume delumination, measuring the weight of the patient, etc. are available. In our study, mean intraoperative blood loss in CO2 LASER tonsillectomy was 40.9 mL and in dissection technique was 80.2 mL.
Ahmed M et al., and Mohammadi G et al., compared dissection and CO2 LASER tonsillectomy and found that intraoperative blood loss and intraoperative time was significantly lesser in CO2 LASER group [9,10]. But postoperative pain was more in conventional group whereas there was no difference between the groups [9,10]. These studies were done retrospectively while ours was done in a prospective manner.
Hossain AT et al., had done a retrospective study among 10 to 35 years and found that intraoperative blood loss was significantly less with CO2 LASER than that of dissection technique (5 mL vs. 18 mL) [11].
Postoperative Pain
Postoperative pain on days 1 and 7 using VAS were almost similar between the groups.
Alharbi FA et al., [12] found that there was no significant difference in postoperative pain between the two techniques similar to Mohammadi G et al., [10].
Auf I et al., conducted a study in which 38 patients underwent Potassium Titanyl Phosphate (KTP) laser tonsillectomy on one side and standard dissection tonsillectomy on other side and found that laser tonsillectomy caused more postoperative pain and less bleeding than dissection technique [13].
Telian SA et al., revealed a clinically significant feature that hot dissection tonsillectomy group took two and half days longer to return to a normal diet [14]. This difference of one day in the time to return to normal diet is of clinical significance. Even though this was not assessed in our study we observed that LASER by virtue of causing more pain resulted in longer recovery time as evidenced by significantly increased postoperative time in postoperative day 7 [Table/Fig-3].
Surprisingly, Kim NG et al., found that the laser tonsillectomy patients experienced less postoperative pain when compared with dissection, coblation and electrocautery tonsillectomy [15].
Rakesh S et al., conducted a study comparing coblation and dissection tonsillectomy and found that dissection tonsillectomy had increased intraoperative bleeding and no significant pain difference on postoperative day 7 [16].
Limitation
Possible limitations in our study are that a single Laser setting was used in all patients. Sub group analysis could have been done in Laser group by comparing different Laser settings with postoperative pain. Secondly, although postoperative pain was managed similarly in each group the differential tissue healing after Laser and conventional methods were not taken into account when assessing pain. Thirdly, cost analysis and quality of life assessment regarding time taken to return to normal diet was not done.
Conclusion
Tonsillectomy with CO2 LASER method is associated with less intraoperative time, less intraoperative bleeding but with more postoperative pain. More studies incorporating sub group analysis in Laser group by comparing different Laser settings with postoperative pain, cost analysis, quality of life assessment after Laser tonsillectomy and studies comparing various Lasers in tonsillectomy have to be done to enforce the view that Laser tonsillectomy is feasible in a low resource setting as an alternative to dissection and snare method.