An inguinal hernia is herniation of loop of the intestine in the inguinal canal and repair of such herniation is one of the commonest surgeries. Repair/surgery of inguinal hernia can be performed under General Anaesthesia (GA) or Regional Anaesthesia (RA) [1]. RA technique includes spinal, epidural or nerve blocks like hernia block (Ilio-hypogastric-Ilioinguinal-Lower intercostals nerves T11 and T12 block) or paravertebral block. Various comorbidities like cardiac, renal, cerebral, endocrine, respiratory etc., may accompany the situation and further complicate anaesthetic management. Treatment of postoperative pain is also an issue in such high-risk patients [2].
Central neuraxial blockade i.e., SA is a very convenient and the most preferred method for inguinal hernia repair. It can lead to hypotension and bradycardia, depending upon sympathetic block, preoperative cardiac condition and intravascular volume of the patients. PVB is considered safer than the central neuraxial blocks in light of reduced haemodynamic alterations. Hypotension, bradycardia and other effects due to sympathetic blockade are not seen in PVB [2]. Patients who are taking anticoagulants, in whom central neuraxial blockade is contraindicated, PVB is considered a viable alternative to practice [3]. Disadvantages are longer procedural time, lack of adequate skills, possibility of failure, inadvertent epidural spread or contralateral spread of the drugs and pneumothorax or injury to lungs when performing PVB at higher level [4-6]. Other complications include direct trauma to nerves, intraneural injections, abdominal visceral damage, retroperitoneal hematoma, psoas abscess, epidural spread and haemo-thorax [7]. Peripheral Nerve Locator or Ultrasonography (USG) increases the success rate of block, reduces possibility of complications [8]. A comparative study was needed to evaluate efficacy of PVB over SA in unilateral uncomplicated inguinal hernia surgery. The aim of this study was to compare onset of sensory block, duration of analgesia, procedure time, intraoperative and postoperative haemodynamic changes as well as complications in SA and PVB.
Materials and Methods
This study is a prospective comparative study. Fifty male patients, age between 18 to 60 years with different occupational background and ASA status I and II undergoing elective unilateral uncomplicated inguinal hernia surgery at BJ Medical College and Civil Hospital Ahmedabad, Gujarat, India, were included in study from January 2014 to December 2014. Prior permission of Institutional Ethics and Review Committee was obtained and necessary guidelines were followed. Pre-anaesthetic examination was done in all patients.
Exclusion Criteria
Patient’s refusal, obese patients with BMI >35, ASA physical status >III, history of bleeding and coagulation disorder, allergic to local anaesthetic agents, infection at local site, head injury and increased intracranial pressure, neurological disease or psychotic disorder, severe anaemia, haemodynamic instability, cardiac or hepatic or renal disease.
Patients were randomly allocated to Group PVB and Group SA. Randomisation was done by computer-generated random numbers and unpaired random allocation to SA and PVB groups. Informed and written consent was taken from all patients after preoperative assessment. Routine investigations including complete blood count, renal and liver function tests, X-ray chest, ECG and serum electrolytes were noted. On operation table, 20 gauge intravenous lines were secured. Monitors applied were ECG, Non-Invasive BP (NIBP), Oxygen Saturation probe (SpO2). Vitals were recorded baseline, after premedication with inj. midazolam 0.02 mg/kg IV and inj. Ondansetron 0.08 mg/kg IV, immediate after anaesthesia and every five minutes for initial 15 minutes, thereafter every 15 minutes till the end of surgery. In SA group preloading was done with ringer lactate 500 mL.
Paravertebral Block
Sitting position was used for both PVB and SA. Line connecting the iliac crests was drawn with identifying L4 spine and then each spine from T10 to L4 was marked. Entry points were marked 3 cm lateral to the cephalad border of the T10, T11 and L1 spine. This plane usually corresponds to the transverse process of the vertebra lying below the marked vertebra. Under all aseptic and antiseptic precautions, painting were done and drape applied. Skin wheal was raised with inj. lignocaine hydrochloride (2%) 2 mL at the entry point.
Technique of PVB
A 4 inch 22 G stimuplex insulated needle was inserted perpendicular to the skin untill it contacted the transverse process of the vertebra. If needle failed to contact the process within 4 cm at the thoracic level or 5 cm at lumbar level, needle was withdrawn up to the skin and again reinserted at an angle of 100-150° with the skin in either cephalic or caudal direction. After contacting the transverse process, needle was slightly withdrawn and redirected cephalic at thoracic level and caudally at lumbar level to walk off the transverse process. Initially, nerve locator was set to deliver 3 mA current with 2 Hz frequency to achieve visible ipsilateral abdominal muscle contraction. Once contraction achieved, current was reduced gradually to 0.5 mA with nerve locator needle tip at approximately 1-2 cm deep from contact of transverse process. If there was no visible contraction, needle tip was manoeuvred in cephalad, caudal, medial or lateral direction and not in anteroposterior direction till visible contractions achieved. After achieving contractions at 0.5 mA current, inj. bupivacaine hydrochloride (0.5%) 4 mL and inj. lignocaine hydrochloride+adrenaline (2%) 3 mL (Total 7 mL volume per segment at all three segments) was injected slowly after repeated negative aspirations. Sensory blockade using pinprick (Gromley and Hill scale) was assessed at surgical site (ipsilateral) from level T8 below and motor blockade was assessed by modified bromage scale [2].
Spinal Anaesthesia
Spinal anaesthesia was given in sitting position. Under all aseptic and antiseptic precaution, painting was done and drape applied. Subarachnoid space was located with 9 inch 25 G spinal needle. Inj. bupivacaine hydrochloride (0.5%) Heavy 2.8-3.4 mL (Depending on various patient factors) was injected after aspiration of clear CSF. Sensory level T8 achieved by varying table position. Sensory blockade was assessed by pinprick (Gromley and Hill scale) and motor blockade by modified bromage scale [2].
Total procedure time (Time from needle insertion to completion of local anaesthetic drug injection) was noted in both groups. From time at which drug was injected (Zero time), time to achieve sensory block onset (Gromley and Hill scale Grade-1), time to achieve complete sensory block (Gromley and Hill scale Grade-2) and level of motor block were noted. O2 with venti-mask 4-6 L/minute was given to all patients. Intraoperatively as per blood loss ringer lactate, normal saline, colloids and/or blood were infused. Supplementation of light sedation was given for patchy insufficient effects, e.g., like perceived sensations at operative site during excessive surgical manipulation. General anaesthesia with assisted (with Laryngeal mask) or controlled ventilation (with Endo-Tracheal Tube) was given for failed block.
Complications like Nausea, vomiting, Hypo/Hypertension, Brady/Tachycardia, urinary retention were noted. Bradycardia, heart rate <60/minute was treated with inj. glycopyrrolate 0.2 mg or inj. atropine 0.6 mg iv and hypotension, SBP <25% of baseline SBP was treated with inj. mephentermine 6 mg iv. Postoperative pain was assessed by Visual Analogue Scale (VAS) having score of 0-10 (0 to 3-Mild pain, 4 to 7-Moderate pain and 8 to 10-Severe pain). Duration of analgesia (time from when block was given to VAS score >4 and rescue analgesic needed) was noted. Time to achieve ambulation was noted [10-12].
Statistical Analysis
Statistical analysis was done by Mean±SD for age, Unpaired t-test for onset and duration, procedural time and chi-square test for complications between SA and PVB groups. SPSS version 20.0 software was used for the analysis. p-value <0.05 considered as significant.
Results
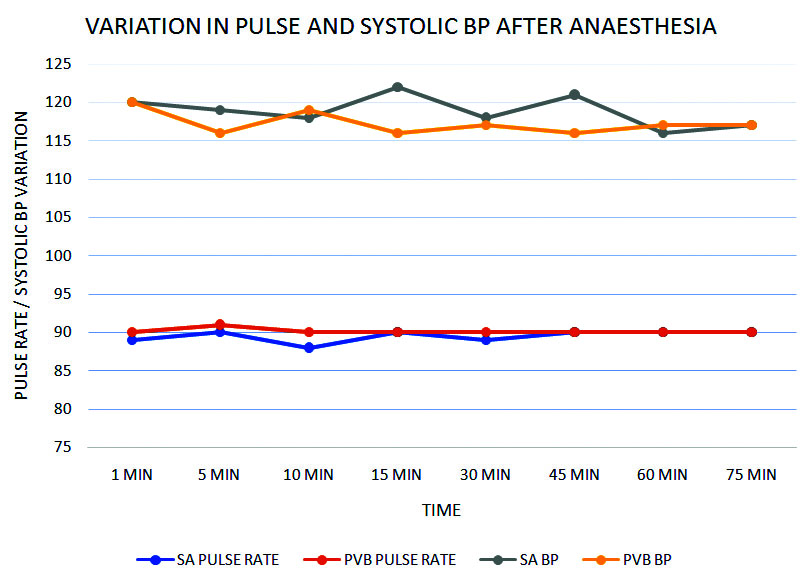
Two groups PVB and SA in the current study were comparable in age distribution of the patients. No significant difference (p=0.90) was found in relation to duration of surgery. Procedure time for PVB (16.30±2.41 minutes) was significantly higher than SA (3.32±0.74 minutes). Onset of sensory effect (p=0.0145) differs significantly between PVB and SA group. Group SA was having motor blockade of Bromage scale III in all the cases while there was no motor blockade (Bromage scale 0) in Group PVB. Sensory onset was earlier in group SA than group PVB. Time to achieve surgical anaesthesia was significantly higher (p<0.001) in group PVB as compared group SA (14.5±1.43 v/s 6.64±1.25 minutes) [Table/Fig-1]. No significant difference was observed in perioperative pulse and systolic blood pressure between PVB and SA groups [Table/Fig-2]. Duration of postoperative analgesia was reported from VAS score of patient at different times. Duration of analgesia (Till VAS Score was <4) was found significantly prolonged in group PVB (p<0.001). No complications were found in PVB group. Nausea (1), hypotension (3), and bradycardia (3) and urinary retention (1) were observed in patients in group SA.
Comparison of Variables between SA and PVB groups.
| Variable | SA | PVB | p-value | Remark |
|---|
| Age (years) | 43.72±10.05 | 44.60±9.40 | p=0.75>0.05 | Not significant |
| Duration of surgery (minutes) | 67.80±5.61 | 68.00±5.77 | p=0.90>0.05 | Not significant |
| Procedural time (minutes) | 3.32±0.74 | 16.30±2.41 | p<0.0001 | Significant |
| Onset of sensory blockade (minutes) | 4.52±0.92 | 5.32±1.28 | p=0.0145 | Significant |
| Time to reach surgical anesthesia (minutes) | 6.64±1.25 | 14.5±1.43 | p<0.0001 | Significant |
| Duration of analgesia (VAS Score <4) (minutes) | 212.78±25.11 | 370.80±42.91 | p<0.0001 | Significant |
Perioperative variation in Pulse and Systolic BP.
Discussion
Anaesthesia technique influences the postoperative monitoring, analgesics requirement and rehabilitation of the patients. Central neuraxial blockade i.e., SA is the most convenient method for inguinal hernia repair but associated with complete sensory and motor blockage with occasional haemodynamic alteration. Regional blocks including PVB is being preferred as an alternative technique to SA in many uncomplicated day care surgeries, providing adequate anaesthesia and analgesia without significant motor blockage [2]. The results show that both spinal anaesthesia and paravertebral block provide adequate anaesthesia and prolonged postoperative analgesia. This was demonstrated by reduced pain scores postoperatively. Lönnqvist PA and Hildingson U, had reported that the psoas muscle interrupts the paravertebral space at T12 level [9]. Keeping these in mind, three-segment PVB at the T10, T11 and L1 levels were used for PVB. Saito T et al., cited that the local anaesthetic injected in the ventral area of the lower thoracic paravertebral space, at the T11 level, resulted in an extended unilateral block, and favoured the single-injection, multi-segmental, paravertebral block [10]. However, due to technical difficulties and higher failure rates, multi-injection block was preferred. Procedure time i.e., time taken from needle insertion to local anaesthetic drug injection was noted higher in PVB group because PVB needed to be given at more than one level and lack of experience with the procedure compared to SA. Group PVB required significantly higher time to reach surgical anaesthesia as sub-arachnoid block was faster than nerve root blocks, Bhattacharya P et al., had also reported time to surgical anaesthesia for group PVB was 20±5 minutes and for group SA was 5±1 [11]. Akcaboy EY et al., also found it to be significantly higher for PVB (17±2.36 minutes) than for SA (11.3±1.5 minutes) [12].
Relatively larger volume of local anaesthetic was required to block the desired segments of paravertebral chain. An amount of 4 mL bupivacaine (0.5%) mixed with 3 mL lignocaine+adrenaline (2%) was given at all three levels. Observed duration of analgesia was significantly more (370.80±42.91 minutes) for PVB group. There was no lower limb motor paralysis noted with PVB (Bromage Scale 0), while there was complete lower limb motor paralysis with SA (Bromage scale 3). No patient in group PVB had any significant haemodynamic changes. Changes in haemodynamic parameters in SA group (hypotension-3 patients, bradycardia-3 patients) were due to bilateral blockage and also blockage of more segments in SA.
Failure of PVB was defined as failure of onset of pinprick discrimination within 15 minutes of giving block. Success rate of PVB noted was 80% in the present study. Five patients of PVB group had unsatisfactory effect of anaesthesia, so GA was supplemented. Eight patients of PVB group complained of occasional stretching pain and discomfort during surgery and were supplemented with Inj. fentanyl+Inj. ketamine. Bhattacharya P et al., had success rate of 93% with blind technique in their study [11]. Klein SM et al., used nerve stimulator guided PVB and got success rate of 90.9% [6]. Weltz CR et al., showed success rate of 93.33% in their study of PVB in inguinal hernia surgery [13]. Mandal MC et al., had also reported success rate of 84.6% with PVB [14].
Karmakar MK, also demonstrated use of PVB in 22 outpatient inguinal herniorrhaphy cases [15]. Thavaneswaran P et al., conducted systemic review of multiple clinical trials involving PVB for hernia and breast surgery [16]. They noted that PVB failure rate was not >13%. Patients were more satisfied with PVB and had shorter hospital stays than GA. PVB for anaesthesia substantially reduced nausea and vomiting in comparison with GA. Hence, different studies suggest that PVB can be used for uncomplicated unilateral hernia surgery as primary anaesthesia modality.
Limitation
Routine use of ultrasound would have increased success rate of the block but was not used because of its limited availability. Duration of anaesthesia in PVB could have been further increased by use of various adjuvants like clonidine, dexmedetomidine, fentanyl, tramadol, dexamethasone, ketamine etc., but was not used because of lack of standardisation and confounding effect. Smaller study population size is also one of the limiting factors for the evaluation of results.
Conclusion
Although Paravertebral Block requires longer Procedure time, sensory onset and time to reach surgical anaesthesia, complications like nausea, hypotension, bradycardia or urinary retention were significantly lesser as compared to SA. Selective unilateral blockage is observed in Paravertebral Block compared to bilateral and multiple segments blockages in Spinal Anaesthesia. Paravertebral Block with nerve locator significantly prolongs the duration of postoperative analgesia and reduces rate of complications in patients undergoing unilateral uncomplicated inguinal hernia surgery. Success rate can be improved by regular practice, use of ultrasound guidance and nerve stimulators. PVB can become a viable alternative to central neuraxial block when the latter is contraindicated.