Takayasu’s Arteritis and Systemic Lupus Erythematosus-A Rare Coexistence
Savio Dsouza1, Raviraja V Acharya2, Ramachandran Padmakumar3, Kusugodlu Ramamoorthi4, Akshay Kumar5
1 Assistant Professor, Department of Internal Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2 Professor, Department of Internal Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
3 Professor, Department of Internal Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
4 Associate Professor, Department of Internal Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
5 Post Graduate, Department of Internal Medicine, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Savio Dsouza, Sanyo s Villa Salmara Shankarpura Udupi District, Manipal-576104, Karnataka, India.
E-mail: saviokaren@rediffmail.com
Takayasu arteritis, also known as “pulseless disease” is an inflammatory disease characterized by large caliber artery inflammation. Although tuberculosis and syphilis are known to be associated with Takayasu arteritis, it is rarely found in association with Systemic Lupus Erythematosus (SLE). We report a case of 28-year-old Indian female with SLE, on low dose corticosteroids, she presented with hypertension and developed sudden onset of abdominal pain. She was found to have features suggestive of large vessel vasculitis. The patient was treated with one month of high dose corticosteroids and discharged. She was reviewed, once inflammation subsided and underwent procedure of placement of a self-expandable stent. She had improvement of blood pressure immediate post procedure and reduction of abdominal pain and claudication pain after two weeks of follow up. Although, SLE is known to involve small and medium-sized arteries, large vessel involvement and features of Takayasu arteritis are extremely rare, clinically.
Artery inflammation, Corticosteroids, Pulseless disease, Self Expandable stent
Case Report
A 28-year-old unmarried Indian female presented to the hospital with a history of easy fatigability, malar rash and bilateral upper and lower limb claudication pain on exertion for three months. She had a history of photosensitivity since the age of 12 years for which she used topical sunscreen and hypromellose 0.2% eye drops, as prescribed by a local physician. Five years later, the patient had generalized fatigability and increased hair fall and on evaluation was found to be hypothyroid and started on thyroid hormone supplementation. She was diagnosed to have hypertension and was treated with cilnidipine 10 mg twice a day by a local physician.
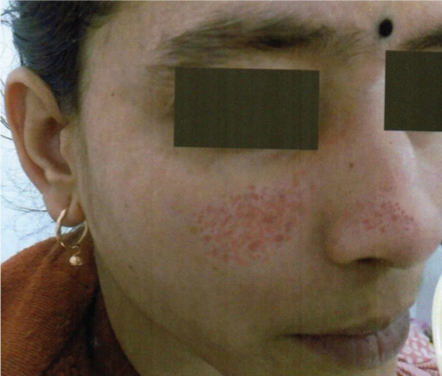
The patient presented to the hospital with complaints of increasing malar rash since past one month that increased on exposure to bright sunlight [Table/Fig-1]. She gave a history of lower limb claudication pain mainly in thigh muscles compared to the upper limb. She had complaints of on and off small joint pains since five years which got relieved with non-steroidal anti-inflammatory drugs, but since past one month, her joint pains were not relieved by non-steroidal anti-inflammatory drugs.
On examination, the patient had a weak pulse on the right upper limb with normal rhythm and pulse rate of 76 beats per minute, blood pressure recorded was 138/90 mmHg in the right upper limb, 160/104 mmHg in left upper limb, 140/94 mmHg in right lower limb and 142/92 mmHg in left lower limb respectively. The general physical examination showed bruit in right carotid. Systemic examination was unremarkable.
Laboratory investigations showed haemoglobin 10.5 gm/dL, Erythrocyte sedimentation rate of 85 mm/hour, Mantoux test negative, serum creatinine 0.8 and globulin 5.06 gm/dL with a positive Coombs test. Urinary protein and microscopic examination were normal. Autoimmune workup showed Anti Nuclear Antibody strongly positive with Anti dsDNA positive with a titer of 140 IU/L and low complement level C3-62 mg/dL (90-180mg/dL), C4 level -8 mg/dL (10-40 mg/dL). Because of difference in blood pressure a carotid Doppler was done which showed mild narrowing of the right subclavian artery. Anticardiolipin and Anti CCP were negative. She was counselled regarding evaluation of secondary causes of hypertension, but due to poor economic condition she refused for further investigations and was discharged from the hospital.
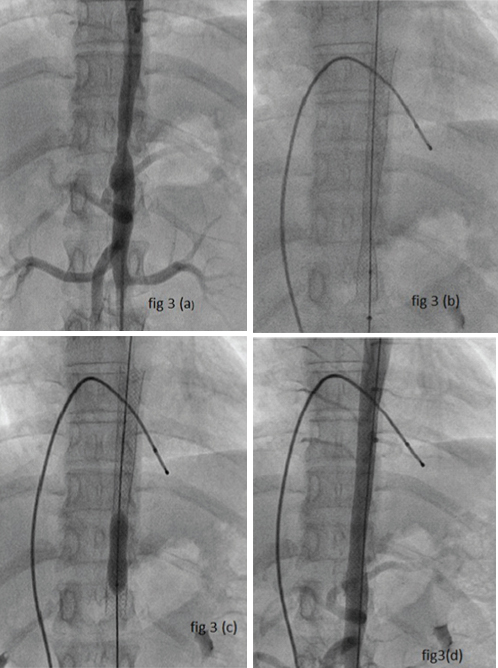
Two months later, the patient presented to emergency with complaints of severe abdominal pain, generalized not associated with reflux symptoms or diarrhoea and severe lower limb claudication pain. Ultrasound examination of the abdomen and pelvis were normal. Upper Gastrointestinal Endoscopy showed no abnormality. In view of persistent abdominal pain CECT abdomen with angiography was done which showed no evidence of mesenteric vasculitis but focal circumferential irregular wall thickening of thoracic aorta for a length of ~1.0 cm causing luminal narrowing of 1.3 cm at the level of T11-T12 suggestive of large vessel occlusive vasculitis Type III Takayasu arteritis [Table/Fig-2a,b]. She was started on prednisolone 1 mg/kg and was planned for stenting after active inflammation settles. After one month of steroid therapy, a self-expandable stent was placed 10 x 94 mm walls after balloon dilatation to the site of stenosis, and the site where the stent was placed was reviewed with angiography which showed dilatation with adequate dye passage [Table/Fig-3a-d]. The patient was better symptomatically with reduction of lower limb claudication and normalization of blood pressure 2 hours post procedure.
Mid Thoracic aorta constriction in CT angiography.

Angiography showing mid thoracic aorta constriction, Self Expandable stent in thoracic aorta, Baloon dilatation of the stented part, Normal Flow post angiography.
Discussion
Takayasu’s arteritis syndrome coexisting with SLE have been described very rarely with only 21 cases available in the literature, of which four had associated antiphospholipid antibody syndrome and last two cases reported in literature were of Sokalski DG et al., and Bandyopadhyay D et al., [1,2]. Takayasu arteritis is a rare, inflammatory, large-vessel vasculitis because it primarily affects the aorta and its primary branches and is usually a granulomatous inflammation which involves all arterial walls and is of unknown aetiology. Females are affected in 80 to 90 percent of cases, with the usual age of between 10 and 40 years (median – 34 years) with prevalence high in Asian continent [3]. Seko Y et al., described Takayasu arteritis as granulomatous infiltration of aortic tissue mainly by killer cells, especially gamma delta T lymphocytes [4]. Absent or diminished pulsation is seen due to arterial wall thickening or thrombosis of main branches of aorta, often asymmetric but collateral formations precludes occlusion in a majority of cases but in untreated cases may lead to occlusion and gangrene [5].
All of the American College of Rheumatology criteria of Takayasu’s arteritis were met in the indexed case which included: (1) Age less than 40 years; (2) Decreased right brachial pulse; (3) blood pressure difference of >10 mm Hg between the two arms; (4) bruit over the carotid artery; (5) Lower limb claudication; (6) angiographic evidence of thoracic aorta arteritis [6]. The present patient had evidence of thoracic aorta arteritis and usually Asians have predominantly Type III Takayasu’s arteritis as described by Hata A et al., also called as ’Middle aortic syndrome” or “Atypical coarctation” [7].
According to Systemic Lupus International Collaborating Clinics, the present case was fulfilling five out of eleven clinical criteria being: (1) Acute cutaneous lupus- malar rash; (2) Photosensitivity; (3) Arthritis; (4) Alopecia; (5) Haemolytic anaemia – coombs positive and four out of six immunological criteria being: (1) ANA – Positivity; (2) Anti dsDNA – Positive; (3) Low complement level; (4) Positive Direct Coombs test making a diagnosis of SLE [8].
Bandyopadhyay D et al., described a similar case of Takayasu’s arteritis which progressed to Systemic Lupus Erythematosus. SLE is associated with vasculitis in 56% of patients mainly cutaneous small vessel vasculitis, and lesions in the aorta are rare occurrence. Vascular involvement is one among the major cause of death and morbidity in patients with SLE. However, vascular involvement is common in males of younger age group [2]. Chakrabarti N et al., described a case of a pregnant female with SLE and diagnosed with Antiphospholipid syndrome (APS) having Takayasu arteritis on presentation in a background of claudication pain and gangrene of lower limbs [9].
Mechanisms involved in Systemic Lupus Erythematosus pathogenesis is due to autoantibodies and the immune complexes they form with antigens leading to defective phagocytosis and triggering B cell activation through B-cell activating factor and by persistently activated T helper cells making B-supporting cytokines such as IL-6 and IL-10. This along with genetic polymorphism, hormonal and environmental factors lead to abnormal activation of the immune system [10]. Takayasu’s arteritis was the first vasculitis associated with infective agent Mycobacterium tuberculosis which triggers the activation of superantigens by cross-reaction with heat shock protein and production of cytotoxic T lymphocytes and leading to chronic granulomatous inflammation [11]. Thus, since T cell-mediated immunity plays a major role in both the diseases it may be an overlap of the immune mechanism which leads to coexistence of both diseases.
Conclusion
Takayasu’s Arteritis and Systemic lupus erythematosus are diseases due to immune dysregulation. Overlap of vasculitic involvement should be considered in any patient with Systemic lupus erythematosus presenting with abdominal pain or claudication of limbs about large vessel involvement which is rare in SLE. Angiographic diagnosis is of utmost necessity in such patients as delay may lead to mesenteric ischemia or limb gangrene.
[1]. Sokalski DG, Copsey Spring TR, Large artery inflammation in systemic lupus erythematosusLupus 2013 22(9):95310.1177/096120331349224123761181 [Google Scholar] [CrossRef] [PubMed]
[2]. Bandyopadhyay D, Ganesan V, Bhar D, Bhowmick D, Takayasu’s arteritis with systemic lupus erythematosus: a rare associationCase Reports in Rheumatology 2015 2015:93419610.1155/2015/93419626167325 [Google Scholar] [CrossRef] [PubMed]
[3]. Lupi-Herrera E, Sánchez-Torres G, Marcushamer J, Takayasu’s arteritis - Clinical study of 107 casesAm Heart J 1977 93(1):9410.1016/S0002-8703(77)80178-6 [Google Scholar] [CrossRef]
[4]. Seko Y, Minota S, Kawasaki A, Shinkai Y, Perforin-secreting killer cell infiltration in Takayasu’s arteritisClin Invest 1994 93(2):75010.1172/JCI1170297906697 [Google Scholar] [CrossRef] [PubMed]
[5]. Yoneda S, Nukada T, Tada K, Imaizumi M, Takano T, Subclavian steal in Takayasu’s arteritisStroke 1977 8(2):26410.1161/01.STR.8.2.26415335 [Google Scholar] [CrossRef] [PubMed]
[6]. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, 2012 Revised International Chapel Hill Consensus Conference Nomenclature of VasculitidesArthritis Rheum 2013 65(1):01-11.10.1002/art.3771523045170 [Google Scholar] [CrossRef] [PubMed]
[7]. Hata A, Noda M, Moriwaki R, Numano F, Angiographic findings of Takayasu arteritis: new classificationInt J Cardiol 1996 54(Suppl):S155-63.10.1016/S0167-5273(96)02813-6 [Google Scholar] [CrossRef]
[8]. Petri M, Orbai AM, Alarcon GS, Gordon C, Merrill JT, Fortin PR, Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosusArthritis Rheum 2012 64(8):2677-86.10.1002/art.3447322553077 [Google Scholar] [CrossRef] [PubMed]
[9]. Chakrabarti N, Chattopadhyay C, Aortoarteritis with systemic lupus erythematosus and secondary antiphospholipid syndromeIndian Dermatology Online Journal 2012 3(1):66-68.10.4103/2229-5178.9348323130270 [Google Scholar] [CrossRef] [PubMed]
[10]. Graham KL, Utz PJ, Sources of autoantigens in systemic lupus erythematosusCurr Opin Rheumatol 2005 17(5):513-17.10.1097/01.bor.0000171215.87993.6b [Google Scholar] [CrossRef]
[11]. Aggarwal A, Chag M, Sinha N, Naik S, Takayasu’s arteritis: role of Mycobacterium tuberculosis and its 65 kDa heat shock proteinInt J Cardiol 1996 55(1):49-55.10.1016/0167-5273(96)02660-5 [Google Scholar] [CrossRef]