This case report describes the successful interceptive treatment approach for two young patients with impacted permanent lateral incisors. The interceptive orthodontic treatment for impaction usually includes extraction of primary tooth, expansion and space opening with fixed appliance. If all kinds of interceptive treatments fail, the surgical intervention is an option by exposing the impacted tooth, then applying traction force to move the impacted tooth to the normal position. However, surgery is not the first option in growing patients since, there is still a chance for spontaneous eruption of the impacted tooth. In the present report, the patients presented to the orthodontic clinic with complaint of non-erupting front teeth after the loss of deciduous teeth, with the eruption of lateral incisors on the contralateral side. The treatment of both patients consisted of maxillary expansion to create space for permanent left lateral incisor. The teeth erupted spontaneously after the maxillary expansion.
Case 1
A healthy 11-year-old boy, presented to the orthodontic clinic with a chief complaint of non-eruption of upper front tooth after six months of extraction of his milk tooth. The family and medical histories were not significant according to the patient’s parents. No history of dental trauma at younger age to primary predecessors was reported.
Intraoral and Extraoral Examination
Intraoral examination revealed an un-erupted maxillary left lateral incisor tooth (#22). However, the contralateral tooth on right side had already erupted (#12) [Table/Fig-1].
Case 1: Pre-treatment intra oral photographs show: a) right view; b) frontal view; c) left view; d) upper arch; e) lower arch.

The patient was in early mixed dentition with a 2 mm overjet, and a 2.5 mm overbite. The clinical examination showed an Angle Class I Molar relationship on both the sides. On palpation, no bulging was found at the site of left lateral incisor. Adjacent central incisors had no sign of pain during the percussion and there was not enough space for the eruption of the impacted lateral incisor. It is noteworthy that the deciduous lateral incisor had been extracted six months prior to this visit. This was done in view of expected spontaneous eruption of the impacted lateral incisor.
Extra-oral examination revealed slight facial asymmetry with chin deviated to right. The profile was slightly convex with normal vertical facial proportions and obtuse nasolabial angle [Table/Fig-2].
Case 1: Pre-treatment extra oral photographs.

Radiographic Diagnosis
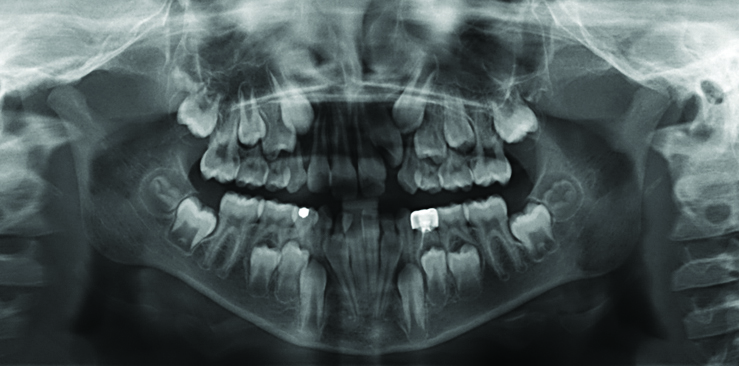
Panoramic radiography revealed the presence of all permanent teeth and showed left permanent lateral incisor impacted. The maxillary primary canine was seen obstructing lateral incisor eruption [Table/Fig-3]. The lateral incisor was rotated and displaced from its eruption path.
Pretreatment panoramic radiograph of case 1 after extraction of tooth 62 and after recall and wait for six months.
Lateral Cephalometric Radiograph was taken. The values were taken using a cephalometric tracing and analysis. The analysis revealed a skeletal Class I relationship [Table/Fig-4,5].
Pre-treatment lateral cephalometric radiograph of case 1.
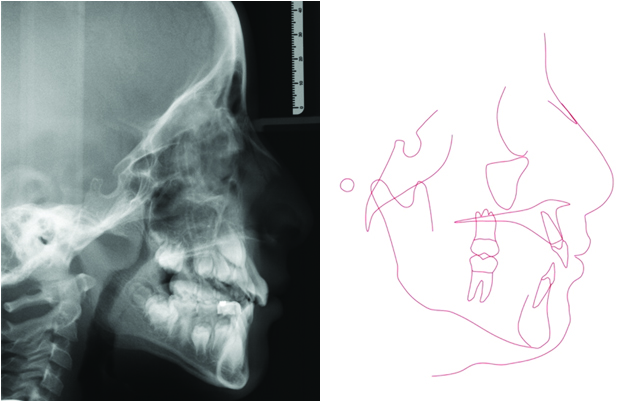
Pre-treatment lateral cephalometric analysis of case 1.
| Skeletal Analysis case 1 |
|---|
| SNA Angle | 80-89° | 67,1° |
| SNB Angle | 75-82° | 63,5° |
| ANB Angle | 2-4° | 3,6° |
| Facial Angle | 87,8±3,6° | 82° |
| Angle of Convexity | 0±5° | 5° |
| Mandibular Plane | 21,9±3,2° | 29° |
| Y-Axis | 59,4±3,8° | 62° |
| Dental Analysis |
| Interincisal Angle | 135,4±5,8° | 133,6° |
| Angle of Anterior Cranial Base to Occlusion | 14° | 35,4° |
| Angle of Anterior Cranial Base to Mandibular | 30° | 46,1° |
| Angle of Axis of 1l to Mandibular Base | 84-92° | 93° |
| Angle of FH to Occlusion Plane | 8-12° | 16° |
Case 2
A nine-year-old healthy girl came to the orthodontic clinic with a chief complaint concerned about delayed eruption of upper front tooth. The family and medical histories were not significant according to the patient’s parents. The dental history did not reveal a traumatic injury to the primary maxillary dentition.
Intra-Oral and Extra-Oral Examination
Intraoral examination showed a mixed dentition and the absence of the maxillary left lateral incisor tooth (#22), although the contra lateral permanent right lateral incisor had already erupted. The patient was in mixed dentition, a 2.5 mm overjet, and a 4 mm overbite. The clinical examination showed an Angle Class I Molar relationship. Mandibular dental midline was displaced 1 mm to the right. On palpation, no bulging was found during the clinical examination at the site of lateral incisor. Adjacent central incisors had no sign of pain during the percussion and there was not enough space for the eruption of the lateral incisor (tooth #22) [Table/Fig-6].
Case 2 pre-treatment intra oral photographs: a) right view; b) frontal view; c) left view; d) upper arch; e) lower arch.

Extraoral examination revealed slight convex, normal vertical facial proportions, obtuse nasolabial angle [Table/Fig-7].
Case 2 pretreatment extra oral photographs.

Radiographic Diagnosis
Panoramic radiograph was taken and showed an impacted left permanent lateral incisor [Table/Fig-8]. The lateral incisor showed a normal eruption path. However, the space between permanent left central incisor and the deciduous canine was not enough to allow the lateral incisor to erupt.
Pre-treatment panoramic radiograph of case 2.

Cephalometric analysis indicated a Class II skeletal pattern with a high mandibular plane angle [Table/Fig-9,10].
Pre-treatment lateral cephalometric radiograph of case 2.
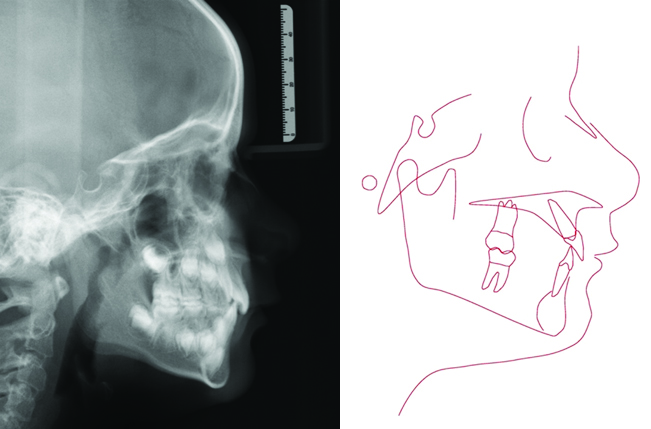
Pre-treatment lateral cephalometric analysis of case 2.
| Skeletal Analysis case 2 |
|---|
| SNA Angle | 80-89° | 79,0° |
| SNB Angle | 75-82° | 74,7° |
| ANB Angle | 2-4° | 4,4° |
| Facial Angle | 87,8±3,6° | 89° |
| Angle of Convexity | 0±5° | 9° |
| Mandibular Plane | 21,9±3,2° | 19° |
| Y-Axis | 59,4±3,8° | 55° |
| Dental Analysis |
| Interincisal Angle | 135,4±5,8° | 142° |
| Angle of Anterior Cranial Base to Occl | 14° | 17,8° |
| Angle of Anterior Cranial Base to Mand | 30° | 32,9° |
| Angle of Axis of 1l to Mand. Base | 84-92° | 90° |
| Angle of FH to Occl. Plane | 8-12° | 4° |
Treatment Objectives
Based on the diagnostic records and clinical examinations, the treatment objectives were to: 1) create enough space for the impacted maxillary lateral incisors to erupt spontaneously by orthopedic maxillary expansion; and 2) guide the maxillary lateral incisors gradually to their appropriate positions to obtain pleasant aesthetics. The treatment of both patients consisted of maxillary expansion to create space for permanent left lateral incisor.
Treatment Alternatives
Both patients and their parents were presented with the following three treatment alternatives other than the interceptive treatment. The other treatment options were: 1) wait for another 6 to 12 months for spontaneous eruption of the impacted lateral incisor; 2) If the teeth didn’t erupt, start orthodontic treatment, gradually implementing complete fixed orthodontic appliances during the eruption of the permanent teeth by creating a space; 3) If the teeth didn’t erupt after orthodontic opening of the space with fixed orthodontic appliance, surgical exposure and traction of the impacted lateral incisors into the proper position. After discussing the possible treatment alternatives and being told about the risks and benefits of each treatment option, the patient’s parents decided on interceptive treatment as it seemed non-harmful to them. Nevertheless, patients in both cases were highly cooperative. Therefore, removable expansion plates with protrusive springs were used [Table/Fig-11].
Photograph pf the expansion plate that was used in case 2.
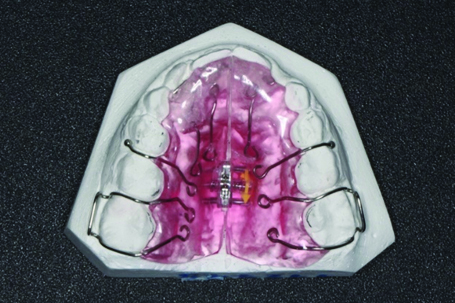
Treatment Progress
The initial treatment was started with expansion for both the cases. Follow-up visits were planned after six weeks in each case. Permanent lateral incisors erupted between 9-11 weeks after expansion. The expansion was continued until enough space was achieved using expansion screws. The patients were instructed to wear the appliance at the night after blocking the screw for one month as a retention period. The treatment plan in each case was designed in a way to provide early expansion so as to allow the impacted lateral incisors into the place. However, in such cases regular follow-up is needed. There are many factors that can influence the treatment plan including the patient’s compliance to wear the removable appliance.
Treatment Results
The objectives of the treatment had been achieved. The maxillary arch seemed to acquire its ideal form after expansion.
In both patients, the impacted maxillary left lateral incisor successfully erupted without any orthodontic traction. Good periodontal health was achieved. However, in case 1, primary canine was exfoliated during expansion period and the space for permanent canine was reduced but as there was not enough space for permanent canine eruption, therefore, follow-up is needed. The patient may need fixed orthodontic therapy at a later stage. In case 2, left lateral incisor erupted in cross bite. Again, this needs follow-up and may need fixed orthodontic therapy at a later stage. However, an adequate space was obtained with satisfactory alignment [Table/Fig-12,13,14 and 15].
Case 1: Post-treatment intra oral photographs: a) right view; b) frontal view; c) left view; d) upper arch; e) lower arch.

Case 1: Post-treatment extra oral photographs.

Case 2: Post treatment intra oral photographs: a) right view; b) frontal view; c) left view; d) upper arch; e) lower arch.

Case 2: Post-treatment extra oral photographs.

After treatment, panoramic radiographs were taken and showed no root resorption or periodontal bone loss in both cases [Table/Fig-16,17].
Post-treatment panoramic radiograph of case 1.
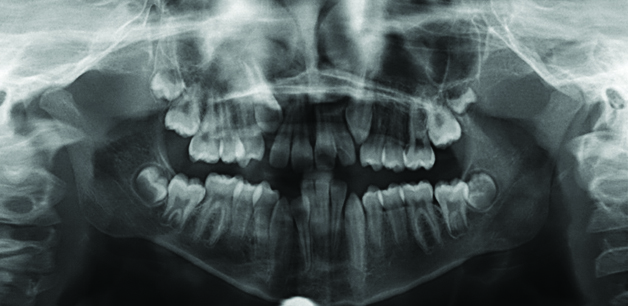
Post-treatment panoramic radiograph of case 2.

Discussion
Impaction defines as a failure of tooth eruption at its normal functional position within normal eruption time [1]. Impaction can directly affect overall treatment planning, and timing of treatment for the orthodontic patient [2]. Impaction in the anterior region, is aesthetically compromising and treatment may be challenging that may usually require orthodontic and/or surgical intervention. Therefore, early diagnosis of impaction is essential to avoid any surgical intervention at a later stage [3]. Several surgical techniques are commonly used to expose maxillary anterior teeth impactions, including an apically positioned flap and closed-eruption technique. Moreover, combined surgical and orthodontic therapy requires long treatment duration, and is associated with increased complications. Those complications may include ankylosis, root resorption, bone loss and periodontal problems. All these issues are usually associated with compromised aesthetic outcomes. Surgery is not required in all patients with impaction because the space-regaining procedure can result in spontaneous eruption of the impacted tooth [4]. The factors that may affect the successful spontaneous eruption of an impacted tooth are numerous; such as, patient age, location and direction of the impacted tooth, the degree of root development, and insufficient space for eruption of the impacted tooth [5].
Impaction of a lateral incisor is a rare phenomenon, and in the literature, there are only a few reports describing this condition [6]. However, the congenital missing of lateral incisor is high with 0.8% in deciduous teeth and 2% for the permanent teeth [7]. The impaction especially in the incisors should be considered for early treatment by the dental practitioner because it may affect the treatment of malocclusion. In many studies, early treatment of eruption disturbance in the incisor area has been recommended [4,8,9]. The possible cause of impaction in both discussed cases was a lack of space. It has been recommended to create space for the tooth during the early mixed dentition and follow-up the progress of spontaneous eruption [3,10,11]. Moreover, spontaneous eruption of lateral incisors after expansion has also been reported [4]. If there were no treatment in both cases, there is still possibility of the lateral incisor to erupt without any intervention; and in that case, the lateral incisor may erupt palatally or bucally to its normal position. However, the risk of impaction is still high in both cases. The treatment was advised since the contralateral incisors had already erupted. Another reason for early treatment was to minimise emotional problem of the child as a result of compromised aesthetics and to create more space. There was also a parental concern that the teeth were congenitally missing and thus, the treatment was started to prevent future complications.
The interceptive treatment of two young patients with impacted maxillary lateral incisors was successfully performed by simple removable expansion plate with a protrusion spring. After expansion and space creation, the path of eruption of impacted lateral incisor was clear and the lateral incisors were expected to erupt spontaneously. No surgical intervention was needed. The prognosis of interceptive treatment depends upon the patient’s cooperation and compliance as well. However, both patients showed high level of cooperation.
A question could be raised that why maxillary expansion was performed without transverse deficiency and whether maxillary expansion was really needed? Our patients did not have a maxillary transverse deficiency. Although, slow maxillary expansion has been proposed as an interceptive treatment; the treatment goal was to create space by expansion for the lateral incisors to erupt and to guide the deviated laterals incisor into their normal position. It has been found that the use of maxillary expansion in early mixed dentition has an increased rate of successful tooth eruption in the maxillary anterior region [4,12].
The panoramic radiograph in case 1 showed that the left lateral permanent incisor was blocked and rotated. This may have been due to the presence of primary lateral incisor that may have blocked the pathway for eruption of the left permanent canine and severely displaced the permanent incisors. The recommendation was to extract the primary lateral incisor before beginning any treatment. This was accomplished six months prior to the visit described above in case 1. After removal of the primary lateral incisor from the path of eruption of impacted lateral incisor, six months’ time was used as a wait for spontaneous eruption. However, the tooth did not erupt. Moreover, intra and extra oral photographs, panoramic and cephalometric radiographs were obtained in the first recall after extraction. Follow-up of maxillary canine is mandatory in case 1 and planning of second phases in both cases will be after the eruption of all permanent teeth.
Conclusion
Early diagnosis of impaction is essential and early intervention with interceptive treatment is advisable to avoid further complications. The lateral incisors erupted spontaneously after 9-11 weeks using expansion with a simple expansion plate. No surgical intervention was required.
Consent: The consent was obtained from the patient for publication of images and case presentation.
[1]. Alqerban A, Jacobs R, Lambrechts P, Loozen G, Willems G, Root resorption of the maxillary lateral incisor caused by impacted canine: a literature reviewClin Oral Investig 2009 13(3):247-55.10.1007/s00784-009-0262-819277728 [Google Scholar] [CrossRef] [PubMed]
[2]. Suri L, Gagari E, Vastardis H, Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature reviewAm J Orthod Dentofacial Orthop 2004 126(4):432-45.10.1016/j.ajodo.2003.10.03115470346 [Google Scholar] [CrossRef] [PubMed]
[3]. Becker A, Early treatment for impacted maxillary incisorsAm J Orthod Dentofacial Orthop 2002 121(6):586-87.10.1067/mod.2002.12417112080308 [Google Scholar] [CrossRef] [PubMed]
[4]. Sant’Anna EF, Marquezan M, Sant’Anna CF, Impacted incisors associated with supernumerary teeth treated with a modified Haas applianceAm J Orthod Dentofacial Orthop 2012 142(6):863-71.10.1016/j.ajodo.2011.07.03023195372 [Google Scholar] [CrossRef] [PubMed]
[5]. Sabuncuoglu FA, Olmez H, Esenlik E, Orthodontic approach to dilacerated central incisor localized horizontally on the anterior nasal spine: a case reportJ Dent Child (Chic) 2011 78(3):168-72. [Google Scholar]
[6]. Tozoglu S, Yolcu U, Tozoglu U, Developmental disturbance of maxillary lateral incisor after traumaDent Traumatol 2007 23(2):85-86.10.1111/j.1600-9657.2006.00380.x17367455 [Google Scholar] [CrossRef] [PubMed]
[7]. Pinho T, Maciel P, Pollmann C, Developmental disturbances associated with agenesis of the permanent maxillary lateral incisorBr Dent J 2009 207(12):E2510.1038/sj.bdj.2009.96119876043 [Google Scholar] [CrossRef] [PubMed]
[8]. Pavoni C, Mucedero M, Paoloni V, Cozza P, Interceptive management for multiple eruption disturbances: a follow-up evaluationEur J Paediatr Dent 2014 15(2 Suppl):191-94. [Google Scholar]
[9]. Brin I, Zilberman Y, Azaz B, The unerupted maxillary central incisor: review of its etiology and treatmentASDC J Dent Child 1982 49(5):352-56. [Google Scholar]
[10]. Manasse RJ, Atsawasuwan P, Conroy C, Treatment of labially impacted upper central incisorsJ Clin Orthod 2015 49(11):701-10. [Google Scholar]
[11]. Morning P, Impacted teeth in relation to odontomasInt J Oral Surg 1980 9(2):81-91.10.1016/S0300-9785(80)80043-3 [Google Scholar] [CrossRef]
[12]. Pavoni C, Franchi L, Lagana G, Cozza P, Radiographic assessment of maxillary incisor position after rapid maxillary expansion in children with clinical signs of eruption disorderJ Orofac Orthop 2013 74(6):468-79.10.1007/s00056-013-0180-x24158584 [Google Scholar] [CrossRef] [PubMed]