Infants have a blood glucose concentration 60 to 70% of the maternal levels at birth and it falls during the initial 24 hours of life. The lowest value is seen in the 3rd hour of life. This is followed by transient rise in blood glucose levels during next 24 hours. This is mainly attributed to the glycogenolysis of hepatic stores, inducing gluconeogenesis, and utilising exogenous nutrients following feeding. Thus, after the first 3-4 hours glucose levels increase and stabilise at mean levels of 65 to 70 mg/dL [1]. Again, dangerously low levels may be encountered at the age of 3-4 days, before stability is achieved. So, transient low blood glucose levels are common in the first few hours after birth as the glucose supply to neonates changes from a continuous transplacental supply from the maternal blood to an intermittent supply obtained from feeds. Persistent or recurrent hypoglycaemia can result in neurologic sequelae like permanent brain damage, cognitive impairment, visual disturbance, occipital lobe epilepsy, and cerebral palsy [2,3]. Symptomatic hyperglycaemia is associated with glycosuria along with osmotic diuresis, intraventricular bleeding, increased risk of neuromuscular sequelae and mental retardation among the survivors [4]. It is therefore essential that all high risk infants must be screened for metabolic disturbances such as hypoglycaemia and hyperglycaemia [5-7]. Their incidence and severity can be reduced by appropriate feeding regimens and early intervention following identification of the metabolic disturbance [4,5]. Hypoglycaemia is defined as blood glucose levels less than 45 mg/dL [1,8]. Hyperglycaemia is defined as blood glucose levels more than 125 mg/dL [1,4]. Cord blood sugar has a mean value of 73 mg/dL and range is 45-96 mg/dL [9]. Infant’s blood has a mean glucose value of 63 mg/dL at 1 to 12 hours and range is 40-97 mg/dL [9].
There is inadequate information in the literature pertaining to the cord blood glucose values as well as value below which irreversible hypoglycaemic injury can occur to the infant. So if any correlation between cord blood glucose and capillary blood glucose values can be found out, the former one can also be used as an early screening tool for hypoglycaemia or hyperglycaemia, thereby reducing infant morbidity. So in general for newborns, low cord blood sugar might be taken as an early indicator for neonatal hypoglycaemia. By routine cord blood glucose estimation, those neonates going for impending hypoglycaemia can be picked up early and timely intervention thereby will prevent neonatal hypoglycaemia and its complications. Also by using cord blood random blood sugar measured by Glucometer Random Blood Sugar (GRBS) early interventions like heel prick; venous blood sampling can be avoided for the neonates. The main objective of the study was to find out the correlation between glucose levels in cord blood and capillary blood of neonates using glucometer soon after birth and to determine the prevalence of hypoglycaemia and hyperglycaemia among the study population.
Materials and Methods
It was a hospital based cross-sectional study conducted at a tertiary care centre at Southern Kerala. The study was approved by institutional ethics committee of the hospital. The study was conducted over a period of 1½ years (January 2015 to July 2016). Written informed consent was taken from the parents of the subjects. All neonates including preterm, intrauterine growth retardation, Small for gestational age, large for gestational age, and twin pregnancies were included in the study and Infants with clinically detected congenital anomalies were excluded from the study.
Data Collection Methods
Blood glucose levels were measured using glucometer (accuchek) with blood from the umbilical cord as well as the capillary blood obtained by heel prick using a stylet under aseptic precautions [10,11]. Both GRBS values were entered in the semi structured questionnaire. Mother details including gestational age, parity, maternal risk factors and baby details like birth weight, date of birth, time of birth, gender, details regarding term/preterm/post term/Small for Gestational Age (SGA), Large for Gestational Age (LGA), Appropriate for Gestational Age (AGA) collected and entered in the semi structured questionnaire.
Statistical Analysis
The data was analysed using SPSS software, version 22. Descriptive measures were calculated. Correlation between the cord blood glucose and capillary blood glucose level assessed by calculating correlation coefficient (Pearson correlation) and other statistical tests used were t-test and chi-square test.
Results
Of the total deliveries in the hospital during the study period, 1100 study subjects satisfying the inclusion criteria were enrolled in the study. Of which 570 (51.8%) babies were males and the remaining 530 (48.2%) were females. Out of the total study subjects 937 (85.2%) babies were of normal birth weight, 125 (11.4%) were of Low Birth Weight (LBW), 33 (3%) were large babies and 5 (0.5%) babies were of Very Low Birth Weight (VLBW). The mean birth weight was 2.985 kg. The minimum birth weight was 0.890 kg and maximum was 4.64 kg. The mean maternal age was 26 years and the maternal age varied from 18 years to 41 years. As far as maternal complications are concerned 143 (13%) mothers had Gestational Diabetes Mellitus (GDM) while Pregnancy Induced Hypertension (PIH) was present in 100 (9.09%) mothers. Mothers of 253 babies (23.0%) suffered from hypothyroidism as well. The mothers of 484 (44%) babies were primigravidae and the remaining 616 (56.0%) were multigravidae. About 932 (84.7%) babies were delivered vaginally while the rest 168 (15.3%) were delivered via caesarean section. The mean cord GRBS in the current study was found to be 79.027±18.470 mg/dL (range 39-175) and the mean capillary GRBS was found to be 66.364±15.5868 mg/dL (range 30-141).
Correlation
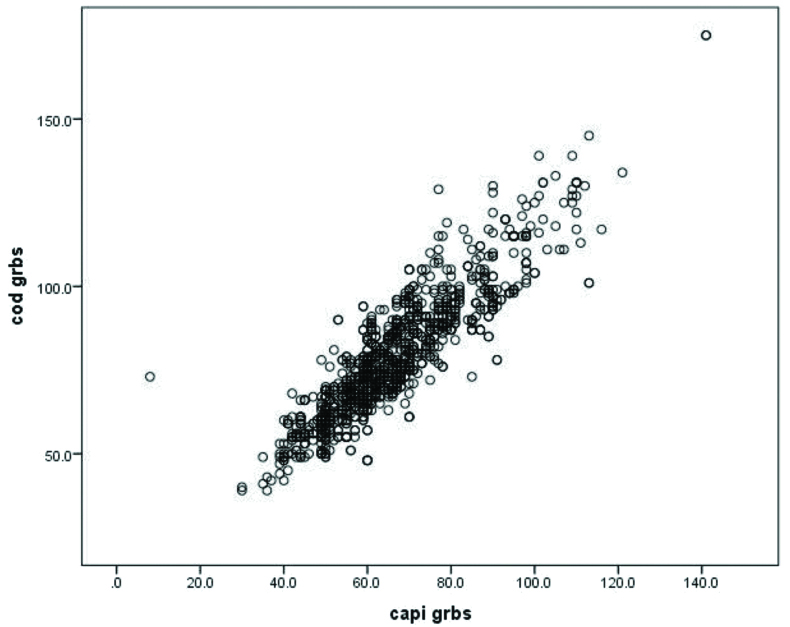
In this study there was a statistically significant (p-value=<.0001) positive correlation (Pearson correlation coefficient r=0.894) between cord GRBS values and capillary GRBS values [Table/Fig-1].
Scatter plot showing correlation between cord blood GRBS and capillary blood GRBS. Cod grbs-Cord GRBS, capi grbs –Capillary GRBS.
Linear Regression
Linear regression done for predicting capillary GRBS from cord GRBS. Capillary GRBS can be predicted by using the equation
Capillary GRBS=α+βx. Where; α is 6.307, β is 0.894 and x is cord GRBS value.
Hypoglycaemia
When capillary blood sugar values were taken into account, the number of babies with hypoglycaemia was 72 (6.5%) [Table/Fig-2]. So the prevalence of hypoglycaemia was 6.5%. The cut-off value for hypoglycaemia was 45 mg/dL [1].
Association between capillary blood sugar and gestational age.
| Gestation | Hypoglycaemia | Normoglycaemia | Total |
|---|
| Preterm | 12 (11%) | 94 (89%) | 106 |
| Term | 60 (6%) | 934 (94%) | 994 |
| Total | 72 | 1028 | 1100 |
Pearson Chi-Square Value 4.373 p-value 0.037, Odd’ S Ratio 1.987 (95% Ci–1.032-3.826)
Hyperglycaemia
When cord blood sugar values were taken into account; the numbers of babies with hyperglycaemia were two (0.2%). So the prevalence of hyperglycaemia was 0.2%. The cut-off value for hyperglycaemia was 125 mg/dL [1,4].
Out of 932 babies delivered vaginally; 55 (6%) of them developed hypoglycaemia and out of 168 babies delivered by LSCS 17 (10%) of them developed hypoglycaemia. Thus according to this study hypoglycaemic events were more common in LSCS babies than those delivered vaginally. Pearson chi-square value 4.140, p-value 0.042.
Among 106 preterm babies 12 (11%) were having hypoglycaemia and 94 (89%) were normoglycaemic while among term babies only 60 (6%) developed hypogycaemia and the rest 934 (94%) were having normal range glucose values.
When cord GRBS was taken into account; one (20%) among VLBW babies had hypoglycaemia, seven (5.6%) among LBW babies had hypoglycaemia and two (0.2%) among normal birth weight babies had hyperglycaemia in this study.
When capillary GRBS was taken into account; two (40%) among VLBW babies, 13 (10.4%) among LBW babies, 41 (4.4%) among normal birth weight babies and 16 (48.5%) among large babies had hypoglycaemia. Pearson Chi-Square Value–114.285 (p-value- <0.0001). Among 116 babies of mothers with gestational diabetes mellitus on insulin, 52 (44.8%) babies had hypoglycaemia which was statistically significant p-value<0.0001. Among babies of mothers with GDM on metformin, 1 (3.8%) developed hypoglycaemia which was statistically not significant. Out of 100 babies of mothers with pregnancy induced hypertention on Alpha methyldopa; 14 (14%) had hypoglycaemia which was statistically significant.
Discussion
The main objective of the study was to find out the correlation between glucose levels in cord blood and capillary blood of neonates using glucometer soon after birth and the secondary objectives were to determine the prevalence of neonatal hypoglycaemia and neonatal hyperglycaemia among the study population based on the capillary blood glucose levels.
The mean cord GRBS in the current study was found to be 79.027±18.470 mg/dL (range 39-175) and the mean capillary GRBS was found to be 66.364±15.5868 mg/dL (range 30-141). As per the study conducted by Acharya PT et al., regarding normal blood chemistry value in cord and capillary blood of term infants mean cord blood sugar was 73 mg/dL (range 45-96) and the mean capillary blood glucose was 63 mg/dL (range 40-97) [9]. The current study values well correlates with the above mentioned study.
In the present study, all the subjects had cord blood glucose values higher than the corresponding capillary blood glucose values. The similar findings were reported in the study done by Trindade C et al., [12].
In this study there was a statistically significant positive correlation between cord GRBS values and capillary GRBS values. With respect to this very high positive correlation, cord blood glucose values can be considered as an efficient initial screening tool to assess the glycaemic status of the newborns especially those at risk, i.e., Infant of diabetic mothers, LGA, SGA, IUGR babies. Inspite of paucity of literature pertaining to the correlation between cord and capillary blood glucose values directly, there are several other studies from different parts of the world which indirectly throw light on the possible high degree of correlation between the parameters under consideration. The study conducted in term infants by Acharya PT et al., reported as early as 1965, cord and capillary blood glucose were measured as part of normal blood chemistry values and their mean values were published [9].
Though a direct study linking cord and capillary blood glucose value is lacking, cord blood glucose values have been used as the basic parameter to compare with several other parameters of newborn. This shed immense light on the reliability of cord blood glucose as a study parameter. The study conducted by Trindade C et al., published in November 2011, aimed at finding correlation between cord blood glucose and maternal glucose levels [12]. The above mentioned study states that the cord blood glucose values were higher than the corresponding blood sugar values (p-value=0.001).
It is found that the capillary GRBS can be predicted from the measured cord blood sugar values with the equation Capillary GRBS=α+β x where α is 6.307, β is 0.894 and x is cord GRBS value, For example: if the cord blood glucose is obtained as 80 mg/dL, the predicted capillary GRBS value=6.307+.894×80=77.827 mg/dL.
This proves that cord blood glucose value can be used as an ideal parameter for predicting the corresponding capillary GRBS values. So in general, for newborns, low cord blood sugar might be taken as an early indicator for neonatal hypoglycaemia.
Hypoglycaemia
One of the secondary objectives of the study was to determine the prevalence of hypoglycaemia in the study population. When capillary blood sugar values were taken into account, the number of babies with hypoglycaemia was found to be 72 (6.5%). The cut-off value for hypoglycaemia in this study was taken as 45 mg/dL.
As per the study conducted by Sasidharan CK et al., in southern Kerala, the prevalence of neonatal hypoglycaemia is 4.1% [13]. Yet another study, conducted by Singhal PK et al., the prevalence was determined to be 4.8% [14]. Prevalence from the above mentioned studies are comparable with the results of the present study.
Hyperglycaemia
Hyperglycaemia, on the other hand, was detected in two of the study population accounting for 0.2%. As per international and national literature, incidence is very less as compared to hypoglycaemia; reason being suggested that it is a common feature of VLBW babies. In the current study setup only 0.5% of the study population has VLBW [15].
Limitation
In the current study GRBS measurement using glucometer has been resorted to as the technique for cord and capillary blood glucose estimation. However, it is well accepted that the gold standard for glucose measurement was the random blood glucose values.
The cord and capillary blood glucose values were dependent on a number of factors; duration of labour was significant among them. But since the study had been conducted in a tertiary care centre where usually referred cases were higher. Hence, there was no precise method to know the exact time that has elapsed after onset of labour. Glucometer related troubles: cost of the glucometer strips was around Rs 40 per strip. The (semi) invasive nature of the procedure (heel prick) also should be considered.
Conclusion
In this study a positive correlation between cord GRBS values and capillary GRBS values was found out. Capillary GRBS can be predicted by using the positive predictive equation; which again is ample evidence that the cord blood glucose value measured with a glucometer soon after birth can be used as an effective predictor of the corresponding capillary blood glucose values.
Both hypoglycaemia and hyperglycaemia can be detected and early intervention can be done. The measurement of blood glucose values in the immediate post natal period could very effectively and precisely throw light on the glycaemic status of the baby, thereby helping health care providers an opportunity to reduce both morbidity and mortality of neonates. This study recommends universal measurement of cord blood glucose values to get hindsight about the glycaemic status preferably all newborns so as to avoid preventable complications in babies especially at risk.