There is paucity of literature on mental morbidity of soldiers involved in peacekeeping activity despite 60 years of India’s participation in United Nations (UN) Peacekeeping missions. Peacekeeping refers to a military intervention in a conflicted area authorised by the UN Security Council [1]. Many service members from different countries have participated in both UN and North Atlantic Treaty Organisation (NATO) based peacekeeping missions. Indian soldiers have proven their worth in more than 63% of UN’s 69 missions so far and are currently active in 11 of the 16 missions. [2]. However, these acts are not without cost. So far till 30 June 2018, there have been 163 mortalities [3]. With persisting hostilities in Syria and Africa, peacekeeping activity will become harsher and our policy makers must have available mental health inputs to supervise, prevent and control mental morbidity and repatriation.
In Peacekeeping missions there is overseas deployment for troops, hostile and harsh conditions, presence of vectors, loneliness, and mobile or on foot dangerous patrolling, armed conflict and disregard on the part of some local parties for peacekeepers’ security and role. This places the Indian peacekeepers at risk for mental health problems. ‘Peacekeeper’s stress syndrome’ was first described in 1979 in the Norwegian peacekeeping operations [4]. This is now formally acknowledged as a unique problem of UN peacekeeping [5]. Peacekeepers stress syndrome is defined as rage, frustration, feelings of impotence, delusionsand helplessness when confronted with violence and atrocities to which the peacekeeper is unable to respond [6]. Acute stress disorder, PTSD, conversion reaction, depression, alcoholism or drug abuse and somatisation disorder has also been reported in peacekeepers [6].
Taking a look at certain active missions, India’s commitment at South Sudan is handling threat to international security in the region. Indian troops are heavily engaged in upholding the mandate for protection of civilians despite extremely volatile internal situation [7]. In Congo, civilians, humanitarian personnel and human right protectors are under imminent threats of physical violence. Peacekeepers were established to confirm the withdrawal of Isreal forces from Southern Lebanon, restore international peace and security; and assist the government of Lebanon in ensuring the return of its effective authority in area. Indian Peacekeepers supervise the cessation of hostilities, support Lebanese forces in deployment and security, ensure area of operation is not used for hostile activities and assist local population to protect unarmed civilians from physical violence [7]. In Golan, Peacekeepers have to maintain cease-fire following agreement and supervise disengagement of Israel and Syria forces. The United Nations Disengagement Observer force (UNDOF) has been targeted by terrorist groups operating in the area [7]. Attacks on base camps, convoys or during patrols and kidnapping has happened on Indian contingent in past by rebel groups and terrorist. Soldiers have lost lives and also, been witness to atrocities on civilian populations and have handled dead bodies of both civilians and colleagues, more so at Sudan and Congo.
There is considerable knowledge gap in mental health status of Indian peacekeepers. Its the duty of mental health workers and policy makers to fill this void for those who care and sacrifice for International peace. Keeping this in mind, the present study was undertaken. This study is likely to fill the factual void and provide useful information for commanders and policy makers to reduce the repatriation due to mental illness and also to modify the risk factors for mental illness thereby, enhancing their role as peacekeepers. With this aim it was planned to study the sociodemographic profile and mental morbidity in Indian soldiers repatriated from UN Peacekeeping mission.
Materials and Methods
This study was a cross-sectional study conducted in the psychiatry department of a Tertiary Care Army hospital in Delhi. The study was conducted from Jan 2011 to July 2015 and clearance of Hospital ethical committee was undertaken. The patients were all consecutively repatriated Indian soldiers for various UN peacekeeping missions in globe including Congo, Somalia and Golan heights. Total deployment in these areas was 37507. Inclusion criteria was soldier must have been in UN mission deployment at the time of reporting sick to us (while on leave) or have been repatriated from UN mission by health authorities on mental health grounds. Exclusion criteria’s were patients with concurrent serious physical illness and soldiers on foreign assignment but not on UN mission peacekeeping operations. Informed consent of the patient was also taken before including them in the study. All soldiers were male and had at least one previous counter-insurgency exposure before induction into UN mission.
In the first stage, detailed clinical evaluation of an individual was carried out and details recorded as per specifically designed format which included their sociodemographic profile, psychosocial stressors, previous treatment history and lab investigation. They were diagnosed as per International Classification of Diseases (ICD 10) criteria [8] for their psychiatric disability and treated.
When stable in next stage they were assessed for their experiences during Peacekeeping mission by administering them Combat Experiences, Deployment Concerns and Deployment Experiences Scale from Deployment Risk and Resilience Inventory DRRI [9]. Only these three subscales were used from the whole inventory.
(i) Combat experiences: This war-zone factor refers to objective events and circumstances such as firing a weapon, being fired on, being attacked or witnessing an attack (e.g., encountering an explosive device), encountering friendly fire, and going on patrols that involve such experiences and does not include personal interpretations or subjective judgments of the events or circumstances. It is a 17 item scale which utilises six point Likert type scale from never (one), once or twice (two), several times (three), few times each month (four), few times each week (five) to daily (six). Possible range is 17-102. Higher scores indicate intense combat experience.
(ii) Deployment environment: Environmental conditions like lack of desirable food, difficulties in acculturation, privacy issues uncomfortable living arrangements as well as climate factors adversely affect the quality of life during overseas deployment. Deployment environment is a 14 item scale which utilises 5 point Likert type scale from almost none (one), a few times (two), some of the time (three) most of the time (four) to almost all of the time (five). Possible range is 14-70. Higher scores indicate tougher living condition and working environment.
(iii) Deployment concerns: Safety and well being concerns during deployment like fear of nuclear, chemical or biological warfare attacks, ambush attacks negatively impacts psychological and emotional health of the troops. This factor reflects emotional or cognitive appraisals of situations that may or may not accurately represent objective or factual reality. It is a 12 item scale which utilises 5 point Likert type scale from strongly agree (one), somewhat agree (two), neither agree nor disagree (three), somewhat disagree (four) to strongly disagree (five). Possible range is 12-60. Higher scores indicate high concerns. It takes about 20-25 minutes to administer three scales.
Old records of such repatriated soldiers were also studied and where ever required telephonic contact was made with them to further clarify the matters. An attempt was being made to delineate modifiable risk factors which predispose soldier towards repatriation following mental morbidity. A number of statistical tests were performed where categorical data was described as per their frequency and continuous data as mean and standard deviation.
Results
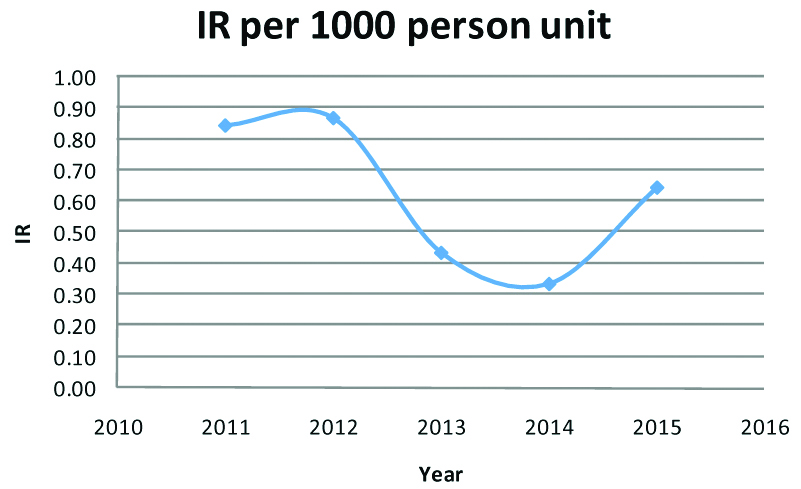
[Table/Fig-1] depicts the incidence of mental illness per year of UN stay. In the year 2011, the incidence rate was 0.85, 2012 it was 0.87, 2013 it was 0.44, in 2014 it was 0.34 and 2015 it was 0.65. A total of 23 patients out of 37507 were diagnosed to have mental illness and repatriated.
Incidence Rate of mental illness per year.
Mean age of soldiers repatriated was 34.87 years (range-26 to 43, sd=5.08) Service bracket of troops ranged from 6 years to 23 years. Mean was 15.5 years. Officers were about 17% and Ranks were 83% of total repatriated patients [Table/Fig-2]. No Junior Commissioned Officer (JCO) was admitted for mental illness. Naik and Havildar rank were maximally represented in repatriated group with 34%. General duty trades men were maximally represented with 47.8%. Soldiers developed symptoms within a month (13%) of arrival, 20% developed within 3 month of arrival. People who outsourced their psychiatric treatment before disembarking were 8.6%, and people with previous service record of mental illness were 4%. Among stressor reported by repatriated soldiers no problem was reported in 34% and death, illness and injury in family by 39%.
Socio demographic profile of repatriated soldiers.
| Mean with SD | Frequency (n=23) |
|---|
| Age | 34.8 years (5.08) | |
| Service (Years) | 15.5 years (3.01) | |
| Age Distribution |
| 26-28 | 4 (17.39%) |
| 29-31 | 2 (8.69%) |
| 32-34 | 4 (17.39%) |
| 35-37 | 3 (13.04%) |
| 38-40 | 8 (34.78%) |
| 41-43 | 2 (8.69%) |
| Service in Years |
| 6-10 | 4 (17.4%) |
| 11-15 | 6 (26%) |
| 16-20 | 9 (39%) |
| >20 | 4 (17.4%) |
| Rank |
| Sepoy | 3 (13%) |
| Naik | 8 (34.78%) |
| Havildar | 8 (34.78%) |
| JCO | 0 (0%) |
| Officers | 4 (17%) |
| Education |
| Matriculation | 5 (21.73%) |
| ISC | 9 (39.13%) |
| Graduate | 8 (34.78%) |
| Postgraduate | 1 (4.34%) |
| Trade |
| Trade Man | 2 (8.6%) |
| Infantry General Duty | 11 (47.8%) |
| Technical General Duty | 3 (13.04%) |
| Special General Duty | 3 (13.04%) |
| Officer | 4 (17.2%) |
| Duration of stay before repatriation |
| 1 month | 3 (13%) |
| 2 month | 4 (17.39%) |
| 3 month | 5 (21.7%) |
| 4-12 month | 11 (47.8%) |
| Psychosocial stressors (note: Multiple stressors can be faced by same person) |
| No problem | 8 (34%) |
| Financial problem | 1 (4.34%) |
| Disciplinary problem | 1 (4.34%) |
| Conflict with spouse | 3 (13%) |
| Self health related problem | 1 (4.34%) |
| Death, illness and Injury in family | 11 (39%) |
| Work Place related problem | 2 (8.6%) |
The mean Combat experience scores of repatriated soldiers were 24.9 (SD 2.76). Mean Deployment concern score was 32.9 (SD 4.2) and Deployment environment was 23.4 (SD 4.2).
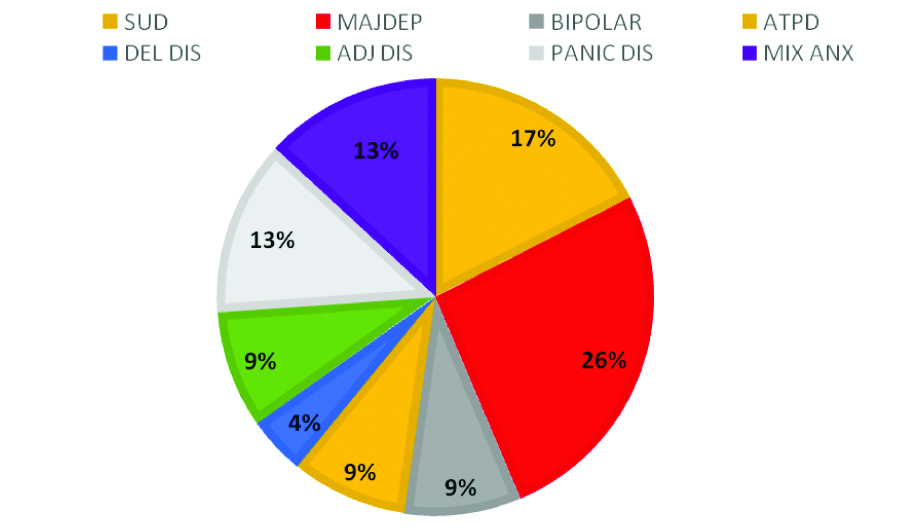
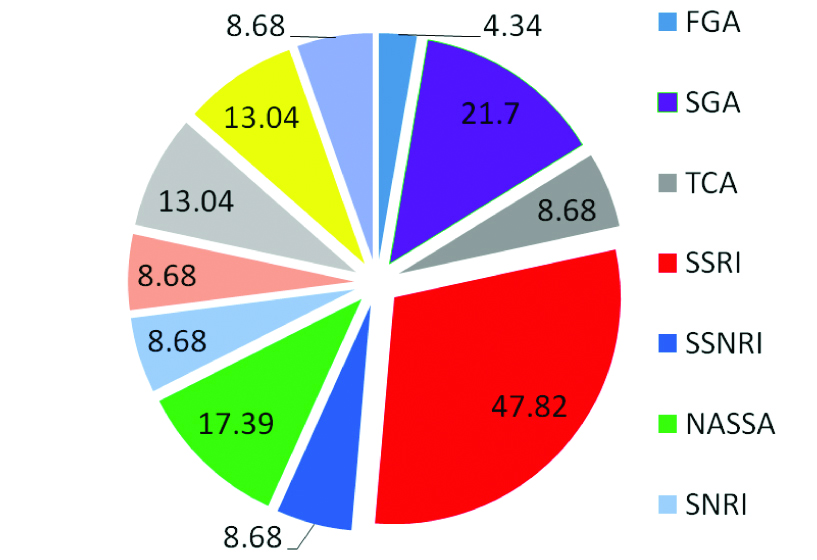
Cases were assessed by psychiatrist as per ICD criteria. Amongst psychiatric morbidity [Table/Fig-3], major depression was observed in 26%. There were no cases of PTSD or attempted suicide. Amongst major psychiatric symptoms reported by repatriated soldiers, sleep disturbance was reported by 25.8%, mood changes, restlessness and appetite changes were reported by 21.5%, suicidal ideations by 13%, needle marks in 4%, anger control was a problem in 13%, delusion by 13%. Patients were treated with various psychotropic drugs [Table/Fig-4].
Mental morbidity profile.
SUD: Substance use disorder; MAJDEP: Major depressive disorder; Bipolar: Bipolar disorder; ATPD: Acute and transient psychotic disorder; DEL DIS: Delusional disorder; ADJ DIS: Adjustment disorder; PANIC DIS: Panic disorder; MIX ANX: Mixed anxiety depressive disorder.
Psychotropic drug profile.
FGA: First generation antipsychotics; SGA: Second generation antipsychotics; TCA: Tri cyclic Antidepressant; SSRI Norepinephrine reuptake inhibitor; SSNRI: Selective serotonin norepinephinephrine reuptake inhibitor; NASSA: Noradrenergic and specific serotonergic antidepressant; SNRI: Serotonin-norepinephrine reuptake inhibitors
Discussion
This study offers first look at the experiences of Indian troops who have been deployed in UN peacekeeping mission across the world since 2011 to 2015. Although the sample is repatriated Indian UN soldiers and, consequently, there are strong limitations to its generalisation, this is one of the first attempts to address the lack of empirical literature on this unique military subpopulation. Most encouraging aspect of the study was incidence of mental illness per year of UN stay was less than one percent and absence of PTSD and suicide attempts in repatriated Indian soldiers. This can be explained in the background that Indian soldiers have had previous exposure to counterinsurgency operations for several decades where operational scenario is similar to peacekeeping mission. This made our soldiers hardy. Secondly policies and programs of Indian army and leaders related to rotation policy, stress management, counsellors and yoga teaching are in place and effective on ground [10].
Injuries, mental illness and alcoholism were responsible for two thirds of all repatriations to home and prior screenings for better psychological health assessment were emphasised [11]. Among persons working in developing countries, psychiatric causes are a frequent reason for premature return to home [12-14]. In our repatriated soldiers, 13% reported symptoms within a month of deployment, 21.7% reported within three month of deployment.
It was revealed by the repatriated soldiers that: (i) they were trying to outsource their mental health treatment and did not declare their mental illness before disembarking and later manifested with relapse in the absence of medicine; (ii) Recovered cases were detailed for UN Mission appointment overlooking their previous mental health records. Past mental health care is established pre-deployment risk factor for post-deployment mental health problems [15,16]. Pre-screening of military personnel deployed to combat/contingency operation has reduced mental health problems and medical evacuations from the field [17]. Such pre-screening can also help reducing repatriation rates. Hence, it is important to review the medical records of the candidates for UN mission, particularly with respect to a previous history of substance abuse and psychiatric illness. Another area which will reduce repatriation is by improving the pre-deployment mental health training which is known to improve post-deployment mental health [18].
The security environment in UN peacekeeping mission is extremely challenging and volatile. Infrequent attacks on base camps convoy or during patrols have happened on Indian contingent by rebel groups and terrorists. Soldiers have also been witness to atrocities to civilian populations and have handled dead bodies of both civilians and colleagues. Deployment Concerns were relatively high as soldiers were concerned about attacks, Improvised Explosive Device (IED), local infections and injury during their overseas deployment which is understandable in context as all of them had their first overseas deployment. However, Combat Experience score was close to lower minimum of 17 (mild to moderate) in our sample. The training and experience in counterinsurgency operations by Indian soldiers as well as several stress busting measures taken by Indian Army might have served them well to deal with combat experience in UN. Similarly, Deployment Environment soldiers expressed satisfaction with the quality of life indicators like physical comforts, food, rest and privacy during UN peacekeeping.
Among the modifiable risk factors reported by soldiers, maximum (39%) reported family stressors and marital discord was reported by 13%. High risk of mental illness in divorced and separated or widowed peacekeepers has been observed [19]. Looking after the families is in best interest of organisation. Felt need of this group should be met by organisation by opening more marital and family counselling centres and employing trained counsellors and therapist for this purpose. Soldiers with sense of well being in the family front are less likely to decompensate on mental health ground. Older personnel are also at increased risk of morbidity in peacekeeping operations [19] akin to our finding where 42% of repatriated soldiers were in older age group of 38 to 43 years.
Major depression was maximally seen followed by substance use disorder, panic disorder, mixed anxiety depressive disorder, bipolar affective disorder, acute and transient psychotic disorder, adjustment disorder and delusion disorder in our soldiers. There were no suicide attempts or any PTSD, though there were suicidal ideations in 13% of repatriated cases. Increased incidence of anxiety, depression [20], suicides, increased alcohol use [21,22], have been reported in the past. Studies have examined the relation between peacekeeping and risk for suicidal ideation and found that exposure to traumatic events during deployment is associated with an increased likelihood of suicidal ideation [23,24]. When compared to studies from other peacekeeping operations, 8% of American peacekeepers were noted to have met diagnostic criteria for PTSD [25], and 15% incidence of PTSD was noticed in a Canadian study of peacekeeping operations to the former Yugoslavia [26].
Other risk factors in peace keepers which predisposes them to mental illness like gender [27] (females more prone to anxiety and depression and men more prone to alcohol abuse), low income, lower rank [28], negativism as personality factor [29] and anxiety traits [30] also needs to be looked into.
Limitation
As already clarified this was a hospital based study which was cross-sectional and hence, it cannot be generalised and no causality can be reflected. Though, PTSD and suicide attempts were not seen in our sample, the absence of them should not be taken as evidence of their absence and long-term follow-up of cases needs to be done.
Implications
There are several impactful implications of our study. First it is giving us insight into the mental illness of repatriated soldiers and covers the knowledge gap for health care givers. Due to stigma in Armed Forces [31] it is seen that men are not reporting mental illness and outsourcing their treatment. Therefore, de-stigmatisation of mental illness and vigorous screening before overseas deployment can further reduce repatriation.
Conclusion
This study is first of its kind on repatriated Indian peacekeepers with respect to mental health issues. The low incidence of mental morbidity, absence of PTSD and suicidal attempts in the study group validates the multi-dimensional approach taken by Indian army to reduce stress in Indian soldiers. However, improving screening measures for mental illness prior to deployment will aid in further reduction of repatriation. Soldiers with sense of well-being and harmony in family are less likely to decompensate on mental health grounds. Further longitudinal studies need to be taken to assess deployment related impact on long-term mental health outcome of Indian soldiers.