Direct and indirect expenses incurred from critical care lead to further deterioration of already poor classes [4]. Pursuing social support and positive reappraisal are most commonly used strategies by parents [5,6]. Parents have to change their lifestyle to give time to the child who is under treatment and also at the same time stay away from work, take care of other children at home. These situations can levy extra financial burden and loss of productive hours [7]. Apart from financial burden, seeing a child admitted in PICU can be emotionally disturbing for parents.
Health system of India is becoming highly privatised. In government set-ups, outpatient visits declined from 25% to 20% and hospitalisations declined from 60% to 40% over the decade preceding 2004-05 [8]. Data from the 21st National Sample Survey Office (2015) shows that in government setups in Gujarat, outpatient visits declined from 21% to 19.5%, hospitalisation in rural areas declined from 31.3% to 23.4% and urban areas from 26.1% to 23.3% [9].
In developed countries, most of the families are under the cover of the medical insurance and major medical expenses are taken care of by insurance companies [10]. In a developing country like India, there are large economic differences between various socio-economic classes [11]. Very few people can afford insurance cover [12]. According to World Bank statistics (2014), about 21.3% people in India, live on less than 113.5 rupees per day [13]. They manage hospital costs by various means like savings, selling land and assets; borrow from land lords, etc., [14].
The study aimed to assess financial burden and depression amongst parents of a child admitted in PICU and their variance with social support and household coping strategies.
Materials and Methods
A cross-sectional survey was conducted amongst parents of patients (age: 1 month to 18 years) admitted to PICU over 16 consecutive months (June 2014 to September 2015) at rural tertiary care teaching hospital located in Anand, Gujarat. Ethical approval was taken from the Institutional Ethics Committee prior to conduct of the study. Parents who gave written informed consent were included in the study.
Sample Size: As it is an estimation problem, a larger sample size was required to provide stable estimates of various quantities. In absence of national or regional data, we assumed 50% prevalence of depression as this assumption provides maximum sample size that in turn will ensure stability of estimates. Assuming 50% prevalence of depression, we required a sample of at least 97 at 95% confidence level and 10% acceptable error. The sample size was increased to 150 to capture all coping strategies adequately after considering feasibility. A convenient sample of 150 parents was interviewed over the period of the 16 months. Parents who had a child admitted in the PICU were approached and briefed about the purpose and procedures of the study. They were interviewed by one of the authors, in the waiting area of the PICU, one to two days before discharge. Parents who experienced death of a child during hospitalisation were excluded from the study.
Instruments: Structured questionnaires were used to collect the following:
1) Socio-demographic details of the parent and the child;
2) PHQ-9 is a validated questionnaire to screen for depression. Cut-off scores used were 0-4 for no or minimal depression, 5-9 for mild depression, 10-27 for moderate to severe depression. In comparison to a mental health provider structured interview, scores of 5-9 on PHQ-9 represent respondents with either no depression or sub-threshold depression (minor depression and dysthymia). PHQ-9 score ≥10 has a sensitivity of 88% and a specificity of 88% for major depression [15];
3) Financial burden and household coping strategies: To measure these constructs we collected data on: a) approximate medical cost incurred prior to hospitalisation (Private doctor fees, traditional healer, medicines, investigations); b) approximate non-medical cost incurred prior to hospitalisation (Travel, “special food”, other); c) actual medical cost incurred post hospitalisation (including consultation fees, medicine, investigations, excluding any insurance benefits availed); d) approximate non-medical cost incurred post hospitalisation. We also collected from parents estimated cost of treatment provided to parents at the time of admission, lost productivity in terms of number of days family members having to stay away from work and household coping strategies employed to meet the economic burden;
4) Family social support: Parents were interviewed to find sources of personal and emotional support for the family.
Statistical Analysis
Descriptive statistics {mean (SD), frequency (%), Median (IQR) etc.,}. were used to depict the characteristics of the study population. Chi-Square test/Analysis of Variance were employed to check associations depending upon the type of variables involved. Analysis was done by using STATA (14.2).
Results
Demographics: A total of 150 parents of 150 children admitted to PICU were included in the study. Most informants were Hindu, fathers, residing in rural areas, living in joint family. All informants were married. Mean age of the fathers was 31.22 years (range 23 to 50) and mean age of mothers was 30.39 years (range 22 to 42). Very few had any medical insurance and very few had BPL ration card. Mean monthly family income was 6186.3 rupees and median was 5000 rupees.
Majority of the children admitted to PICU were males, admitted during day time and most admissions were unplanned. The median duration of PICU stay was four days (IQR: 2, 6) and median duration of hospital stay was six days (IQR: 3.75, 10). Almost all the admitted children needed oxygen, fluids and ventilator support [Table/Fig-1].
Sociodemographic characteristics and clinical profile of study population.
| Particulars | Frequency (%) |
|---|
| Patient profile |
| Gender (Male) | 89 (59.3%) |
| Birth Order |
| 1 | 85 (56.7%) |
| 2 | 50 (33.3%) |
| ≥3 | 15 (10%) |
| Time of admission |
| Day | 83 (55.3%) |
| Evening | 24 (16%) |
| Night | 43 (28.7%) |
| Unplanned Admission | 146 (97.3%) |
| Diagnostic category |
| Respiratory | 48 (32.0%) |
| Neurological | 34 (22.67%) |
| RTA/Head injury | 17 (11.33%) |
| Other | 51 (34.0%) |
| Needed Oxygen | 148 (98.7%) |
| Needed Fluids | 149 (99.3%) |
| Needed ventilator support | 146 (97.3%) |
| Median (IQR). PICU stay in days | 4 (2,6) |
| Median (IQR). Hospital stay in days | 6 (3.75,10) |
| Caregiver’s Profile |
| Informant (Father) | 106 (70.7%) |
| Residence (Rural) | 87 (58.0%) |
| Family type (Joint) | 87 (58.0%) |
| Medical Insurance available | 5 (3.3%) |
| Below Poverty Line Ration card | 9 (6%) |
| Religion |
| Hindu | 121 (80.7%) |
| Muslim | 29 (19.3%) |
| Mode of Transport |
| Ambulance | 64 (42.7%) |
| Rickshaw/Car | 86 (57.33%) |
Financial Burden: Median (IQR) direct out-of-pocket cost for the study population was INR 26,050 (12000, 50000). Median monthly income to cost ratio was 5.55. The median (IQR) medical and non-medical cost for the study population was INR 20,000 (13725, 50375) and INR 1,200 (600, 2525) respectively. Median cost for travel was INR 650 and median cost for food was INR 500. Indirect cost was measured using number of day’s family member(s) had to stay away from work. For most of the children admitted, their fathers had to stay away from work (n=149, median duration 6 days) and for 12 children, grandfathers stayed away from work (median duration 5 days). Only a few cases had other relatives staying away from work and hence not reported. The Median (IQR) difference between estimated cost on admission and actual medical cost incurred INR 0 (IQR: 0, 5000).
As shown in [Table/Fig-2], medical cost was not significantly different according to type, time of admission, need for ventilation and diagnosis. There was positive correlation between PICU stay duration and medical cost (r=0.49) and also positive correlation between hospital stay duration and medical cost (r=0.51).
Variance in financial burden according to child’s admission characteristics (N=143*).
| Variable | Characteristic | Number | Medical cost (INR)Mean (SD) | p-value |
|---|
| Time of admission(n=143) | Day | 80 | 31700 (33490) | 0.356 |
| Evening | 23 | 40956 (32672) |
| Night | 40 | 30150 (20512) |
| Type of admission(n=143) | Planned | 4 | 13500 (08582) | 0.198 |
| Unplanned | 139 | 33309 (30534) |
| Diagnostic category (n=143) | Respiratory | 44 | 32568 (27017) | 0.716 |
| Neurological | 31 | 36387 (33148) |
| RTA/Head injury | 17 | 37058 (30021) |
| Other | 50 | 29460 (32009) |
*7 records were excluded from this analysis as these were considered extreme outliers with medical cost >200000 rupees
Household Coping Strategies: As shown in [Table/Fig-3], Borrowing money from relatives and friends (58%), using savings (28.7) and selling assets (28%) were the most frequently used household coping strategy. Minority had to borrow from moneylenders. The mean number of household strategies used per family was 1.34.
Household coping strategies (n=150).
| Household coping strategies | n (%) | Mean amount generated (INR) | Family typeNumber(Percentage) | Type of ration cardNumber(Percentage) | Access to other health care benefitsNumber(Percentage) |
|---|
| | | Joint | Nuclear | Don’t have | BPL | Krupa* | None |
|---|
| Used savings | 43 (28.7) | 11523 | 26 (60.4) | 17 (39.6) | 9 (20.9) | 0 | 4 (9.3) | 39 (90.7) |
| Sold assets | 42 (28) | 2361 | 22 (52.3) | 20 (47.7) | 3 (7.1) | 2 (4.7) | 0 | 42 (100) |
| Borrowed from money lender | 21 (14) | 3946 | 8 (38) | 13 (62) | 3 (14.2) | 0 | 1 (4.7) | 20 (95.3) |
| Borrowed from relatives/friends | 87 (58) | 9090 | 53 (60.9) | 34 (39.1) | 8 (9.2) | 4 (4.6) | 3 (3.4) | 84 (96.6) |
| Borrowed from others | 3 (2) | 4400 | 2 (66.7) | 1 (33.3) | 0 | 1 (33.3) | 0 | 3 (100) |
| Reduced household consumptions | 4 (2.7) | 103 | 2 (50) | 2 (50) | 1 (25) | 0 | 1 (25) | 3 (75) |
* Krupa is a low-cost health insurance scheme offered by the local hospital
Depression and Sources of Personal, Emotional Support: The mean (SD) PHQ-9 score was 1.07(0.26). Eleven parents (Nine fathers and two mothers) had mild depression on PHQ-9, none of the parents had moderate to severe depression. Skewed distribution of father:mother may be a limitation with respect to analysis of psychological burden.
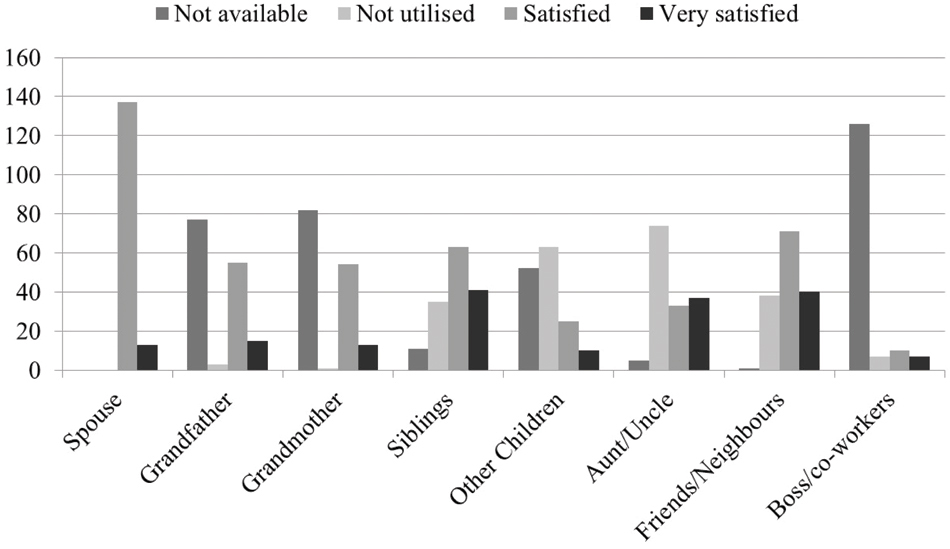
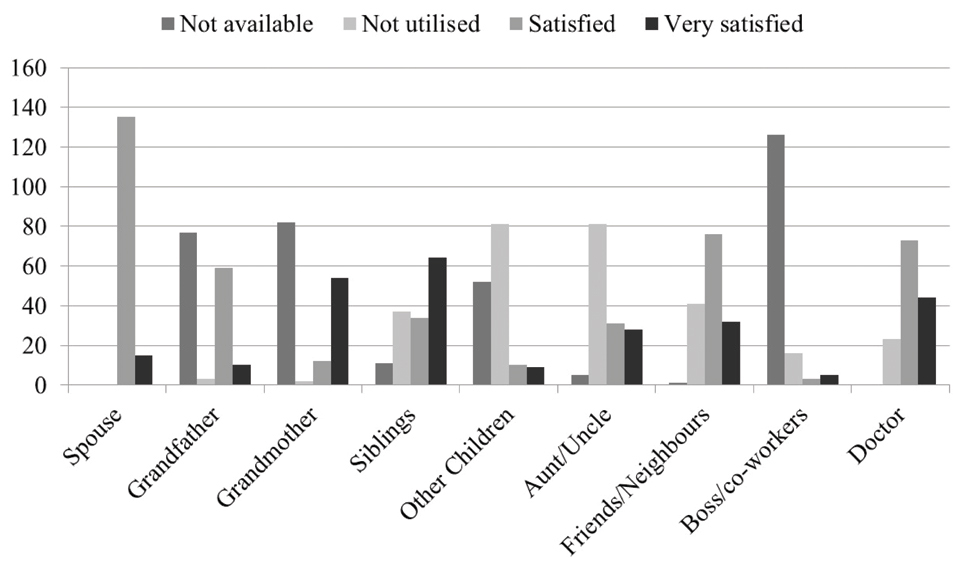
As can be derived from [Table/Fig-4,5], Spouse, friends and neighbours and siblings were the most instrumental in providing personal support like doing household chores, getting things from home, help with transportation etc., while child was hospitalised. Spouse, friends and neighbours, siblings, grandparents and doctor were instrumental in providing emotional support. None of the families got such supports from any organisation/agency or religious support group.
Sources of Personal support for Parents of Children Admitted to Pediatric Intensive Care Unit (PICU).
Sources of Emotional support for Parents of Children Admitted to Pediatric Intensive Care Unit (PICU).
Discussion
There was slightly higher representation of rural population (58%) and joint families. Monthly income of parents was low and this is in keeping with World Bank data [16]. In contrast to western countries, majority did not had access to any medical insurance [10,17]. Lacking insurance cover, most people from middle and low socio-economic status may feel the burden of intensive care to be unbearable and this may ultimately contribute to high Discharge Against Medical Advise rates, eventual mortality and morbidity. Indian government has recently started low cost life insurance schemes (Pradhan Mantri Suraksha Bima Yojana, Pradhan Mantri Jeevan Jyoti Bima Yojana, Mukhyamantri Amrutum), similar low cost, affordable health insurance schemes may help lower health care burden on individuals in India.
In contrast to Western setups where most of the PICU admissions occur in a planned manner and post-surgical [18], majority of admissions in our study were unplanned as seen earlier [19]. Unplanned admissions do not allow parents to plan for the sudden financial expenditure and can be distressing for parents.
Acute respiratory illness is one of the most common causes of under-five mortality in the country [20]. The median duration of PICU stay (four days) and median duration of hospital stay (six days) in our study corroborates with previous studies [4,21]. Moderate to strong positive correlation between duration of PICU stay (r=0.49), duration of hospital stay (r=0.59) and medical cost is not a new finding, but clinicians should consider early ambulation and discharge in individual cases.
The median (IQR) medical and non-medical cost for the study population was INR 20,000 (IQR: 13725, 50375), and INR 1,200 (IQR: 600, 2525) respectively. When compared with the average income, the median income to cost ratio was 5.5. These findings combined with lack of insurance coverage suggest that direct and indirect expenses incurred from critical care may push parents further into poverty. Variance in medical cost was not significant according to type, time of admission, need for ventilation and diagnosis. This might be because ours is the only tertiary care hospital in nearby rural area which receives critical patients from periphery.
Most of the times the child’s father had to stay away from work to take care of the admitted child. This unplanned leave from work generates indirect cost (loss of wages). Borrowing money from others (relatives/friends) (58%), using savings (28.7%) and selling assets (28%) were the most frequently used household coping strategy. An earlier study on economic and psychological difficulties in parents of patient with epilepsy found that 22% were receiving monetary support from other members in the family [22]. The main challenges confronting free public hospitals are deficient infrastructure, deficient manpower, unmanaged patient load, equivocal quality of services, high out of pocket expenditure [23]. The failure of many government schemes offering free healthcare can be attributed to India’s health policy failures because whatever little is spent on health is not used effectively.
An earlier study found, 55% of the parents had drafted the help of other family members (grandparents, elder children and other senior members in the case of a joint family) to take care of the child [22]. Low levels of psychological problem (n=11) may be due to higher representation of fathers. The level of psychological burden was quite low as compared parents of children with chronic disease [24].
Limitation
Small sample size, data from single private care centre and cross-sectional study design are few limitations of the study. Also, questionnaire was subjected at the time of discharge which might have different level of effect on emotional aspect.
Conclusion
Unplanned admission, lack of insurance cover and significant direct medical cost as inferred from the high income to cost ratio, indirect cost incurred by staying away from work may push already impoverished families further into poverty.
*7 records were excluded from this analysis as these were considered extreme outliers with medical cost >200000 rupees
* Krupa is a low-cost health insurance scheme offered by the local hospital