Primary Myelofibrosis with Mesenteric Extramedullary Haematopoiesis
Saurabh Kumar1, Shaloo Shaloo2, Juhi Chawla3, Subha Ashok4, Shalini Thapar Laroia5
1 Assistant Professor, Department of Radiology, Institute of Liver and Biliary Sciences, New Delhi, India.
2 Resident, Department of Radiology, Institute of Liver and Biliary Sciences, New Delhi, India.
3 Resident, Department of Radiology, Institute of Liver and Biliary Sciences, New Delhi, India.
4 Resident, Department of Radiology, Institute of Liver and Biliary Sciences, New Delhi, India.
5 Additional Professor, Department of Radiology, Institute of Liver and Biliary Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saurabh Kumar, Assistant Professor, Department of Radiology Institute of Liver and Biliary Sciences (ILBS), D-1, Vasant Kunj, New Delhi, Delhi, India.
E-mail: sunny_mamcd911@yahoo.com
Primary myelofibrosis or chronic idiopathic myelofibrosis is a myeloproliferative neoplasm characterized by proliferation of abnormal haematopoietic stem cells in bone marrow resulting in replacement of marrow with fibrotic scar tissue. Extramedullary Haematopoiesis (EMH) as a compensatory phenomenon in myelofibrosis can lead to hepatosplenomegaly with diffuse organ infiltration or focal deposits. Peritoneal involvement of EMH is rare and can present with peritoneal or serosal implants which can mimic malignancy. We present a case of diffuse peritoneal /mesenteric extramedullary haematopoiesis with hepatosplenomegaly as an initial presentation in patient of idiopathic myelofibrosis.
Megakaryocytes, Myeloproliferative neoplasm, Osteosclerosis
Case Report
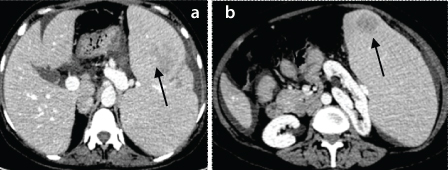
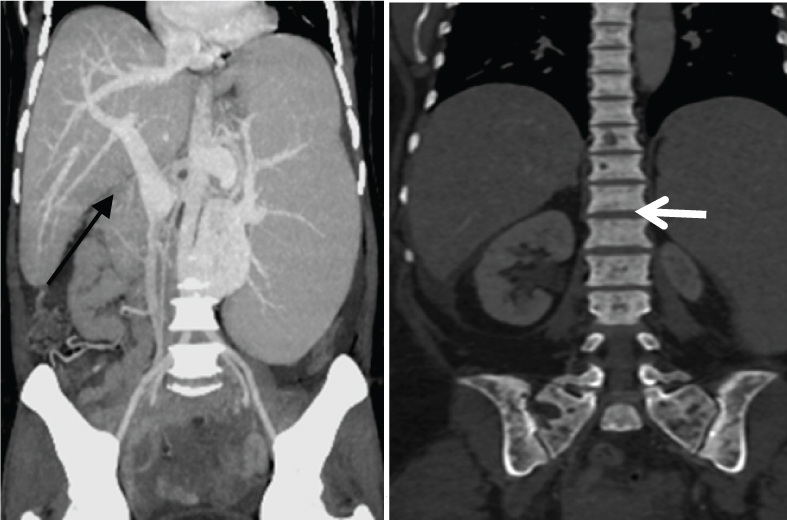
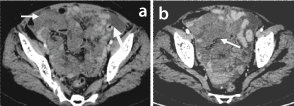
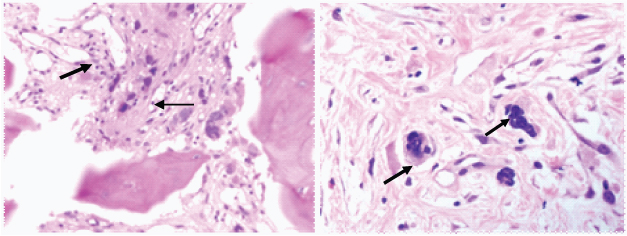
A 62-year-old woman presented with a six months history of progressive abdominal distention, loss of appetite and weightloss. Physical examination revealed mild pallor, abdominal hepato-splenomegaly with tenderness in lower abdomen. Rest of physical examination was unremarkable. Blood investigations revealed anaemia, leuokopenia with peripheral leukoerythroblastosis. Contrast-Enhanced CT abdomen showed hepatomegaly, massive splenomegaly with intrasplenic well defined mildly enhancing hypodense soft tissue mass lesions [Table/Fig-1a and b]. There were features of portal hypertension with prominent spleno-portal axis [Table/Fig-2a] and few abdominal collaterals. Visualised pelvic bones and vertebrae show diffuse sclerosis [Table/Fig-2b]. In addition there was mild ascites with infiltration of the small bowel mesentery and omentum with mildly enhancing soft tissue [Table/Fig-3a and b] which is seen extending along the serosal surface of ileal loops. Uterus and adnexa were unremarkable. Based upon radiological and peripheral blood smear findings possibility of marrow infiltrative disorder likely primary myelofibrosis, with hepato-splenomegaly and secondary portal hypertension was made, which was confirmed on bone marrow aspirate/biopsy which showed hypocellular marrow spaces with dense fibrosis, collagenous deposit with suppressed erythroid and myeloid series and presence of atypical megakaryocytes. JAK2 mutation positivity was noted. The intrasplenic lesions and mesenteric soft tissue were thought to be representing extramedullary haematopoiesis which was confirmed histopathologically. Mesenteric biopsy specimen histopathology [Table/Fig-4a and b] showed large abnormal megakaryocytes embedded within fibrocollagenous stroma, which stained positively for factor VIII-related antigen and of platlet factor IV, features were consistent with extramedullary haematopoiesis. Tissue specimens were negative for malignancy and infection (tuberculosis). The patient was started on oral ruxolitinib (JAK2 tyrosine kinase inhibitor) and was planned for splenectomy.
Axial CECT abdomen (venous phase) image showing hepato -splenomegaly with hypodense lesions in splenic parenchyma (arrow).
Coronal MIP image abdomen showing dilated splenoportal axis (arrow) suggesting portal hypertension. Coronal image (bony window) abdomen showing diffuse osteosclerosis (arrow).
Axial CECT abdomen image showing mesenteric soft tissue deposits (arrow) with ascites.
Bone marrow biopsy slide showing increased fibrosis (thin arrow) with presence of atypical megakaryocyte (thick arrow) (40X). (b) – Mesenteric soft tissue biopsy slide showing fibrocollagenous tissue with entrapped large cells with multilobated nuclei and moderate cytoplasm- atypical megakaryocyte (arrows) (40X).
Discussion
Primary myelofibrosis is a rare disorder in which normal bone marrow is replaced by fibrous scar tissue preventing the adequate production of red cells, white cells and platelets [1]. It can occur at any age but common age of presentation is between 60-70 years and histopathologicaly classified either as JAK2 mutation positive or negative [2]. Presentation is generally with non specific symptoms of fever, weight loss, night sweats and anaemia and in few cases, disorder is picked up incidentally in routine blood examination. Splenomegaly is a consistent finding secondary to extramedullaryhaematopoiesis and is seen in all patients [3].
Extramedullary Haematopoiesis is the presence of haemopoietic tissues in location other then bone marrow medullary space [4]. It can be seen in variety of disorders including chronic haemolytic anaemias and myelofibrosis. The common site of involvement is liver, spleen and lymph nodes leading to hepato splenomegaly and lymphadenopathy, Central nervous system, paraspinal region, renal and gastrointestinal tract being relative uncommon sites. Haematopoietic mass presenting with intestinal, gastric obstruction or rectal stenosis or simulating carcinoma have been described in literature with only few case reports of it presenting as diffuse mesenteric infiltration [5,6]. In one of the case report the presentation was similar as was seen in our case with diffuse mesenteric soft tissue infiltration and ascites which was later proven histopathologically to be extramedullary haematopoiesis [6].
The imaging findings of extramedullary haematopoiesis are dependent on the relative amounts of the normal marrow constituents—fat, haematopoietic cells and fibrosis which can be better differentiated on MRI [7]. Computed tomography generally reveals a heterogeneous hypodense mass with absent, minimal, or heterogeneous enhancement [6]. Due to presence of diffuse mesenteric and serosal soft tissue infiltration in the present case close differential of Carcinomatosis, Lymphomatosis, leukaemic deposits, and infective process (like tuberculosis) were also considered as we know imaging appearances of focal and diffuse peritoneal extramedullary haematopoiesis are nonspecific and one has to rely on histopathology for differentiation.
Possible explanation of portal hypertension, which can occur in around 7% of patients with myelofibrosis, includes sinusoidal narrowing and increase intrahepatic resistance by infiltration of myeloid cells or due to increase portal blood flow secondary to splenomegaly which is the proposed mechanisms in patients with myelofibrosis besides portal vein thrombosis [8]. Ascites which occur in around 5-10% of cases of myelofibrosis and is seen in the present case can be secondary to portal hypertension [6]. Other proposed mechanism of ascites being rupture of hepato splenic nodules of extramedullary haematopoiesis into the peritoneal cavity or peritoneal implants of extramedullary haematopoiesis. Diffuse osteosclerosis as seen in the present case involving axial and appendicular skelton is well documented in patients with myelofibrosis.
Treatment option includes splenectomy for relieving symptoms of pain and portal hypertension and controlling peritoneal extramedullary haematopoiesis with low-dose abdominal radiation therapy, direct intraperitoneal chemotherapy and oral thalidomide [9]. Ruxolitinibis found to be beneficial in patients with JAK2 mutation positivity [10]. The patient was put on Ruxolitinib and is planned for splenectomy.
Conclusion
Extramedullary haematopoiesis should always be kept as a differential in patients of idiopathic myelofibrosis who present with diffuse peritoneal/mesenteric infiltrating mass besides carcinomatosis, leukaemic deposits or tuberculosis. Though imaging findings are sometimes non specific one can always rely on histopathological analysis.
[1]. Barosi G, Myelofibrosis with myeloid metaplasia: diagnostic definition and prognostic classification for clinical studies and treatment guidelinesJ Clin Oncol 1999 17(9):2954-70.10.1200/JCO.1999.17.9.295410561375 [Google Scholar] [CrossRef] [PubMed]
[2]. Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK, Typical and atypical presentations of extramedullaryhemopoiesisAJR 2002 179(5):1239-43.10.2214/ajr.179.5.179123912388506 [Google Scholar] [CrossRef] [PubMed]
[3]. Saboo SS, Krajewski KM, O’Regan KN, Giardino A, Brown JR, Ramaiyua N, Spleen in haematological malignancies: spectrum of imaging findingsBr J Radiol 2012 85(1009):81-92.10.1259/bjr/3154296422096219 [Google Scholar] [CrossRef] [PubMed]
[4]. Shaver RW, Clore FC, Extramedullaryhematopoiesis in myeloid metaplasiaAJR Am J Roentgenol 1981 137(4):874-76.10.2214/ajr.137.4.8746974990 [Google Scholar] [CrossRef] [PubMed]
[5]. Wei X-Q, Zheng Z-H, Jin Y, Tao J, Abassa K-K, Wen Z-F, Intestinal obstruction caused by extramedullaryhematopoiesis and ascites in primary myelofibrosisWorld J Gastroenterol 2014 20(33):11921-26.10.3748/wjg.v20.i33.1192125206301 [Google Scholar] [CrossRef] [PubMed]
[6]. Holden C, Hennessy O, Lee W, Diffuse mesenteric extramedullaryhematopoiesis with ascites: sonography, CT, and MRI findingsAmerican Journal of Roentgenology 2006 186(2):507-09.10.2214/AJR.04.178816423960 [Google Scholar] [CrossRef] [PubMed]
[7]. Gupta P, Naran A, Auh YH, Chung JS, Focal intrahepatic extramedullaryhematopoiesis presenting as fatty lesionsAJR 2004 182(4):1031-32.10.2214/ajr.182.4.182103115039182 [Google Scholar] [CrossRef] [PubMed]
[8]. Lioté F, Yeni P, Teillet-Thiebaud F, Barge J, Devars Du Mayne JF, Flamant Y, Ascites revealing peritoneal and hepatic extramedullaryhematopoiesis with peliosis in agnogenic myeloid metaplasia: case report and review of the literatureAm J Med 1991 90(1):111-17.10.1016/0002-9343(91)90513-W [Google Scholar] [CrossRef]
[9]. Elliott MA, Mesa RA, Li CY, Hook CC, Ansell SM, Levitt RM, Thalidomide treatment in myelofibrosis with myeloid metaplasiaBr J Haematol 2002 117(2):288-96.10.1046/j.1365-2141.2002.03443.x11972510 [Google Scholar] [CrossRef] [PubMed]
[10]. Tefferi A, Vainchenker W, Myeloproliferative neoplasms: molecular pathophysiology, essential clinical understanding, and treatment strategiesJ Clin Oncol 2011 29(5):573-82.10.1200/JCO.2010.29.871121220604 [Google Scholar] [CrossRef] [PubMed]