Diabetes Mellitus is a chronic metabolic disorder. It is a complex disease characterised by chronic hyperglycaemia, metabolic abnormalities resulting in long-term macrovascular and microvascular complications [1]. DM is a major health problem all over the world (pandemic) with high morbidity and mortality rate [1]. According to the World Health Organisation (WHO) 2012 statistics, 1 in 10 adults suffer from diabetes [1]. The incidence of Type 2 DM is increasing and it will get doubled in the period of 30 years [2].
Diabetes is a slow onset disorder, resulting from interactions between environmental factors and polygenetic inheritance. Majority of diabetic patients suffer from complications. These complications are mainly due to hyperglycaemia which can lead to increased morbidity and mortality owing to poor glycometabolic control. Glycometabolic control can be monitored by Fasting Blood Glucose (FBG), and Haemoglobin A1c (HbA1c). HbA1c is a useful marker to determine mean blood glucose levels over the period of three months [3]. Another cofactor responsible for diabetic complications is altered platelet morphology, increased platelet dysfunction and reactivity which results in the prothrombotic state of DM leading to vascular complications which in turn increases morbidity and mortality in diabetic patients [2,4]. Platelets in DM are hyperactive and releases more granules which cause the increase in platelet turnover, which inturn results in larger platelets and these larger platelets, are more enzymatically and metabolically active and have a tendency to form clots leading to both macro and microvascular complications [4,5]. Platelet indices are a measure of the platelet function and activation. Therefore, increased platelet indices may be allied with increased thrombogenic potential. Platelet indices can be measured by automated haematology analysers as a routine haematological procedure [1]. Expected Mean Platelet Volume (MPV) value in our lab was between: 7.4-10.4 fL, Platelet Distribution Width (PDW): 9-14 fL, Platelet Large Cell Ratio (PLCR): 15-35% [6,7]. MPV is indicator of the average size, hence activity of platelets. It is calculated by dividing the Platelet Crit (PCT) by platelet count. Variability in the platelet size can be measured by PDW. It is measurement by calculating the width of the platelet histogram at the 20% height level. Increased PDW means platelet size variation and it is elevated earliest than other platelet parameters in diseases affecting platelets. PLCR indicate the percentage of large platelets with a volume >12 fL. An increase in PLCR may be an indicator of giant platelet [6]. Both PDW and PLCR are calculated by platelet histogram generated by automated haematology analyser, so they are not influenced by the average MPV. These tests are simple, inexpensive, and easily available in routine laboratories and are done nearly for every patient coming to the hospital via a routine Complete Blood Count (CBC) test. Therefore, for early diagnosis of thromboembolic diabetic complications which are attributed to platelet activation, can be measured by platelet indices, proving them to be potentially useful marker [2].
The present study aimed to evaluate the variation in platelet indices among patients with DM, to determine the association between platelet indices and complications due to diabetes and also estimation of the correlation between platelet indices with glycaemic control (HbA1c), FBG and duration of diabetes, so as to know whether platelet indices can be of any help in the early diagnosis of thromboembolic events in DM which would reduce the morbidity and healthcare costs in patients with diabetes.
Materials and Methods
The present study was prospective and cross/sectional study was conducted in the Department of Pathology, Jawaharlal Nehru Medical College, Belgaum over a period of one year from January 2013 to December 2013 on 210 patients who were suffering from Type 2 DM and attended Outpatient Department (OPD). Informed consent was obtained from all individual participants included in the study and approval from the Institutional Ethic Committee was also taken (MC/DOME/895).
Inclusion criteria: Patients who were suffering from Type 2 DM and attending OPD.
Exclusion criteria: Patients with anaemia (Hb <11 g/dL for females and Hb <12 g/dL for males), thrombocytopenia (platelet count <1, 50,000/μL), thrombocytosis (platelet count >4,50,000/μL) and malignancy were excluded from the study, so as to rule out any other causes of reactive platelets. Even, patients on antiplatelet drugs were excluded. Hypertensive patients who later develop DM were also excluded so as to avoid hypertension as the confounding factor in the study.
All diabetic patients underwent a complete clinical evaluation with specific reference to any diabetic complication as well as any drug intake. After taking the detailed history and clinical examination of the patients, 2 mL blood was collected in Dipotassium Ethylenediaminetetraacetic Acid (EDTA) tube and was processed in automated haematology analyser (Lab life D5 Supreme) within one hour of the collection to minimise variation due to sample ageing. Many literatures have suggested that platelet indices can be measured accurately by both EDTA and citrate tubes, if the analysis is performed within one hour of sampling [6].
The sample for FBS, HBA1c, lipid profile was collected in sodium fluoride, EDTA and plain vacutainer respectively. The sample was then maintained at room temperature. The estimation of FBS and lipid profile was carried out in autoanalyser (Siemens, Dimension Rx L Max). HBA1c was estimated by high performance liquid chromatography method (Bio-Rad D-10).
After analysing variation in platelet indices, all 210 diabetic patients were divided into two groups, Group A i.e., patients without diabetic complications (157, 74.76%) and Group B i.e., patients with diabetic complications (53, 25.24%). Than all 210 diabetic patients were again divided on the basis of HBA1c levels, Group I was patients whose HBA1c level is <6.5% (25,17.14%) and Group II was. patients whose HBA1c level is >6.5% (185,82.86%). As, the latest cut-off criteria for diagnosis of diabetes according to American Diabetes Association (ADA) 2012 is >6.5%.
Statistical Analysis
Statistical analysis was performed using SPSS version 16.0. Qualitative data were described as number and percentage. Quantitative data were described as range (maximum and minimum), mean and standard deviation. Comparison between different group regarding categorical variable was performed using the student’s t-test and Pearson’s correlation test (r value as the coefficient) were used. Probability (p-value <0.05 was considered significant.
Normal Range
MPV: 7.4-10.4 fL, Platelet Distribution Width (PDW): 9-14 fL, Platelet Large Cell Ratio (PLCR): 15-35%, FBS: <100 mg/dL, HbA1c: <6.5% [6,7]. Normal lipid profile values are, for total cholesterol (TC): <200 mg/dL, Low Density Lipid (LDL): <99 mg/dL, High Density Lipid (HDL): >60 mg/dL and Triglyceride (TG): <150 mg/dL.
Results
The present prospective study was conducted over a period of one year. Out of 210 patients, 146 (69.2%) were males and 64 (30.8%) were females. The majority of patients were in age group of 40-59 years (mean age of the study group was 57.7±10.95 years and ranged between 29-82 years) [Table/Fig-1]. The majority of patients were suffering from diabetes for 1-5 years (40%) with average duration of diabetes 5±4.3 years [Table/Fig-2].
Age distribution of the patients.
| Age (years) | No. of patients | % of Patients |
|---|
| 20-39 | 12 | 5.7 |
| 40-59 | 102 | 48.6 |
| 60-79 | 90 | 42.9 |
| 80-99 | 6 | 2.8 |
Duration of DM in patients.
| Duration | No. of the Patients | % of Patients |
|---|
| New | 38 | 18.10 |
| 1-5 years | 84 | 40 |
| 6-10 years | 67 | 31.90 |
| >10 years | 21 | 10 |
The majority of patients (62.86%) had FBS in range of 100-200 mg/dL (mean FBS: 160±78.3 mg/dL and range of FBS: 66-690 mg/dL) [Table/Fig-3a]. Most of the patients had bad glycaemic control i.e., HbA1c >6.5% (82.86%) (mean HbA1c: 8.68±1.84%, range: 5% to 17.2%) [Table/Fig-3b).
Distribution of the FBS, HbA1c, Total Cholesterol (TC), Triglyceride (TG), HDL and LDL in diabetic patients.
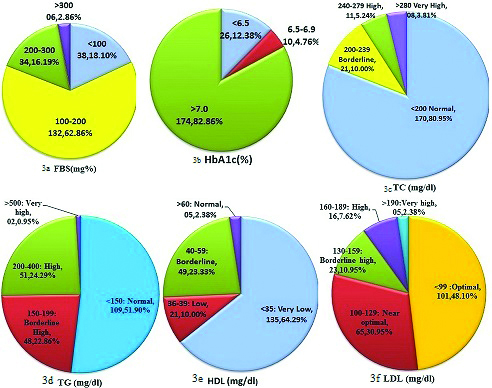
The majority of the patients had normal total cholesterol (80.95%) (mean was in normal range=164.6±65.32 mg/dL, range: 4-726.8 mg/dL) [Table/Fig-3c]. About half of the cases had normal triglyceride levels (51.9%), however the mean triglyceride level was in borderline high range: 159.8±87.71 mg/dL (range: 37-652 mg/dL) [Table/Fig-3d]. The majority of the patients had normal LDL levels (48.1%) (mean LDL was in near optimal range: 105.4±53.77 mg/dL, range was 17-634.2 mg/dL [Table/Fig-3e]. Most of the patients had low HDL (64.29%) (mean HDL level was in very low range: 32.9±10.16 mg/dL, the range: 10-72 mg/dL) [Table/Fig-3f].
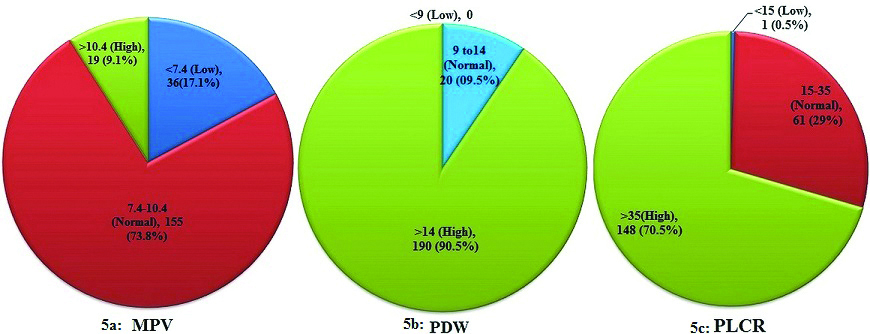
Mean MPV of the study group was 8.6±1.24 fL, and range was 5.2-11.1 fL. Mean PDW was 17.9±3.75 fL and range was 11.6-35.6 fL. Mean PLCR was 35.5±7.88% and range was 12.9-49.4% [Table/Fig-4]. A 9.1% patients had high MPV i.e., >10.4 fL, 90.5% patients had high PDW (>14 fL) and the majority of the patients i.e., 70.5% had high PLCR (>35%) [Table/Fig-5a-c].
Platelet Indices in DM patients (mean±standard deviation, median, range).
| Parameter | Mean±SD | Median | Range |
|---|
| Haemoglobin | 12.8±1.16 | 12.6 | 11-18 |
| Platelet count (103/μL) | 257±75.6 | 248 | 197-311 |
| MPV (fL) | 8.6±1.24 | 8.6 | 5.2-11.1 |
| PDW (fL) | 17.9±3.75 | 16.9 | 11.6-35.6 |
| PLCR (%) | 35.5±7.88 | 37.5 | 12.9-49.4 |
Variation of Platelet Indices in DM patients number, percentage.
Out of 210 diabetic patients, 157 patients (74.76%) were suffering from diabetic complications and 53 diabetic patients (25.24%) were without any diabetic complications. Majority of diabetic patients in the study were suffering from cardiovascular complications (44.76%). The patients suffering from nephropathy had highest value of MPV, PDW, PLCR and HbA1c [Table/Fig-6].
Various complications developed in patients suffering from diabetes mellitus. (mean±standard deviation).
| Complication | No. (%) of the Patients | MPV | PDW | PLCR | HbA1c |
|---|
| Absent | 53 (25.24) | 7.4±1.19 | 11.8±2.06 | 25.8±6.60 | 6.45 |
| Cardiovascular | 94 (44.76) | 8.9±0.96 | 18.7±3.43 | 38.2±5.37 | 7.65 |
| Diabetic foot | 47 (22.38) | 9±1.03 | 19.6±3.96 | 39.8±3.81 | 8.6 |
| Retinopathy | 05 (2.38) | 8.8±0.84 | 18.2±1.73 | 38.1±2.19 | 8.9 |
| Nephropathy | 05 (2.38) | 9.8±0.65 | 22.5±2.91 | 42.7±2.31 | 11.6 |
| Cerebrovascular | 02 (0.95) | 9.4±0.77 | 17.4±1.69 | 38.7±0.84 | 9.15 |
| Multiple complication | 04 (1.91) | 9±1.60 | 19.1±4.51 | 35.2±12.84 | 10.6 |
| TOTAL | 210 (100) | | | | |
On comparing various parameters between patients suffering from diabetic complications and diabetic patients without any diabetic complications, it was observed that all the platelet indices (MPV, PDW and PLCR) were higher in patients with complications as compared with patients without complications and these differences were statistically significant. Even sex ratios, duration of diabetes, FBS, HbA1c, lipid profile were higher in patients with complication than patients without complications with statistically significant p-value (p<0.05). However, there was no significant difference between the groups in relation to age, haemoglobin and platelet count. Platelet count was lower in patients with complication than in patients with uncomplicated diabetes but it was statistically not significant [Table/Fig-7].
Comparison of variables between patients with and without complications due to diabetes mellitus. (mean±standard deviation, student t-test).
| A | B | |
|---|
| Variables | Complications Absent | Complications Present | t-test | p-value |
|---|
| Number of Patients | 53 | 157 | | |
| Age | 58.1±11.09 | 57.5±10.94 | 0.288 | 0.744 |
| Sex | 30 (56.6%) (M) | 116 (73.9%) | 5.585 | 0.018* |
| 23 (43.4%) (F) | 41 (26.1%) |
| M:F ratio | 1.30 | 2.82 |
| Duration | 3.1±4.72 | 5.6±3.96 | 3.846 | <0.001* |
| Fasting Blood Glucose | 128.7±48.83 | 170.4±83.46 | 3.445 | 0.001* |
| HbA1c status | 7.8±2.63 | 8.9±1.37 | 4.010 | <0.001* |
| Total Cholesterol | 137.9±44.39 | 173.7±66.80 | 3.550 | <0.001* |
| HDL | 88.3±34.69 | 111.2±57.78 | 2.719 | 0.007* |
| LDL | 41.2±10.82 | 30.2±8.28 | 7.706 | <0.001* |
| TG | 112.9±40.78 | 175.7±93.55 | 4.734 | <0.001* |
| Haemoglobin | 12.8±1.19 | 12.9±1.15 | 0.283 | 0.777 |
| Platelet Count | 265.4±71.84 | 254.4±76.58 | 0.908 | 0.364 |
| MPV | 7.4±1.19 | 8.9±0.99 | 9.420 | <0.001* |
| PDW | 14.8±2.06 | 19±3.60 | 8.057. | <0.001* |
| PLCR | 25.8±6.61 | 38.7±5.12 | 14.711 | <0.001* |
*Statistically significant (p<0.05); M: Male; F: Female
The study group was also compared based on HbA1c. Out of 210 patients suffering from type 2 DM, 185 patients (88.09%) had HbA1c >6.5%. All the platelet indices and lipid profile were significantly increased in patients with HbA1c >6.5% than in patients with HbA1c <6.5% [Table/Fig-8].
Comparison of variables between patients with HbA1c <6.5% and patients with HbA1c >6.5%. (mean±standard deviation, student t-test)
| I | II | |
|---|
| Variables | HbA1C <6.5 | HbA1C >6.5 | t test | p-value |
|---|
| Number of Patients | 25 | 185 | | |
| Cholesterol | 130.6±48.87 | 169.3±66.9 | 2.822 | 0.005* |
| LDL | 84.5±40.11 | 108.2±66.9 | 2.089 | 0.038* |
| HDL | 42.9±12.81 | 31.6±8.98 | 5.592 | <0.001* |
| TG | 107.6±33.97 | 166±90.37 | 3.245 | 0.001* |
| MPV | 6.6±0.80 | 8.8±1.08 | 9.8886 | <0.001* |
| PDW | 14.1±2.09 | 18.5±1.05 | 5.983 | <0.001* |
| PLCR | 24.6±6.77 | 36.9±6.80 | 8.546 | <0.001* |
*Statistically significant (p<0.05)
Authors found positive correlation between all platelet indices with duration, FBS, HbA1c, lipid profile and diabetic complications which was also statistically significant. However, authors also found negative correlation between all platelet indices with HDL and platelet count but for platelet count, it was not statistically significant [Table/Fig-9].
Correlation of Platelet Indices with other parameters (student t-test, pearson correlation test).
| | Duration | FBS | HbA1c | Total Cholesterol | LDL | HDL | TG | TLC | Platelet count | Complication |
|---|
| MPV | r-value | 0.488 | 0.397 | 0.297 | 0.292 | 0.246 | -0.428 | 0.312 | 0.238 | -0.078 | 0.567 |
| p-value | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | <0.001* | 0.262 | <0.001* |
| PDW | r-value | 0.360 | 0.136 | 0.204 | 0.247 | 0.220 | -0.331 | 0.316 | 0.124 | -0.062 | 0.505 |
| p-value | <0.001* | <0.001* | 0.001* | <0.001* | <0.001* | <0.001* | <0.001* | 0.073* | 0.372 | <0.001* |
| PLCR | r-value | 0.415 | 0.289 | 0.217 | 0.267 | 0.217 | -0.443 | 0.343 | 0.174 | -0.039 | 0.725 |
| p-value | <0.001* | <0.001* | 0.002* | <0.001* | 0.002* | <0.001* | <0.001* | 0.011* | 0.573 | <0.001* |
*Statistically significant (p<0.05), r value: pearson correlation coefficient
Discussion
DM is the most common endocrine disorder. It is characterised by metabolic abnormalities involving multi-organs such as heart, nerves, eyes, CNS, kidneys, gastrointestinal tract and blood vessels, leading to long-term complications owing to increased mortality and morbidity. India is a country with the largest population of people living with diabetes and has become the capital of diabetes in recent years, with every 5th person suffering from DM [8-11].
It is a prothrombic state, which is accompanied by inflammation and accelerated atherosclerosis [12]. Even through aetiology of DM is multifactorial, platelet, especially large platelets play an important role in the pathogenesis of diabetes and the development of complications due to DM [13]. Main reasons for abnormal platelet functions in DM are immature, larger platelets and activated platelets due to the metabolic milieu in DM or due to vascular damage. All these factors are interlinked [13].
As a consequence of platelet dysfunction in diabetic patients, there are enhanced platelets hyperaggregability and platelet activation causing circulating platelets to release more granules which causes reduce survival of platelets and hence releasing larger platelets from bone marrow. This is because of increased ploidy and activation of megakaryocytes. These larger and younger platelets have large volume and they are functionally active because they have increased surface marker on their surface (GPIIb/IIIa, GPIb-IX, GPIa/IIa and CD62), increased thromboxane synthesising capacity and various platelet-specific proteins [13]. Enhanced platelet aggregation and activation has been implicated in the development of microvascular and macrovascular complication [13].
These larger platelets can be measured by platelet indices namely MPV, PDW and PLCR [2]. Thereby, monitoring of platelet function in diabetic patient via platelet indices can help in curbing diabetic related morbidity and mortality.
In the present study, mean value of platelet indices i.e., MPV (8.6±1.24 fL) was in normal range, PDW (17.9±3.75 fL) was high and PLCR (35.5±7.88%) was slightly high. MPV in diabetic patients was in concordance with other studies done by Kodiatte TA et al., (8.29±0.735 fL), Gupta AV et al., (8.96±1.93 fL), Sharpe PC (8.9±0.07 fL) and Demintun R et al., (8.7±0.8 fL) [2,14-16]. When authors analysed the variation of platelet indices, found that the majority of diabetic patients had higher PDW, PLCR value, however for MPV, majority fell in the normal range. Only 9.04% patients had MPV higher than upper limit of normal range. The reason could be that PDW and PLCR are independent of platelet count whereas MPV is dependent on platelet count or plateletcrit and is calculated by histogram. Till date, no study had described the variation of abnormal platelet indices in DM.
Abnormal metabolic milieu (hyperglycaemia, dyslipidemia i.e., hypertriglyceridemia with low HDL and insulin resistance) is usually witnessed in DM. It induces a vicious circle of events in the vascular wall resulting in endothelial dysfunction, platelet hyperactivity and increased inflammation in vessel wall. Both hyperglycaemia as well as hypertriglyceridemia the platelet reactivity either directly or through glycation of plasma protein [12]. Whereas, low HDL causes endothelial dysfunction which increase atherothrombotic risk [5]. Hyperglycaemia induces an overproduction of superoxide which activates protein kinase C and Nuclear Factor kB (NF-kB) and blocks Endothelial Nitric Oxide Synthase (eNOS) activation, consequently resulting in increased production of reactive oxygen ions and hence causing DNA damage. Transcription factors such as NF-kB also induce inflammatory gene expression resulting in augmented expression of cell adhesion molecules and increased production of inflammatory cytokines as well as leukocyte-attracting chemokines. These changes in endothelial cells as well in monocytes lead to increased production of tissue factor, the major procoagulant found in atherosclerotic plaques, along with platelet activation and aggregation and alterations in coagulation and fibrinolytic factors [13]. In the present study mean FBS, mean HBA1c with mean triglyceride was high and mean HDL was low. There was also a statistical correlation between platelet indices and lipid profile in the study.
In our study, the majority of patients were suffering from complication i.e., 74.6%. Study done by Jindal S et al., the percentage of patients suffering from complications was 66.67% and in another study by Kodiatte TA et al., it was 62.4% [2,12]. Cardiovascular complications are the most common cause of mortality and morbidity among people with diabetes. It can account for more than 50% of deaths due to diabetes [8,9,17]. Even in the present study, authors found that majority of the diabetic patients were suffering from cardiovascular disease (44.76%), however, the highest platelet indices were found in patients having diabetic related nephropathy.
On comparing platelet indices between patients without complications and with complications, they were higher in the latter and the difference between the two groups was statistically significant (p-value for MPV, PDW and PLCR were <0.001). This finding was in concordance with the previous studies [2,7,12,15,18-20]. This suggested a role for the enhanced platelet activity in the pathogenesis of vascular complications. In diabetic patients as discussed earlier, platelet survival is reduced resulting in increased platelet turnover which reflects increased thrombopoiesis. Platelet activation also resulted from an altered response to agonists, enhanced glycoprotein receptors expression, increased fibrinogen binding and decreased membrane fluidity, increase in adhensive proteins on the platelet surface [4,16,17,18,21]. Authors also found mean platelet count was decreased in diabetic patients with complication as compared to patient without complication. However, platelet count did not show any statistical significance on diabetic complication. This suggested that platelet count is dependent on various factors like low platelet survival and more turnover of platelet in diabetic complication. Mean duration of the diabetes was higher in patients with complications than in patients with uncomplicated diabetes. This difference was statistically significant with the p-value of <0.001. The risk of chronic complications increases with duration of DM [2]. Patients with complications had deranged lipid profile than patients without complications, p-value between these groups was significant (p-value of total cholesterol, LDL, TG was <0.001 and for HDL was 0.007). Hyperlipidemia is also one of the causes of platelet activation in patients with diabetes [4]. The metabolic alterations of platelet milieu which leads to increased sensitivity to agonist are impaired calcium homeostasis, activation of protein kinase C, decreased platelet derived nitric acid and increased production of superoxide anion [2].
Both FBS and HbA1c were higher in patients with complications due to DM than patients without complications and p-value for both FBS and HbA1c was statistically significant (p-value for FBS being 0.001 and for HbA1c being<0.001). When the platelet indices were compared with glycaemic control, authors found that patients with HbA1c >6.5% had higher platelet indices (MPV, PDW and PLCR) than patients with HbA1c <6.5%. This difference between the groups was statistically significant (p-value for all the three platelet indices was <0.001), and the findings were similar to that of Kodiatte TA et al., and Demirtunc R et al., [2,16]. The reason for poor glycaemic control in the present study could be because of poor dietary practices and lack of knowledge about the glycaemic control among patients suffering from DM [1,17]. Poor glycaemic control in diabetic patients results in hyperactivity of platelets directly as well as through glycation of platelet membrane proteins which cause the early destruction of platelets and increased thrombopoiesis, which in turn result in higher platelet indices in patients with complications. Enhanced platelet activity and platelet aggregation have been associated with the development of microvascular and macrovascular complications [2]. Authors also found that the platelet count had no association but had an inverse relation with all platelet indices, which had been also concluded with the results described in other studies [21]. Platelet indices were also associated with duration, lipid profile, glycaemic status as well as with diabetic complication. This finding was in similar to other study done by Ates O et al., where MPV was positively correlating with the degree of retinopathy but in contrast to the study done by Kodiatte TA et al., where they found no association between MPV and duration of diabetes and presence of complication [2,7].
Limitation
The limitations in the present study were the inability to follow up the patients, to know the prognostic value of present findings and conducting platelet function tests on the sample to substantiate present findings. However, these factors constitute a modest part of the study.
Conclusion
The present study indicated that the platelets in DM are larger and more active and they have higher thrombogenic potential and their platelet indices are increased. The larger platelets are one of the important risk factor for the development of atherosclerosis and are associated with vascular complication. Authors also found increased platelet indices which are directly proportion to diabetic complication and glycaemic control. Diabetic patients with higher platelet indices can easily be recognised during routine haematological analysis and possibly be benefited from anti platelet treatment which can prevent disease progression. Hence, platelet indices are readily available tool to assess the control of DM, progression of disease as well as thromboembolic events.
*Statistically significant (p<0.05); M: Male; F: Female
*Statistically significant (p<0.05)
*Statistically significant (p<0.05), r value: pearson correlation coefficient