The keratinised gingiva extends from the gingival margin to Muco-Gingival Junction (MGJ) and includes free and attached gingiva [1]. Attached gingiva is the firm and resilient part of the gingiva that is tightly bound to the underlying periosteum of alveolar bone through connective tissue. Attached gingiva is keratinised and aids in periodontium to increase resistance to external injury and contributes to stabilisation of gingival margin against frictional forces because of its histological characteristics that allow it to be tough, inflexible and resist abrasion. The thick network of closely packed collagen fibres resists the loading. Attached gingiva provides support against the physiological forces exerted by the muscular fibres of the alveolar mucosa on gingival tissues [2]. Attached gingiva can enhance the plaque removal around the gingival margin and can improve aesthetics and reduces inflammation around restored teeth. Gingival margin binds better around teeth and implants with adequate width of attached gingiva [3,4].
The width of the attached gingiva is defined as the distance between the MGJ and the projection on the external surface of the bottom of the gingival sulcus or periodontal pocket [5]. Traditionally, three methods are commonly used to determine the MGJ: visual method, functional method and histochemical staining method [6]. Hall WB suggested that the width of attached gingiva is determined by subtracting the sulcus or pocket depth from total width of gingiva. Clinically, the amount of keratinised gingiva can be recruited by stretching of the lips or cheeks to demarcate the MGJ and is considered to be insufficient when induces the movement of free gingival margin [7].
The width of attached gingiva on the facial aspect varies in different areas of the mouth. Incisor region has generally greatest width (3.5-4.5 mm in maxilla; 3.3-3.9 mm in mandible) and narrower in the posterior teeth (1.9 mm in maxillary and 1.8 mm in mandibular first premolars) [7]. Earlier studies by Ainamo A et al., have reported that the width of attached gingiva increases with age and in supraerupted teeth [2,8,9]. Andlin-Sobocki A et al., studied children 6-12 years of age and reported that width of attached gingiva increases with age [10]. However, Shaju JP et al., failed to support this observation in their study on Indian population [11].
Lang NP et al., in their study reported that the plaque free areas less than 2 mm of keratinised gingiva were inflamed despite effective oral hygiene and strongly suggested that an adequate width of (2 mm) keratinised gingiva is important for maintaining gingival health [12]. Subsequently, several authors challenged this concept. Miyasato M et al., and De Trey E et al., observed that the tissue could remain clinically healthy with less than 1mm of attached gingiva [13,14]. Wennstrom JL et al., in early 1980s conducted a series of studies on beagle dog model, that showed the attached gingiva and its width have little role in maintaining periodontal health and the gingival health. These can be maintained with almost no attached gingiva [15,16].
In teeth with subgingival restorations, however, it has been reported that a narrow zone of keratinised mucosa is associated with a higher chance of gingival inflammation [17]. Freedman AL et al., stated that the inadequate zone of gingiva would cause marginal gingival tissue movement and improper pocket closure thereby can facilitate subgingival plaque formation [18]. In an 18-year follow-up study on 17 subjects, Freedman AL et al., observed that, despite inadequate keratinised gingiva, the gingiva remains stable for long term with good oral hygiene and gingival health [19].
After a long pause, recent studies reported contradictory results on influence of inadequate attached gingiva on the prevalence of recession and oral hygiene maintenance [20,21]. It is worthy to note that majority of gingival recessions in the lower mandibular region are associated with shallow vestibule along with inadequate attached gingiva. Although not many studies have examined the role of inadequate vestibular depth in the aetiology of recessions, it is stated that gingival recession displaces the gingival margin apically, reducing the vestibular depth, which is measured from the mid-gingival margin to the mucobuccal fold [22].
Hence, the role of minimum width of attached gingiva and inadequate vestibular depth on gingival health and oral hygiene needs to be revisited. Also, there is paucity of human studies that showed correlation of width of attached gingiva with oral hygiene status, gingival inflammation and recession. The objectives of the present study are: 1) Assessment of width of attached gingiva and prevalence of gingival recession in young Malaysian adults; 2) To correlate the width of attached gingiva with oral hygiene status, gingival inflammation and recession. 3) To correlate depth of the vestibule with the above parameters.
Materials and Methods
A cross sectional clinical study was carried out. A total of 230 walk-in subjects were examined from screening clinic, MAHSA University during the period of October 2015 to October 2016. Institutional ethics committee clearance was obtained for the study (RMC/EC09/2015). Prior to commencement of the study, the procedure was explained to the participants both in writing and verbally after which an informed consent was taken. Subjects were included if their age was 20-40 years, without any missing and malaligned anterior teeth. Subjects with high frenum, prosthetic restorations, periodontal disease and orthodontic treatment and patients allergic to iodine were excluded.
After taking the informed consent, 165 patients between the age group of 20-40 years were recruited in the study, 90 female and 75 male. Oral hygiene status was evaluated using Simplified Oral Hygiene Index [23] and gingival inflammation was assessed by recording Modified Gingival Index [24], Sulcus Bleeding Index [25]. The tooth malalignment was observed by viewing the teeth from occlusal plane. The position of each tooth was classified in all participants according to its relation to the regular curve of the arch as either correctly, labially or lingually positioned [26]. Depth of the vestibule was also recorded from mid gingival margin to the mucobuccal fold. If there is recession, adjacent tooth gingival margin was considered. Periodontal parameters including probing depth, gingival recession, CAL were recorded using UNC-15 probe.
Measurement of Width of Attached Gingiva
After all the indices were recorded, mucogingival complex was dried first with the 3-way syringe and cotton rolls, then stained with Lugol’s solution using cotton pellet with light pressure burnishing technique. The Lugol’s solution was prepared by diluting 2g of potassium iodide and 1g of iodine crystals in 60mL of distilled water. The mucogingival junction can be visualised after staining the alveolar mucosa with Lugol’s iodine solution based on the difference in the glycogen content. The alveolar mucosa differs from keratinised gingiva histochemically in its glycogen content, acid phosphatase and nonspecific esterase content and an increased amount of elastic fiber content within the corium resulting in an iodo-positive reaction. The attached gingiva, which is keratinised, has no glycogen in the most superficial layer and gives an iodo-negative reaction [6]. Thus, Lugol’s iodine solution stains only the alveolar mucosa and clearly demarcates the mucogingival junction [Table/Fig-1].
Clear demarcation between keratinised gingiva and alveolar mucosa after Lugol’s staining.

After application of this solution, the keratinised gingiva was measured by using a digital calliper to get the more accurate reading [Table/Fig-2]. All the examiners were trained prior to the study regarding the protocol of recording clinical parameters by the standard examiner. All the measurements were recorded by a the standard examiner. Intra examiner reproducibility was calibrated on five patients and repeated measurements were recorded every third day for three visits. The distance from the crest of marginal gingiva to mucogingival junction was measured in the mid buccal region to get the width of attached gingiva on the buccal side of all the maxillary and mandibular anterior teeth, a total of 12 teeth. All the data collected was tabulated for statistical analysis.
Keratinised gingiva measured using digital calliper.

Statistical Analysis
Descriptive statistics and chi-square test were carried out to characterise the prevalence, extent, severity of gingival recession. The Student’s t-test was used to compare keratinised gingiva widths between teeth with and without root-surface exposure. For calibration of intra examiner reproducibility, one sample T-test was done. The correlation between width of attached gingiva or depth of the vestibule and gingival recession, gingival inflammation and oral hygiene status was assessed by Pearson’s correlation coefficient. These statistical analyses were independently performed using statistical software (Statistical Package for the Social Sciences, version 21.0; SPSS Inc, Chicago, USA). Differences were considered statistically significant when the p-value was <0.05.
Results
The participants included in the study were aged between 20-40 years. However, retrospectively it was observed that among the three races (Malay, Chinese and Indian) of Malaysia, in this study there is a predominance of Chinese participants. Hence, no interpretation was done on racial distribution of the parameters recorded. Mean width of attached gingiva for maxillary arch was 2.71mm and for mandibular arch was 2.37mm with an overall mean of 2.54mm. The mean depth of the vestibule was 9.68mm and 8.74mm for maxillary and mandibular arches respectively with an overall mean of 9.21mm. The mean gingival recession in maxilla was 0.09mm and 0.13mm in mandible and the total mean was 0.11mm [Table/Fig-3,4]. Intra examiner reproducibility was tested on five subjects for three visits and showed statistically good agreement between the readings at different visits (Cronbach’s alpha-0.97).
Demographic data with overall mean values.
| n | Males | Females | Mean Age±SD | Mean Width of AG | Mean depth of vestibule | Mean GR |
|---|
| 165 | 75 | 90 | 27.12±0.09 | 2.54±0.46 | 9.21±1.02 | 0.11±0.26 |
AG: Attached gingiva; GR: Gingival recession
Mean values of all parameters in maxilla and mandible.
| Variables | Width of AG | Depth of the vestibule | Gingival recession | | | |
|---|
| Maxilla | Mandible | Maxilla | Mandible | Maxilla | Mandible | OHI | MGI | BI |
|---|
| Male | 2.64±0.54 | 2.32±0.78 | 9.80±1.12 | 8.69±1.35 | 0.13±0.38 | 0.13±0.29 | 1.55±0.92 | 0.55±0.29 | 0.23±0.2 |
| Female | 2.76±0.51 | 2.42±0.85 | 9.58±1.12 | 8.78±1.35 | 0.05±0.22 | 0.13±0.30 | 1.53±0.96 | 0.53±0.23 | 0.22±0.24 |
| Total Mean±SD | 2.71±0.53 | 2.37±0.82 | 9.68±1.12 | 8.74±1.32 | 0.09±0.31 | 0.13±0.30 | 1.54±0.94 | 0.54±0.26 | 0.22±0.25 |
AG: Attached gingiva; OHI: Oral hygiene index (S); MGI: Modified gingival index; BI: Bleeding index
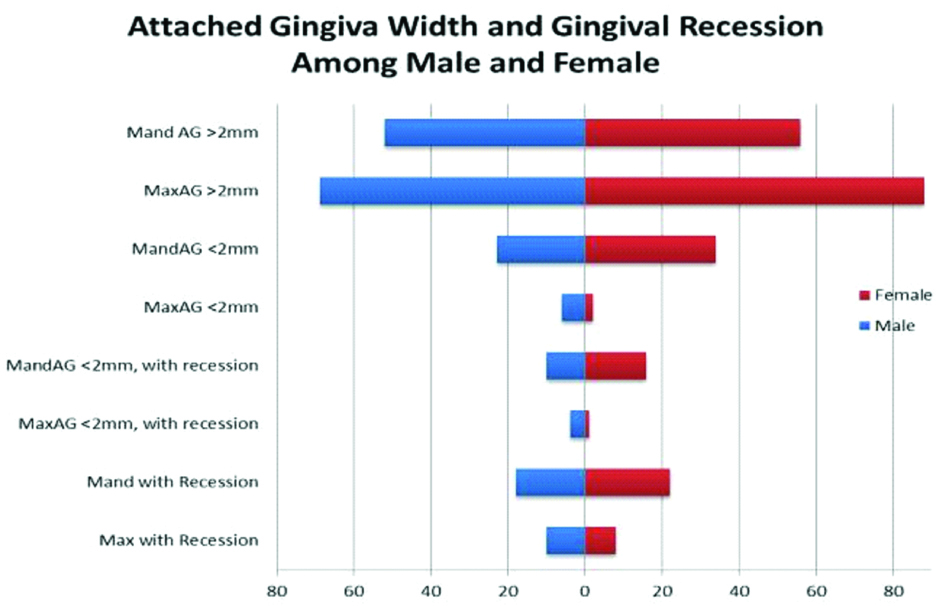
Prevalence of Gingival Recession
The study group comprised of 75 males and 90 females with mean age of 27.12±0.09 years. 63.6% subjects had a good to fair status of oral hygiene according to the OHI-S value and 121 (73.3%) subjects used soft/medium toothbrushes. The prevalence of gingival recession (at least one tooth with denuded root surface >1.0 mm) was 47/165 (28.5%). This prevalence was slightly higher in males than females (32% vs 25.5%) non-significant p=0.275. The prevalence of gingival recession was significantly higher (chi-square test, p<0.001) in the mandible (35/165, 21.2%) than in the maxilla (29/165, 17.5%) [Table/Fig-5,6].
Prevalence of gingival recession.
Gingival recession in association with gender and location.
| | | Gender | Location |
|---|
| n | Percent | Male (75) | Female (90) | Maxilla (165) | Mandible (165) |
|---|
| | | G0 | GR | G0 | GR | G0 | GR | G0 | GR |
|---|
| Gingival recession | 165 | 100.0% | 51 | 24 | 67 | 23 | 148 | 17 | 125 | 40 |
| p-value | 0.275# | <0.001** |
G0: No gingival recession; GR: Gingival recession present.
#statistically not significant at p≤0.05; **Highly significant at p≤0.05 (Chi-Square test).
Width of Attached Gingiva and Gingival Recession
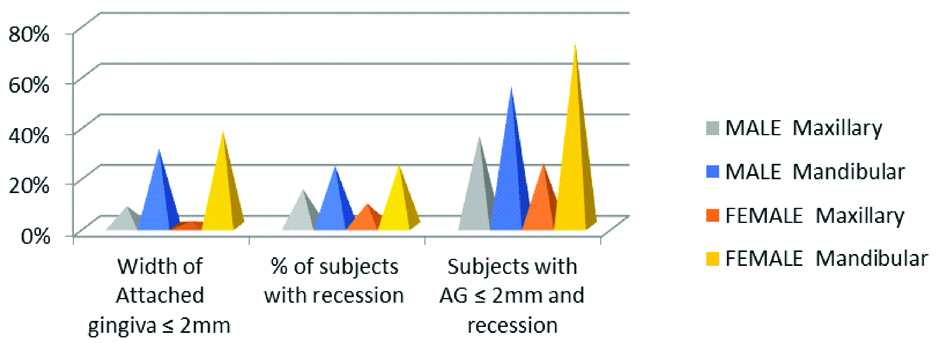
A narrow width of attached gingiva ≤2 mm was observed in 65/165 (39.4%) of the participants. The prevalence of gingival recession was more in subjects with width of AG ≤2 mm (32/59; 54.2%) than those with AG≥2 mm (27/59; 45.7%) and this difference was statistically significant (Paired T-test; p≤0.001). This observation appears to be more appropriate in mandible (26/32; 81.2%) as recession with AG ≤2 mm is greater in mandible compared to maxilla (6/32; 18.8%) [Table/Fig-7,8].
Gingival recession prevalence in relation to width of attached gingiva (>/≤2 mm).
Width of attached gingiva and gingival recession.
| Paired Differences | |
|---|
| 95% Confidence Interval of the Difference |
|---|
| Upper | t | df | Sig. (2-tailed) |
|---|
| Pair 1 | Max AG-Max REC | 0.91022 | 24.535 | 164 | <0.001 |
| Pair 2 | Mand AG-Mand REC | 0.557 | 7.642 | 164 | <0.001 |
**Paired T-test, p-value p≤0.001
Correlation of Width of Attached Gingiva and Gingival Recession
A negative correlation was found between the gingival recession and width of attached gingiva both in maxilla and mandible respectively. (Pearson’s correlation, r=-0.21, p=0.01; r=-0.19; p≤0.05). The frequency of root exposure is also significantly correlated with width of attached gingiva (r=-0.37; p≤0.001). This indicates that greater the width of attached gingiva, the lesser the occurrence of gingival recession. But this association is weak [Table/Fig-9].
Correlation between the parameters.
| Correlations | Pearson’s coefficient | p-value | Correlations | Pearson’s coefficient | p-value |
|---|
| Maxilla | Mean Attached Gingiva |
| Max. AG-Max GR | -0.217 | 0.05** | Mean AG-Mean MGI | 0.038 | 0.63 |
| Max DoV-Max GR | 0.126 | 0.107 | Mean AG-Mean BI | 0.144 | 0.065 |
| Max.AG-Max DoV | -0.020 | 0.799 | Mean AG-Mean OHI(S) | -0.068 | 0.387 |
| Mandible | Mean Depth of the Vestibule |
| Mand.AG-Mand GR | -0.195 | 0.12* | Mean DoV-Mean MGI | 0 | 0.99 |
| Mand.DoV-Mand GR | -0.158 | 0.043* | Mean DoV-Mean BI | -0.008 | 0.92 |
| Mand.AG-Mand DoV | 0.051 | 0.519 | Mean DoV-Mean OHI(S) | 0.015 | 0.852 |
| AG-Attached GingivaDoV-Depth of the vestibuleGR-Gingival recessionBI-Bleeding IndexMGI-Modified Gingival indexOHI(S)-Oral Hygiene Index | Mean GR-Mean MGI | 0.190 | 0.006* |
| Mean GR-Mean BI | 0.189 | 0.007* |
| Mean GR-Mean OHI(S) | 0.189 | 0.006* |
| Mean AG-Mean GR | -0.17 | 0.01* |
| Mean DoV-Mean GR | -0.05 | 0.24 |
| Mean AG-Mean DoV | 0.06 | 0.39 |
*Correlation is significant at the 0.05 level (2-tailed); **Correlation is significant at the 0.01 level (2-tailed).
Correlation of Width of Attached Gingiva with Oral Hygiene and Gingival Indices
Attached gingiva did not show any statistical significant correlation with oral hygiene index (r=-0.06; p=0.38), modified gingival index (r=0.03; p=0.63) nor with bleeding score (r=-0.14; p=0.06) [Table/Fig-9].
Correlation of Depth of the Vestibule with Other Parameters
No notable correlation was observed between width of the attached gingiva and depth of the vestibule (p>0.05). The depth of the vestibule showed a weak negative significant correlation with mandibular gingival recession (r=-0.15; p≤0.04) however, no significant correlation reported in maxilla. In this research, the correlation of vestibular depth with gingival inflammation or oral hygiene scores did not reveal any significant association between these parameters [Table/Fig-9].
Gingival recession showed a highly significant positive correlation with bleeding index (BI; p≤0.002) and MGI (p≤0.001) and OHI-S scores (p≤0.002), and which possibly indicates that poor oral hygiene can cause more gingival inflammation and can lead to greater gingival recession [Table/Fig-9].
Discussion
After the initial report on significance of attached gingiva by Lang NP et al., many studies have focused on this concept and some reported their findings in favour while others contradicted. An association between lack of attached gingiva and recession has often been implied in the literature [27]. Tenenbaum H observed a negative correlation between width of attached gingiva and the number of gingival recessions and also reported no significant correlation between oral hygiene and width of attached gingiva [28]. Ericsson I et al., suggested that an adequate band of attached gingiva could be defined as that amount which is sufficient to prevent gingival recession in opinion of individual practitioners [29]. Further, studies on the width of keratinised gingiva related to gingival recessions are limited. Almost for the past two decades, much of the attention shifted on volume of the keratinised gingiva around implants and subgingival restorations and the earlier concept remained unclear. In the literature review done by Mehta P et al., from 1972-2009, it was concluded that the width of attached gingiva is not significant to maintain periodontal health in the presence of adequate oral hygiene [30]. Previous studies have reported on several contributing factors that can predispose gingival recession like tooth malposition, traumatic brushing, frenum pull, gingival biotype and still considering width of the attached gingiva one among them [31-33]. The gingival features vary based on race and genetics. Hence, in the present study, the role of width of the attached gingiva in causing gingival inflammation, recession and in oral hygiene maintenance in Malaysian subjects was evaluated. In addition the influence of depth of the vestibule on the above parameters has been studied as well.
Earlier studies reported 29%-76% subjects of 15-32 years age group were associated with at least one root-surface exposure >1 mm [34]. The prevalence of gingival recession of the subjects in the present study was 28.6%. This prevalence as compared with the studies mentioned in the review paper is lower than Vietnamese (72.5%), France (84%), Brazil (64%) or Sweden (44%) population, while it is closer to prevalence in Nigeria (27.7%), India (24.29%) Israel (14.6%) [11,31-33]. However, the age group was not exactly the same in all these studies. But, it is commonly observed that gingival recession is not much common in young adults but it increases with age. In the present study, gingival recession was more predominant in males than females, however the difference is not significant perhaps due to less male sample size than females. Higher frequency of recession in males was reported in Indian, American and Turkey studies [11,31,34,35] and is attributed due to less frequency of dental visits, poor oral hygiene and smoking habit in males than females. The mean vestibular depth, measured from the marginal gingiva to mucobuccal fold was 9.21 mm. In patients with gingival recession either adjacent marginal gingiva level was considered. Ward VJ reported a vestibular depth range of 2.5 mm to 11.5 mm using radiographic technique [36].
In this study, 20-40-year-old age group of subjects were included because their permanent dentition was relatively complete and the occurrence of gingival recession had previously been detected in this age group and can be implied mostly to predisposing factors than chronic periodontal diseases [36]. Only subjects without any predisposing/aggravating factors of gingival recession (tooth malposition, smoking, orthodontic/periodontitis treatment, periodontal surgery, and fixed prostheses) were selected to assess the role of width of attached gingiva without any influence of confounding factors.
In this study, the assessment of width of attached gingiva was done in maxillary and mandibular anterior teeth only, as it is reported that prevalence of recession is high in mandibular anterior followed by maxillary anterior teeth [20,37]. Moreover, recession has an unesthetic impact if it is in the anterior teeth.
For the assessment of width of gingiva, the mucogingival junction serves as an important anatomical landmark, which can be demarcated by various methods. As suggested by Fasske E et al., the precise location of this junction can be visualised after staining with stains like Lugol’s iodine that aid in determining the exact point at which the keratinisation ends [38]. The HM staining method was chosen for assessment as it was reported that this method resulted in slightest intra and inter examiner variability [39]. In order to eliminate probing discrepancies all the measurements were carried out by a single examiner. All the examiners were trained prior to the study regarding the protocol of recording clinical parameters by the standard examiner. Intra examiner reproducibility was acceptable. The mid-buccal region was chosen as it is easily accessible and convenient. Digital calliper was used for recording instead of calibrated probe to avoid the errors of probing angulation to obtain a more accurate reading minimising subjective errors.
Among the various correlations tested in this study, significant correlation was shown among width of attached gingiva and gingival recession both in maxilla and mandible. The correlation coefficient is however weak perhaps warranting a greater sample size in future studies. This result is in agreement with those reported by Paturu DB et al., and Ngyuen-Hieu T et al., wherein significant negative correlation between narrow width of keratinised gingiva and gingival recession was reported [20,32].
In mandible, vestibular depth also was shown to have a significant influence on the gingival recession which is not there in the maxilla. This can be explained based on the anatomy and functional differences between maxilla and mandible. Maxilla is non-mobile. The depth of the vestibule in anterior maxilla could be due to greater amount of keratinised gingiva, greater upper lip height and attachment of orbicularis oris and oblique portion of nasalis muscles to the maxilla. Hence, although vestibular depth is low, attached gingiva might be adequate (2mm) or there might be less pull from the muscles due to less mobility. Also, the convexity of the maxilla could confer resistance and prevent recession. Conversely, the mandible and lower lip are more mobile. When the depth of the vestibule is less, the lip movements during speech and mastication can cause tension and movement of the free gingiva particularly in the absence of adequate keratinised gingiva, causing greater chances of gingival recession. Mazeland GRJ et al., suggested that, width of attached gingiva depends on height of alveolar process and vertical dimension of lower face [40].
To further validate this result, the association between depth of the vestibule and width of attached gingiva was tested but no correlation was reported. This confirmed that depth of the vestibule is dependent on various other factors such as muscle attachment, lip height, alveolar bone height and increased depth of the vestibule may or may not show greater keratinised gingiva.
In this study, no correlation was found among width of attached gingiva or vestibular depth with oral hygiene or gingival and bleeding indices. Recent study on Indian population reported a significant association of width of attached gingiva on Oral hygiene Index and Plaque index [21]. This difference might be due to the difference in age group of sample subjects. In the present study, subjects within 20-40 years were recruited to avoid the confounding effect of possible chronic diseases, uniformity in oral hygiene practices was ensured prior to the study. Whereas, Indian study included 15-65 years age group of subjects and oral hygiene practices were not controlled.
Limitation
Gingival biotype which is also considered as one of the predisposing factors for gingival recession was not assessed in this study. The oral hygiene status of majority of the participants in this study is good to fair. Therefore, the oro-dental status of the subjects in this study may differ from that of the young adults in the overall Malaysian population. This is a limitation of the study in that the results may not be generalised to all Malaysian population.
Conclusion
To conclude, within the limitations of this study, prevalence of gingival recession in our sample subjects was 28.6%. A weak negative correlation was found between width of attached gingiva, mandibular vestibular depth and gingival recession that could be inferred as, in the mandibular arch, width of attached gingiva can still possibly act as a factor that predispose to gingival recession. Depth of the vestibule in mandibular arch also was shown to have influence on gingival recession. However, the correlation is weak, these findings need to be further studied before confirmation. No significant correlation was shown between width of attached gingiva or vestibular depth and gingival inflammation and oral hygiene maintenance. Hence, for the maintenance of proper oral hygiene and gingival health, neither width of attached gingiva nor depth of vestibule was found to be significant. Future studies with larger sample and considering gingival biotype along with width of attached gingiva may show better understanding of the true correlation between these parameters.
AG: Attached gingiva; GR: Gingival recession
AG: Attached gingiva; OHI: Oral hygiene index (S); MGI: Modified gingival index; BI: Bleeding index