WHO estimates that seeking prompt and appropriate health care could reduce child deaths by 20% [1]. Among childhood deaths in developing countries around 27% result from Acute Respiratory Infections (ARI) and another 23% from diarrhoea [1]. Various studies from developing countries have reported delay in seeking appropriate care and not seeking any care contributes to large number of child deaths [2-5]. Existing interventions could prevent many deaths among children if they are presented for appropriate and timely care [6]. Health interview surveys appear to offer the best vehicle for analysing care seeking behaviour on representative sample of children. These surveys typically involve single cross-sectional interviews, based on random sample of defined population, in which mothers are asked to report about illnesses experienced and health services or treatment used within specified time period prior to interview. Delay in access to health care involves problem in disease recognition, decision making and availability of health services [7]. Early diagnosis and prompt and appropriate referral serves as backbone of programmes aiming at reduction of under five (U-5) mortality.
Realistic formulation of health policies and programmes requires inputs from HSR, which is scarce in our country. Better understanding of HCSB is needed both in terms of utilisation of different sources of care and expenses on treatment for optimisation of health care delivery.
Socio-economic status is one of the important determinants of HCSB and the ability to spend for treatment of illness. Out-of-pocket-expenditure accounts for largest component of total household health expenditure in the country. Health expenditures, expressed as a fraction of household income, range from 3.95% in the poorest households [8] and this entraps the families into poverty–illness-poverty cycle. Growing reliance on private curative health care even by poorer people indicates inability of the state system to meet health demands of community. This disturbing trend is an indicator of denial of health care for a larger population in future. There is a need to enhance the effective utilisation of existing resources and simultaneously to think of various ways of augmenting such resources.
To assess health seeking behaviour for under five (U-5) childhood illness, perception of danger signs in mothers, study sources of health care sought and expenditure incurred in outpatient care for U-5 in different parental income groups.
Materials and Methods
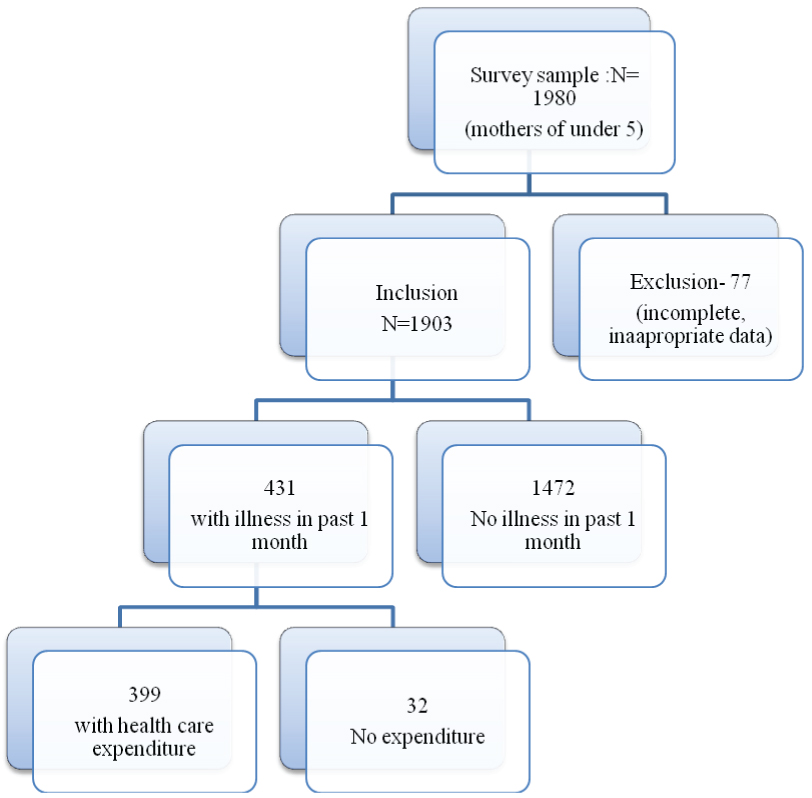
A cross sectional survey was conducted in all five taluks of Dakshina Kannada district with a target sample size of 1980 mothers of U-5 children. Dakshina Kannada is a coastal district of Karnataka with five taluks. The district has an area of 4560 square kilometers, a population density of 416 per sqKm, literacy rate 83.35% and IMR of 10.9 (2015). In the present study, 66 clusters were randomly selected by cluster random sampling method, each cluster was around anganwadi with 30 U-5 Children [Table/Fig-1]. The number of clusters was proportional to number of anganwadis in that taluk. UNICEF multi-indicator survey questionnaire was adopted, modified to local language, pretested and used for the study. A core group of 10 health care workers were trained for fifteen days to administer the questionnaire and to collect the data. Questionnaire contained information about socio-demographic characteristics of family, symptoms, perception of danger signs and illness. Mothers of U-5 children in the region were identified, door to door survey done and invited to participate in the interview. After informed verbal consent and interview necessary information was recorded in questionnaire with the help of health workers. In addition, mothers were also enquired about health care expenditure during illness episodes.
Flow chart of under five mother inclusion in the study.
HCSB was analysed with variables ‘Appropriate care’, ‘Appropriate and prompt care’ and ‘prompt care’ based on type of facility and source from where care was sought and also time interval elapsed from recognition of illness until care was sought.
Outcome variables are as follows:
Appropriate Care: Care sought from qualified medical professionals in Public Health System (PHS) and private hospitals/clinics.
Inappropriate Care: Care such as purchasing medicines from pharmacy, home remedies, visiting pharmacies, temples and traditional healers were defined as inappropriate care.
Prompt Care: Care that was sought within 24 hours from recognition of illness.
Acute Respiratory Infection (ARI): Cough with fever with or without respiratory difficulty
Acute Diarrhoeal Disorder (ADD): Loose or watery stools three or more episodes in a day.
Data Analysis
Data was coded and analysed using the SPSS package (SPSS Inc., Chicago, IL, USA, Version 11.5). Results were expressed as rates and proportions. Outcomes variables were compared with socio-demographic characteristics of families. Factors influencing care seeking behaviour with ‘prompt care & appropriate care’ were identified as dichotomized dependent variables and independent variables as both categorical and continuous variables by using logistic regression. Care seeking behaviour predictors were estimated by calculation of Odds Ratios (OR) and 95% Confidence Intervals (CIs) and a p-value of less than 0.05 was considered significant.
Results
Total of 1903 mothers of U-5 children were recruited in cross sectional study. Among these, 917(48.3%) were Below Poverty line (BPL) card holders out of which 229(24.9%) had a monthly income of less than Rs.1000 and 437(47.6%) had income of more than Rs.3000. 32(12.2%) of people with income less than Rs.1000 did not have BPL card. Health care providers were available within 5 km in 1815(95.4%) of the mothers. It was reported that 1693(89%) breast fed their babies within two hours of birth. Out of 1903 mothers danger signs were perceived as fever in 1797 (94.4%), inability to suck at breast/drink in 1335 (70.2%), rapid breathing in 1542 (81%), loose stools in 1504 (79%) and blood in urine and stools in 1251 (65%).
Out of 1903 surveyed, illness episode was reported in 431 (22.6%) children in past one month. Among them 299 (69.4%) had ARI, 64 (14.8%) had ADD, 15 (3.5%) had infectious diseases and 53 (12.3%) other diseases. A total of 294 (68.2%) children received some care within 24 hours while 113 (26.2%) within 48 hours and 7 (1.6%) after three days. ‘Appropriate care’ was sought by 410 (95.1%) out of 431 mothers interviewed during the child’s illness, whereas 407 (94.4%) mothers sought ‘prompt care’ and 388 (90.02%) mothers sought ‘appropriate and prompt care’. Socio-demographic characteristics of mothers according to outcome variables are shown in [Table/Fig-2]. A logistic regression analysis showed that only maternal age plays a significant role as to provide prompt and appropriate care (p <0.04).
Socio-demographic variables and health care seeking behaviour (N=1903).
| Parameters | Appropriate Care |
|---|
| Prompt (<24hr) | Not Prompt (>24hr) |
|---|
| Maternal Age (Yr) |
| <20 | 3 (50%) | 3 (50%) |
| 20-25 | 94 (93.1%) | 7 (6.9%) |
| 25-30 | 197 (96.6%) | 7 (3.4%) |
| 30-35 | 69 (93.2%) | 5 (6.8%) |
| >35 | 25 (100%) | 0 (0%) |
| Parity |
| 1 | 151 (92.1%) | 13 (7.9%) |
| 2 | 172 (96.6%) | 6 (3.4%) |
| 3 | 46 (97.9%) | 1 (2.1%) |
| >4 | 19 (90.5%) | 2 (9.5%) |
| Education |
| Illiterate | 11 (100%) | 0 (0%) |
| Secondary | 161 (95.3%) | 8 (4.7%) |
| Intermediate | 184 (94.8%) | 10 (5.2%) |
| Degree | 32 (88.9%) | 4 (11.1%) |
| Income (Rs) |
| <1000 | 54 (93.1%) | 4 (6.9%) |
| 1001-2000 | 72 (97.3%) | 2 (2.7%) |
| 2001-3000 | 32 (100%) | 0 (0%) |
| >3000 | 230 (93.5%) | 16 (6.5%) |
| Distance (km) |
| <1 | 118 (95.2%) | 6 (4.8%) |
| 2-5 | 253 (95.1%) | 13 (4.9%) |
| 5-10 | 15 (83.3%) | 3 (16.7%) |
| 10-20 | 2 (100%) | 0 (0%) |
Private Health Care System (PHCS) was the most common source of health care, 335 (77.7%) as compared to PHS 75 (17.4%). Other means of seeking health care were over the counter medication in 6 (1.4%), home remedy and traditional healers in 3 (0.7%).
In income group less than Rs.1000, 22 (36.7%) sought health care from PHS and 37 (61.7%) from PHCS. [Table/Fig-3] shows source of health care sought by various income groups. Mean expenditure for illness in PHS was Rs.236 while in the PHCS Rs.514. Doctors charges were a mean of Rs.104 in PHCS as to Rs.54.6 in PHS, while medication expenditure was Rs.187.5 and Rs.55.6 respectively. No significant difference was with respect to travel (p<0.7) and investigation (p<0.3) expenditure. [Table/Fig-4] shows expenditure in PHCS and PHS.
Source of health care sought by various income groups (N=431).
| Source of Health Care | Monthly Parental Income |
|---|
| <1000 | 1000-3000 | >3000 |
|---|
| Govt Hospital (PHS) | 22 (36.7%) | 26 (23.9%) | 27 (10.5%) |
| Private (PHCS) | 37 (61.7%) | 79 (72.5%) | 214 (83.3%) |
| Home remedy | 1 (1.7%) | 0 (0%) | 8 (3.1%) |
| Traditional healers | 0 (0%) | 2 (1.8%) | 1 (0.4%) |
| OTC | 0 (0%) | 1 (0.9%) | 2 (0.8%) |
| Others | 0 (0%) | 1 (0.9%) | 5 (1.9%) |
Expenditure in public and private health systems (N=399).
| Source of Health Care | Mean Expenditure (Rs) | Std. Deviation | Z |
|---|
| Doctors | Govt. hospital (PHS) | 54.6667 | 239.35490 | 6.71800 |
| Private hospital (PHCS) | 104.3134 | 294.10777 | p<0.001 vhs |
| Medication | Govt. hospital (PHS) | 54.6667 | 109.02620 | 5.94200 |
| Private hospital (PHCS) | 187.5791 | 431.08413 | p<0.001 vhs |
| Travel | Govt. hospital (PHS) | 31.0267 | 48.98013 | 0.38500 |
| Private hospital (PHCS) | 43.7343 | 89.04331 | p<0.7 ns |
| Investigations | Govt. hospital (PHS) | 24.6667 | 73.69281 | 1.01800 |
| Private hospital (PHCS) | 24.1940 | 125.73297 | p<0.309 ns |
| Total | Govt. hospital (PHS) | 236.0156 | 419.81094 | 5.97700 |
| Private hospital (PHCS) | 514.5480 | 956.65834 | p<0.001 vhs |
Paradoxically mean expenditure of Rs.637 was seen in income group of less than Rs.1000. [Table/Fig-5] shows details of expenditure in various income groups. It is evident from [Table/Fig-5] that mothers of income group less than Rs.1000 have been spending more for medication and doctors charges during illness as compared to the other groups. Further in the study it was analysed that there was no difference in expenditure among income groups with respect to illness. However, study was a single-visit interview with recall period of four weeks. Duration of illness of disease was not taken into consideration while calculating average expenditure.
Breakdown of expenditure in various income groups: (N=399).
| Type of Expenditure | Income Groups | Mean Expenditure (Rs) | Std. Deviation | H | p |
|---|
| Doctors charge | <1000 | 378.5484 | 711.52558 | 3.32 | 0.191 ns |
| 1001-3000 | 113.0120 | 142.36234 |
| >3000 | 109.3373 | 277.32846 |
| Medication | <1000 | 626.7500 | 1043.74318 | 9.28 | 0.01 hs |
| 1001-3000 | 188.1707 | 368.78723 |
| >3000 | 193.2865 | 281.38582 |
| Travel | <1000 | 67.0488 | 110.97791 | 9.36 | 0.009 hs |
| 1001-3000 | 74.5000 | 127.00862 |
| >3000 | 59.3097 | 74.64110 |
| Laboratory | <1000 | 289.3750 | 227.66576 | 1.67 | 0.433 ns |
| 1001-3000 | 276.9231 | 97.07253 |
| >3000 | 367.2727 | 479.29304 |
| Total | <1000 | 637.7143 | 1526.10726 | 15.85 | <0.001 vhs |
| 1001-3000 | 377.3861 | 573.95965 |
| >3000 | 452.1901 | 782.79046 |
Mothers who had breast fed their babies within first two hours of life spent a mean of Rs 409.33 (N=337) while those who fed beyond two hours, mean Rs729.74 (N=62) [Table/Fig-6].
Initiation of breastfeed and health care expenditure (N=399).
| D1 | Initiation of Breast feed | N | Mean | Std. Deviation | Minimum | Maximum |
|---|
| <2hr | 337 | 409.33 | 733.9515 | 10.00 | 5800.00 |
| >2hr | 62 | 729.7419 | 1471.81150 | 24.00 | 8000.00 |
Discussion
Results indicate that a section of population in low socio-economic group do not possess BPL card and thereby, are denied of PHS benefits. Most mothers were aware of danger signs and were able to give prompt and appropriate care to their children Studies elsewhere reported lack of access to health care due to high cost, as the most common deterrent to optimal HCSB [9,10]. Similar illness in the past can motivate mothers to play a ‘waiting game’ to see if the illness subsides on its own, particularly in situations where the cost of care is prime inhibitory factor [11]. Some studies have reported that care seeking behaviour is predicted by household size, age and education of mother [12]. However in the present study, only mother’s age had a positive correlation with health seeking for child, barring literacy, occupation, income and parity. Financial constraints and poor connectivity were barriers for early care seeking as reported by Mittal V et al., [13]. However, availability of health services within short distances indicates good accessibility to healthcare in district, hence not an obstacle for seeking health in the present study. The treatment taken from PHS facility is significantly lower than from the PHCS. Majority of mothers, irrespective of demographic profile sought prompt and appropriate care for their child and mainly from PHCS. The study accounts limited role of unqualified or traditional practitioners and over the counter medications. This indicates good accessibility to healthcare and awareness regarding health in the community of the district. One interesting findings observed in the study is that mothers from the lowest socio-economic group (income <Rs.1000 per month), provided prompt and appropriate care, however incurring higher expenditure for illness. This could be explained by the vulnerability integrated in HCSB. Lack of resources hamper adequate treatment, favour development of parasite resistance, illness recrudescence and prolongation, ultimately increasing direct, indirect and opportunistic costs. Longer duration of illness can lead to selling of assets and other coping strategies, pushing the household into the vulnerability spiral. In these households malnourishment thrives (not only in children) but childcare takes a backseat with undue burden on mothers, hereby increasing the vulnerability to illness.
It is often believed that in PHS, essential drugs are available at no cost to patients. However, there are hidden expenditures in the form of consultation fee to doctors and travel expenditure. Parents have to spend for medications that are not available or not supplied due to poor logistics of drug supply system. The poorer sections of community can become further impoverished by health care costs. However, good HCSB in the community of the district is reflected by IMR (10.9). Hence it is not right to blame the community for deficiencies in the system. Data on personal health care expenditure should be useful for ascertaining the capacity of people to pay for medical services, there by curtailing impoverished care. There are very few studies regarding HCSB in the community and this behaviour is probably under utilised by the policy makers. An interesting observation on analysis of our study data is that those mothers who initiated breastfeeding within two hours of life had less expenditure (Rs.409.33) as compared to those who initiated after more than two hours (Rs.729.74). This may be due to exclusive breast feeding established and benefits thereafter. Further studies are needed to substantiate this finding and analyse the reason. Information on HCSB and expenditure can be useful for assessing the feasibility and impact of such efforts: how much can be recovered and from whom; what will be the impact on access to services and, ultimately, health.
Conclusion
• Majority of mothers were aware of danger signs. Health services were available within short distances indicating good access to healthcare in the district.
• Contrary to the common belief, most mothers sought prompt and appropriate care irrespective of their economic status, literacy, occupation, parity and distance from health care provider.
• Significant percentage of needy families with monthly income <Rs.1000 do not have BPL cards and are deprived of benefits, while 47.6 % of BPL cardholders came from higher income group availing benefits meant for BPL families, contributing to “impoverished care”
• A large number of BPL families are seeking care from PHCS where expenditure is double the amount spent in PHS thus facilitating poverty-illness-poverty cycle.
• Initiation of breastfeeding within first two hours of life reduces health care expenditure for childhood illness.