Valvular Heart Disease is an important cause of arrhythmia. In the recent years, there has been a steady decline in the prevalence of VHD and the resultant arrhythmias in western countries [1]. However, the prevalence still remains high in developing as well as in third world countries [2]. The patients with arrhythmias are highly prone to Cerebro Vascular Accidents (CVA) due to thromboembolic phenomenon. Early intervention can prevent and forestall these thromboembolic events particularly, primary and recurrent CVAs [3]. Prevention of these thromboembolic events requires that the patient receives anticoagulant therapy. The most common arrhythmia in VHD is Atrial Fibrillation (AF). A study by Wipf JE et al., reported AF prevalence rate of 75% in Rheumatic Heart Disease (RHD) [4]. Study done by Diker E et al., in 1110 patients of rheumatic VHD reported a frequency of 39% for AF [5]. AF due to VHD, particularly mitral valve disease has a substantially higher risk for CVAs than with AF with non-valvular heart disease. Also there is a greater CVA risk in patients with permanent AF than in patients with paroxysmal AF and the risk of stroke is highest in the year of onset of the arrhythmia [4].
Arrhythmias can result in symptoms like palpitations and syncope. But there are a substantial number of patients with VHD in whom arrhythmias may go undetected due to a paucity of clinical symptoms and in whom Holter monitoring has proved to be invaluable tool in identifying any underlying arrhythmias. Additionally, it is used for the analysis of the type, duration, severity, quantification and qualification of these arrhythmias in this population subset [6,7]. There are various echocardiographic variables, which are also associated with risk of onset of arrhythmia. If we can detect the arrhythmia early or detect the parameters which are associated with increased risk of arrhythmias, preventive measures can be undertaken.
The data on the prevalence of arrhythmias, particularly asymptomatic arrhythmias, type of arrhythmias and echocardiographic variables in the subset of population of VHD in South western part of the country is scanty which prompted us to undertake this study.
Materials and Methods
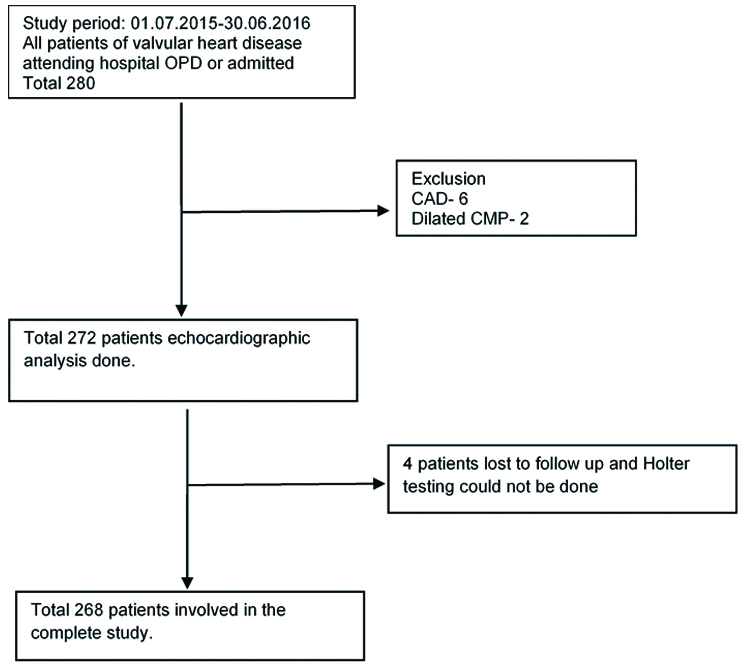
This cross-sectional observational study was conducted at a tertiary care teaching hospital over a period of one year from July 2015 to June 2016. Prior clearance was taken from the institutional ethical committee. Informed written consent was taken from the patients. Consecutive patients of all functional classes as defined by the New York Heart Association (NYHA) were included (Total 280). Patients with concurrent other heart diseases and patients below 18 years of age were excluded from the study. Coronary heart disease was excluded by ECG findings, echocardiography and wherever clinically suspected stress Myocardial Perfusion Imaging (MPI) was done. Total six patients were suspected to have CAD and were excluded. Two had dilated cardiomyopathy and were also excluded. Four patients were lost to follow-up. Rest of the patients (total of 268) were all included in the study [Table/Fig-1].
Showing patient participation.
A detailed history was taken to find out any symptoms related to the arrhythmias (unexplained syncope and palpitation that were non-exertional), history of alcohol intake or medication that can provoke arrhythmias. They underwent detailed physical examination, routine haemogram, biochemistry, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), chest radiography (X-Ray), thyroid profile and Electrocardiogram (ECG). All patients underwent an echocardiography (iE33 PHILIPS serial no-4158990) to affirm the presence of VHD, to study the various echocardiographic variables of Mitral Valve Area (MVA), Mitral Gradient (MG), Left Ventricular Internal Dimensions (LVID) and Left Atrial Diameter (LA dia) and to ascertain the current cardiac status. Consequent to which the patient underwent 24 hour ambulatory Holter monitoring (Holter medilog FD 12 Holter recorder with serial no 92345 made by Schiller). The patients’ Holter recordings were reviewed in our OPD and documented and were advised to promptly report if they developed any new symptoms when again ambulatory Holter monitoring for 24 hours was done.
Statistical Analysis
For baseline comparison of patients, chi-square (χ2) test was used for descriptive variables. Quantitative variables were compared using the independent sample t-test.
Sample size estimation: AF is the dominant arrhythmia in the patients with VHD. By considering the prevalence of AF in VHD in previous studies being 39% [3], we calculated the sample size (N) using the following formula:
N= 4xPxQ/L2
Where P=prevalence of disease=40%
Q=100-P=60%
L=experimental error-15% of P=6%
N=264.33=264(minimum sample required)
Results
There were 268 patients with mean age of 37±12 years in our study. The cohort comprised of 85 male (31.7%) and 183 females (68.3%). The demographic profile of the patients with relation to presence of arrhythmia is shown in [Table/Fig-2].
Arrhythmia in different age groups.
| Arrhythmia | Total |
|---|
| Present | Absent |
|---|
| Age group | ≤20 | 1 | 5 | 6 |
| 21-30 | 13 | 69 | 82 |
| 31-40 | 40 | 42 | 82 |
| 41-50 | 38 | 23 | 61 |
| 51-60 | 18 | 3 | 21 |
| >60 | 12 | 4 | 16 |
| Total | 122 | 146 | 268 |
Frequency of Different Valvular Lesions Detected in the Study: We found that Mitral Stenosis (MS) was present in 181(67.5%), Mitral Regurgitation (MR) in 155 (57.8%), Aortic Stenosis (AS) in 43(16%), Aortic Regurgitation (AR) in 45 (17%) of patients (total isolated as well as in combination) [Table/Fig-3]. Overall involvement of mitral valve was 243 (90.6%) and aortic valve was 48 (18%). The pulmonary valve involvement {both stenosis (PS) and regurgitation (PR)} was 0.7% and that of tricuspid valve involvement {both stenosis (TS) and regurgitation (TR)} was 14 (5.2%). Our study showed the various valvular involvements in decreasing frequency as follows: MS in 98(36.5%) >MS+MR in 64 (24%) >MR in 48 (17.9%) > AS in 10 (3.73%) >AR in 10 (3.73%) >MS+MR+AS+AR in 9 (3.36%) > MS+MR+AS in 7(2.61%) >MR+TR >AS+AR >MR+AS >MR+AR > MS+MR+TR [Table/Fig-3].
Frequency of various valvular lesions in the study group and presence of atrial fibrillation with relation to different valvular lesions; (%) denotes percentage in that cohort of valvular lesion.
| AF | | Total | (%), valvular lesions |
|---|
| Present | (%) | | In whole cohort |
|---|
| AR | 0 | 0.0 | 5 | 1.9 |
| AS | 0 | 0.0 | 10 | 3.7 |
| BAV | 0 | 0.0 | 5 | 1.9 |
| MS | 31 | 42.5 | 73 | 27.2 |
| MR | 11 | 25.6 | 43 | 16.0 |
| MVP | 0 | 0.0 | 5 | 1.9 |
| PS | 0 | 0.0 | 1 | 0.4 |
| AS+AR | 0 | 0.0 | 3 | 1.1 |
| MR+MS | 33 | 50.8 | 65 | 24.3 |
| MR+AR | 0 | 0.0 | 2 | 0.7 |
| MR+AS | 0 | 0.0 | 4 | 1.4 |
| MR+TR | 1 | 20.0 | 5 | 1.9 |
| MS+BAV | 1 | 100 | 1 | 0.4 |
| MS+AR | 1 | 25.0 | 4 | 1.4 |
| MS+TR | 1 | 100 | 1 | 0.4 |
| MS+AS | 3 | 60 | 5 | 1.9 |
| PS+TR | 0 | 0.0 | 1 | 0.4 |
| MS+AS+AR | 0 | 0.0 | 3 | 1.1 |
| MR +AS+AR | 0 | 0.0 | 1 | 0.4 |
| MR+AS+TR | 1 | 100.0 | 1 | 0.4 |
| MR+ AR+TR | 0 | 0.0 | 1 | 0.4 |
| MS+MR+AS | 2 | 28.5 | 7 | 2.6 |
| MS+MR+TR | 3 | 100.0 | 3 | 1.1 |
| MS+MR+AR | 2 | 25.0 | 8 | 2.9 |
| MS+MR+AS+ AR | 9 | 100.00 | 9 | 3.4 |
| MS+MR+AR+TR | 1 | 50 | 2 | 0.7 |
| 100 | | 268 | |
MS: Mitral Stenosis; MR: Mitral Regurgitation; AS: Aortic Stenosis; AR: Aortic Regurgitation; TR: Tricuspid Regurgitation; PS: Pulmonary Stenosis; AF: Atrial Fibrillation; BAV: Bicuspid Aortic Valve; MVP: Mitral Valve Prolapsed
There were 70 (26%) patients in NYHA (New York Heart Association) class-I, 104 (38%) in NYHA class-II, 65 (25%) in NYHA class III and 29 (11%) in NYHA class IV. Clinically 65 (25%) patients were found to be in heart failure and echocardiographically 198 (74%) had evidence of heart failure either as diastolic or as systolic dysfunction or both.
Symptoms with Arrhythmia: A total of 116(42.3%) patients were symptomatic with unexplained syncope and/or palpitation that were non-exertional. A total of 152 (56.7%) patients were asymptomatic. Arrhythmia was detected in 102/116 (90.2%) symptomatic patients and 19/152 (12.5%) of the asymptomatic patients. Statistically a significant correlation between the presence of symptoms and the presence of an arrhythmia (p<0.05) was found in our study.
Types of Arrhythmias: There were 122(45.5%) patients having arrhythmia in the study cohort. AF was found in 100 (37.3%), PVC in 24 (8.9%), Non-Sustained Ventricular Tachycardia (NSVT) and Paroxysmal Supra Ventricular Tachycardia (PSVT) in 14(5.2%), Ventricular Bigeminy (VB) in 7 (2.6%), Multifocal Atrial Tachycardia (MAT)/Atrio Venticular Block (AVB) in 5 (1.8%) of patients. This includes patients having combinations of arrhythmias too.
Valvular Lesions with Arrhythmia: Arrhythmias were present in 94(52%) of patients with MS (MS isolated and in combination), 74(47.7%) with MR, 29(67%) with AS, 16(35.5%) with AR and 7(50%) with TR [Table/Fig-4].
Frequency of overall arrhythmias in the study group with relation to different valvular lesions; (%) denotes percentage in that cohort of valvular lesion.
| Arrhythmia | |
|---|
| Present | (%) | Total |
|---|
| AR | 0 | 0.0 | 5 |
| AS | 7 | 70.0 | 10 |
| BAV | 2 | 40.0 | 5 |
| MS | 33 | 45.2 | 73 |
| MR | 13 | 30.2 | 43 |
| MVP | 1 | 20.0 | 5 |
| PS | 0 | 0.00 | 1 |
| AS+AR | 0 | 0.00 | 3 |
| MR+ MS | 34 | 52.3 | 65 |
| MR+AR | 0 | 0.0 | 2 |
| MR+AS | 3 | 75.0 | 4 |
| MR+TR | 1 | 20.0 | 5 |
| MS+BAV | 1 | 100.0 | 1 |
| MS+AR | 1 | 25.0 | 4 |
| MS+TR | 1 | 100.0 | 1 |
| MS+AS | 3 | 60.0 | 5 |
| PS+TR | 0 | 0.0 | 1 |
| MS+AS+AR | 0 | 0.0 | 3 |
| MR+AS+AR | 0 | 0.0 | 1 |
| MR+AS+TR | 1 | 100.0 | 1 |
| MR+AR+TR | 0 | 0.00 | 1 |
| MS+MR+AS | 6 | 85.7 | 7 |
| MS+MR+TR | 3 | 100.0 | 3 |
| MS+MR+AR | 2 | 37.5 | 8 |
| MS+MR+ AS+AR | 9 | 100.00 | 9 |
| MS+MR+AR+TR | 1 | 50.0 | 2 |
| Total | 122 | 268 |
MS: Mitral Stenosis; MR: Mitral Regurgitation; AS: Aortic Stenosis, AR: Aortic Regurgitation; TR: Tricuspid Regurgitation; PS: Pulmonary Stenosis, AF: Atrial Fibrillation; BAV:Bicuspid Aortic Valve; MVP: Mitral Valve Prolapse
Arrhythmias were commonly associated with multivalvular disease. Isolated MS showed 43% arrhythmics in its group and 36.5% in overall cohort, isolated MR had 29% arrhythmics in its group and 18% in overall cohort and MS+MR in combination had arrhythmia of 53% in its group and 24% in overall cohort. MS showed the maximum prevalence of arrhythmias. PVCs and Ventricular Tachycardia (VTs) were more associated with aortic valvular disease. AS showed 39% patients having PVCs. NSVT and PSVT were present in 30% of patients with AS.
AF was present in 33(51.5%) of 64 patients with MS+MR, 40(40.8%) of 98 patients with isolated MS, 48% of patients with MS (in isolation and combination when considered together), 11(22.9%) of 48 patients with isolated MR and in 45% patients when mitral/aortic valvular lesions were present together with TR [Table/Fig-3].
Left Ventricular Dysfunction with Arrhythmia: There were 29(11%) patients with severe LV dysfunction {ejection fraction (EF)<35%} and all of them had arrhythmia, 65(24%) patients with moderate LV dysfunction (EF<45%) out of which 52 had arrhythmia, 104(38%) had mild LV dysfunction out of which 37 had arrhythmia. A total of 118(59%) patients had arrhythmia in the cohort of LV dysfunction out of which AF contributed the most 99(50%), followed by PVC in 23(11.6%), VB in 7(3.5%) patients.
Digoxin with Arrhythmias: Digoxin was prescribed to many patients who were diagnosed having heart failure and AF. Total 69(25.7%) patients were on digoxin. Ventricular Bigemini (VB) was found in 07(10%) patients who were on digoxin and almost all VBs detected in the study were found in the patients on digoxin. Others on digoxin had PVCs 07(10%), NSVT, PSVT and AV blocks.
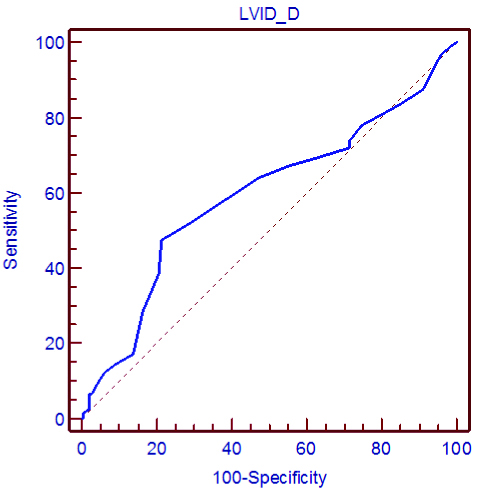
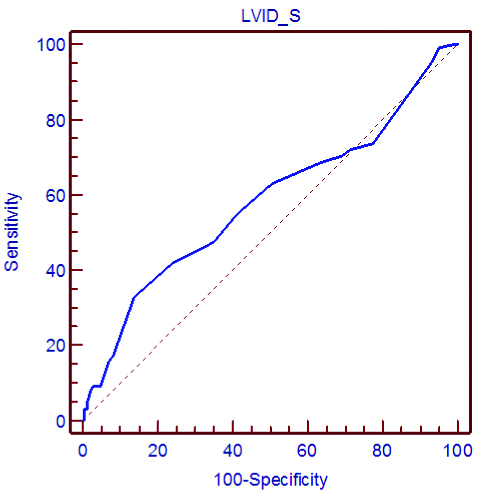
Arrhythmia with Different Echocardiographic Variables: The LVID D and LVID S phases in patients of AS, AR and MR when analysed together in relation to all arrhythmias (presence of any arrythmia), revealed mean values of 48.74±6.25 mm and 36.69±5.18mm respectively and were significantly related to presence of arrythmias. If we plot a regression curve (ROC) for these variables, a critical point was found beyond which the chance of arrhythmia increases. The critical point for LVID D and LVID S was greater than 50 mm and 39 mm respectively [Table/Fig-5,6 and 7].
Showing relation of arrhythmia with LVIDS and LVIDD in patients of MR, AR and AS together with mean (in mm), standard deviation (in mm) and critical point for presence of an arrhythmia.
| Arrhythmia | N | Mean | Std. Deviation | p-value | Critical point |
|---|
| LVID D | Present | 88 | 48.74 | 6.25 | 0.049 | 50 mm |
| Absent | 104 | 47.28 | 5.69 | | |
| LVID S | Present | 88 | 36.69 | 5.18 | 0.032 | 39 mm |
| Absent | 104 | 35.41 | 4.50 | | |
There is a significant relation (p-value <0.05) for these variables in relation to presence of an arrhythmia in these valvular lesions; LVID D: Left Ventricular Internal Dimension In Diastolic Phase; LVID S: Left Ventricular Internal Dimension In Systolic Phase
(ROC-1). Showing relation of presence of arrhythmia with left ventricular internal dimension in diastolic phase (LVID D) for all patients with MR or AS or AR. Critical point (*) in mm denotes the limit for the variable beyond which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
(ROC-2). Showing relation of presence of arrhythmia with left ventricular internal dimension in systolic phase(LVID S) for all patients of MR, AS or AR. Critical point(*) in mm, denotes the limit for the variable beyond which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
VARIABLE=LVID_D
CLASSIFICATION VARIABLE
Arrhythmia
POSITIVE GROUP
Sample size=88
NEGATIVE GROUP
Sample size=104
Disease prevalence unknown.
Area under the ROC curve=0.593
Standard error=0.035
95% Confidence interval=0.532 to 0.652
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
> 50 * 47.5 (38.4- 56.8) 78.8 (71.2- 85.1) 2.24 0.67
VARIABLE=LVID_S
CLASSIFICATION VARIABLE
Arrhythmia
POSITIVE GROUP
Sample size=88
NEGATIVE GROUP
Sample size=104
Area under the ROC curve=0.581
Standard error=0.035
95% Confidence interval=0.520 to 0.641
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
> 39 * 32.8 (24.6- 41.9) 86.3 (79.6- 91.4) 2.39 0.78
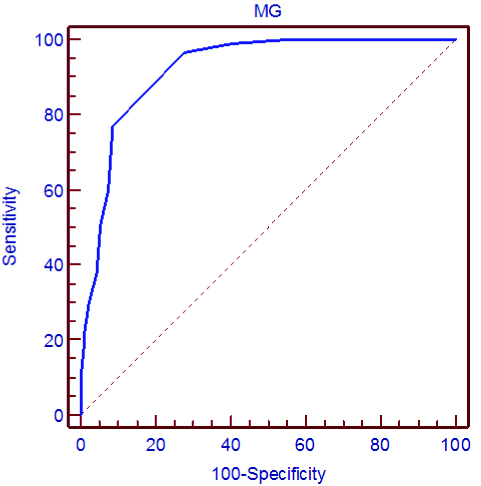
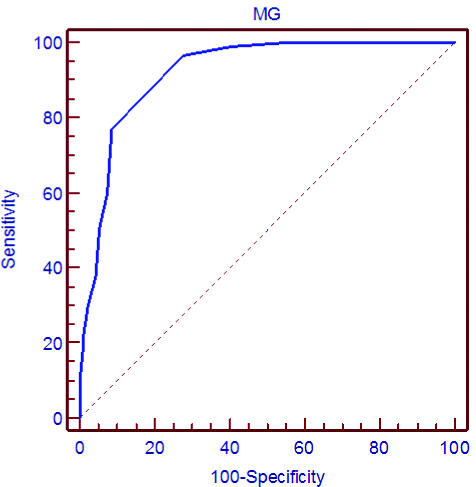
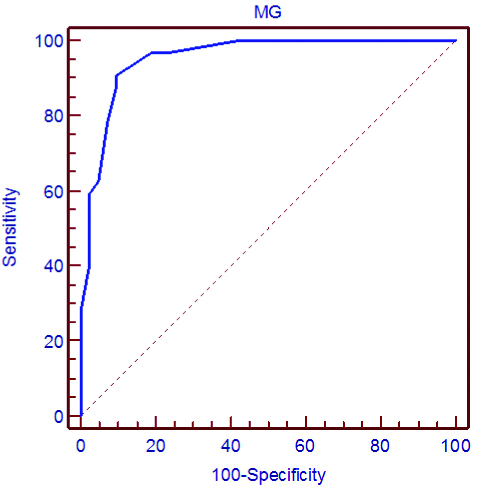
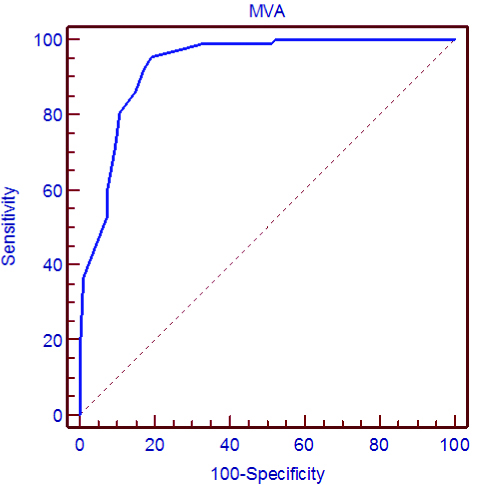
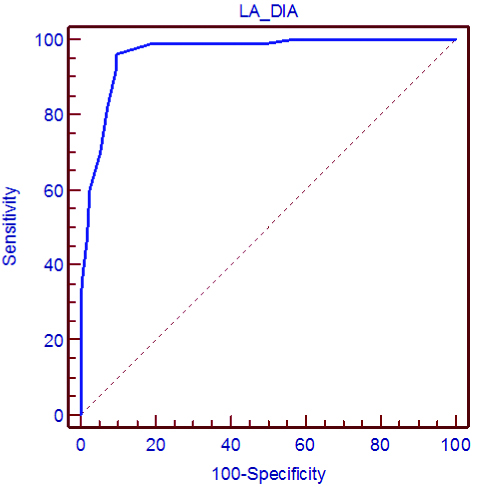
[Table/Fig-8] shows relation of AF with echocardiographic variables. In patients of MS and in combination (n=181) the critical point of MVA was <1.7 cm2 and MG was >8 mmHg [Table/Fig-9,10]. When only isolated pure MS was considered the critical point of MVA was <1.5 cm2 and MG was >9 mmHg [Table/Fig-11,12]. The mean LA diameter in patients with AF considering all the valve lesions was 48.73±3.57 mm and the criticalpoint was 43 mm [Table/Fig-13]. The LVID dimensions taken into account for all the 268 cases were not found significantly related to presence of AF.
Showing relation of AF with echocardiographic variables. Mitral valvular area and mitral gradient in patients of pure MS and in MS in combination with other valvular lesions.
| AF | n | Mean | SD | p-value | Critical point |
|---|
| MVA (pure MS) | Present | 31 | 1.10 | 0.38 | <0.001 | 1.5 cm2 |
| Absent | 42 | 2.33 | 0.72 | | |
| MG (pure MS) | Present | 31 | 12.08 | 2.93 | <0.001 | 9 mm of Hg |
| Absent | 42 | 6.84 | 2.72 | | |
| LA DIA | Present | 100 | 48.73 | 3.57 | <0.001 | 43 mm |
| Absent | 168 | 38.71 | 4.35 | | |
| MVA (all MS) | Present | 87 | 1.20 | 0.39 | <0.001 | 1.7 cm2 |
| Absent | 94 | 2.35 | 0.71 | | |
| MG (all MS) | Present | 87 | 14.03 | 3.10 | <0.001 | 8 mm of Hg |
| Absent | 94 | 6.21 | 3.02 | | |
| LVID D | Present | 100 | 48.42 | 6.59 | 0.337 |
| Absent | 168 | 47.66 | 5.60 | |
| LVID S | Present | 100 | 36.45 | 5.46 | 0.259 |
| Absent | 168 | 35.72 | 4.45 | |
LA diameter and LVID were considered in all the 268 patients. There is a significant relation (p-value <0.05) for these variables in relation to presence of AF in these valvular lesions except of LVID. LA DIA- Left Atrial Diameter, MVA- Mitral Valvular Area, MG- Transmitral Gradient. Mitral valvular area and mitral gradient was considered in 181 patients with MS (isolated or in combination with other valvular lesions) and also separately in pure MS patients (total 73 patients)
(ROC-3). Shows relation of presence of AF with mitral gradient (MG) in all patients of MS (Pure MS and MS in combination). Critical point (*) in mm, denotes the limit for the variable beyond which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
(ROC-4). Shows relation of presence AF with mitral valve area (MVA) in all patients of MS (Pure MS and MS in combination). Critical point (*) in mm, denotes the limit for the variable below which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
ROC-5). Shows relation of presence AF with mitral gradient (MG) in patients of MS (Pure MS only). Critical point (*) in mm, denotes the limit for the variable beyond which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
(ROC-6). Shows relation of presence of AF with mitral valve area (MVA) in patients of MS (Pure MS only). Critical point (*) in mm, denotes the limit for the variable below which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
Shows relation of presence of AF with left atrial diameter (LA dia) in all patients. Critical point (*) in mm, denotes the limit for the variable beyond which there is increased chances of developing an arrhythmia. In ROC critical point is the value which has maximum sensitivity and specificity taken together.
VARIABLE=MG
CLASSIFICATION VARIABLE
AF
POSITIVE GROUP
Sample size=87
NEGATIVE GROUP
Sample size=94
Area under the ROC curve=0.921
Standard error=0.021
95% Confidence interval=0.872 to 0.956
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
> 8 * 96.6 (90.2- 99.2) 72.3 (62.2- 81.1) 3.49 0.05
VARIABLE=MVA
CLASSIFICATION VARIABLE
AF
POSITIVE GROUP
Sample size=87
NEGATIVE GROUP
Sample size=94
Area under the ROC curve=0.930
Standard error=0.020
95% Confidence interval=0.883 to 0.963
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
<=1.7 * 95.4 (88.6- 98.7) 80.9 (71.4- 88.2) 4.98 0.06
VARIABLE=MG
CLASSIFICATION VARIABLE
AF
POSITIVE GROUP
Sample size=31
NEGATIVE GROUP
Sample size=42
Area under the ROC curve=0.953
Standard error=0.027
95% Confidence interval=0.878 to 0.988
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
> 9 * 90.6 (75.0- 97.9) 90.5 (77.4- 97.3) 9.52 0.10
VARIABLE=MVA
CLASSIFICATION VARIABLE
AF
POSITIVE GROUP
Sample size=87
NEGATIVE GROUP
Sample size=94
Area under the ROC curve=0.893
Standard error=0.025
95% Confidence interval=0.839 to 0.934
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
<=1.5 * 95.4 (88.6- 98.7) 80.9 (71.4- 88.2) 4.98 0.06
VARIABLE=LA_DIA
CLASSIFICATION VARIABLE
AF
POSITIVE GROUP
Sample size=100
NEGATIVE GROUP
Sample size=168
Area under the ROC curve=0.963
Standard error=0.014
95% Confidence interval=0.933 to 0.982
––––––––––––––––––––––––––––
Criterion Sens. (95% C.I.) Spec. (95% C.I.) +LR -LR
> 43 * 96.0 (90.1- 98.9) 90.5 (85.0- 94.5) 10.08 0.04
Discussion
The study shows high incidence of arrhythmias in valvular heart disease. Arrhythmia was found in 103/116(88.7%) of the symptomatic patients. A total of 19/152(12.5%) of the asymptomatic patients had Holter evidence of arrhythmias. Hence, a substantial percentage of asymptomatic patients had arrhythmias. In a study by Ramsdale DR et al., involving 65 patients with MS in sinus rhythm, 56% had transient atrial arrhythmias on Holter recordings, 95% of the episodes being asymptomatic, but embolic events occurred in 14% [8]. It is better to intervene before the symptoms occur to prevent dramatic complications which may include sudden death.
It is difficult to say whether the symptoms elicited on history were related to arrhythmia or not. Hence, in our study the proportion of patients with symptomatic arrhythmia may have been over estimated. Complaints such as palpitations and dizziness recorded during history-taking in patients may not necessarily mean arrhythmia nor they can be attributed to known arrhythmia unless the symptoms and the arrhythmia can be repeatedly documented to occur simultaneously. This was not done in our study. Hence actually the incidence of asymptomatic arrhythmia may be much more than 12.5%.
In the whole study group, arrhythmia was detected in 122(46%) patients. The mean age of the group having arrhythmia was 43.27±10.41 years and group without arrhythmia had a mean age of 34.37±11.2 years (p<0.05). These findings are comparable to those shown in a study by Diker E et al., wherein the mean age of the group with AF was 43.1±14.4 years and without AF had a mean age of 33.9±12.8 years [5]. Our study revealed MS to be most common valvular involvement and overall involvement of mitral valve was 243(90.6%) and aortic valve was 48(18%). A study done by Manjunath CN et al., in 13289 VHD where they systematically analysed large volume of echocardiographic data stored in the laboratory over a period of three years found that rheumatic heart disease contributed to 64.3 % of VHD and the order of involvement in their study was MR > MS > MS+MR> MS+AR > AS > MR+AR > AS+AR > MR+AS > MS+AS [9].
Arrhythmia was most common in mitral valve disease and the most common arrhythmia was AF. Diker E et al., reported a frequency of 29% for AF with isolated (pure) MS, 58% with MS in conjunction with mitral and/or TR and 16% in isolated MR and frequency of AF increased from 16% to 52% when TR occurred together with MR [5]. Bentivoglio LG et al., reported a 75% rate of chronic AF in isolated MR [10]. Patients with combined lesions of MS, MR and TR constitute the group with the highest rate of arrhythmia and AF in our study. It can be postulated that the atria are greatly affected haemodynamically in the presence of these lesions in combination.
AF is an infrequent finding in patients with aortic valvular disease. In our study, PVCs and VB were found to be associated with aortic valvular disease. There is a frequent association between AS and conduction disturbances like PVCs, Supraventricular (SVT) and Ventricular Arrhythmias (VT) for which there is a supporting evidence as mentioned in studies by Wolff RR et al and Widgren V et al., [11, 12]. We detected AF in 11% of patients with combined aortic valve disease and <1% in isolated aortic valve disease. Myler RK et al., reported a 1%rate of AF in aortic valvular disease [13]. Diker E et al., too found incidence of AF to be 3% in patients with aortic valvular disease [5].
This study showed arrythmia to be more common in patients with severe LV dysfunction. Urena M et al., studied arrhythmia burden in patients of severe AS who were TAVR candidates. They did 24-hour continuous ECG monitoring day before the procedure to detect previously unknown arrhythmias and found that lower LVEF was associated with higher incidence of paroxysmal arrhythmias and transient conduction disorders [14]. Studies have shown that the presence of left ventricular dysfunction in patients with aortic stenosis is associated with longer His-ventricular intervals as well as with a higher incidence of VT and AF [15]. Study by von Olshausen K et al., where they analysed incidence and severity of ventricular arrhythmias in 42 patients with pure or predominant mitral valve stenosis and 23 patients with pure or predominant mitral valve regurgitation employing 24 hour ambulatory monitoring, a significant inverse correlation was found between incidence and severity of VPB and left ventricular ejection fraction. A reduced right ventricular ejection fraction, on the other hand, barely affected the occurrence of complex ventricular arrhythmias. They concluded that frequent and complex ventricular arrhythmias may be a sign of reduced left ventricular function in patients with mitral valve disease [16].
A total of 118 (59%) patients had arrhythmia in the cohort of LV dysfunction out of which AF contributed the most 99 (50%), followed by PVC in 23 (11.6%), VB in 7 (3.5%) patients. A total of 16 (19%) patients had asymptomatic arrhythmias. Population-based studies have found the incidence of AF to increase with age and severity of heart failure [17]. Heart failure with AF identifies a subgroup with poorer prognosis. Middlekauf HR et al., in their study of 390 patients to clarify the prognostic significance of AF in Class III and IV heart failure patients of varied aetiology like CAD, Valvular heart disease and non-ischemic cardiomyopathy found AF in 19% cases. They found decreased survival with AF compared with sinus rhythm in patients who achieved low pulm capillary wedge pressure with vasodilators and diuretics [18]. They stated that probably the ones who could not achieve low pulmonary capillary wedge pressures already had such depressed LV function that any additional impairment due to AF was insignificant. There have been other studies which show no increase mortality in patients with heart failure with AF. Carson PE et al., reported from the Vasodilator in Heart Failure Trials (V-HeFT) that there was no significant change in mortality with presence of AF. However in the study, the cases had only mild to moderate heart failure [19]. Mahoney P et al., studied 234 patients eligible for heart transplantation. Mortality was similar in those with atrial fibrillation as with sinus rhythm. Atrial fibrillation was not an independent predictor of mortality [20].
Swedberg K et al., analysed the prognostic relevance of atrial fibrillation at baseline as well the importance of new-onset atrial fibrillation on subsequent patient outcome in their study of 3029 patients from the Carvedilol or Metoprolol European trail (COMET) where the effect of carvedilol compared with metoprolol tartrate was evaluated in patients with CHF during a mean follow-up of 58 months [21]. They found that occurrence of atrial fibrillation was associated with increase in risk of mortality. Hence, there are inconsistent reports on the prognostic implication of AF in patients with LV dysfunction.
Ventricular Bigemini (VB) was found in 07 patients of the total sample size and all of them were in patients who were put on Digoxin (p<0.05). Total 69 (25.7%) patients were on Digoxin. Others on digoxin had PVCs 07 (10%), NSVT, PSVT and AV blocks. One patient on digoxin had Atrial Tachycardia (AT) with variable AV block. In the meta-analysis of Zeng WT et al., digoxin use was associated with increased risk of death from any cause. They performed literature search using MEDLINE and EMBASE from 1966 to 2016 and 1980 to 2015 respectively. They in fact suggested that there is a need to reconsider use of Digoxin [22]. However, one major factor which needs to be considered as confounding is that most of the patients of advanced heart failure and resistant AF are started on Digoxin. However, this was not in the purview of our study of one-year duration. We did not have any patient with digoxin toxicity or overdose in our study group.
Univariate analysis of five echocardiographic variables in our study (LVID, LA diameter, MG and MVA) revealed association with an increased risk of overall arrhythmias (for LVID) and AF (for LA dia, MVA and MG). However, in the study by Diker E et al., MVA did not show any correlation as a predictor for AF [5]. They found Left atrial diameter and age as most important parameters in predicting onset of AF. This study also shows LA diameter to be important differing parameter between patients with and without AF. The LA diameter was 48.73±3.57 mm and 38.71±4.35 mm in patients with and without AF, respectively (p <0.001). As cited by Diker E et al., in their study, the LA diameter was 57±12 for having AF and 40±07 for not having AF [5]. In a report by Henry WL et al., the rate of AF was 3% when the LA diameter was ~4.0 cm, but it increased to 54% when the LA diameter was >4.0 cm [23]. However there still remains controversy regarding whether LA dilatation is a cause or a result of AF [24,25]. Because the mean transmitral gradient (MG) is shown to be higher by univariate analysis in patients with than those without AF (12.08±2.93 vs 6.84±2.72 mmHg), it can be correlated that a continuous pressure load on the left atrium may be a causative factor in the formation of AF. However, it should be realised that the underlying factor that causes higher MG in patients with AF may be the higher heart rate values in this patient group. Multivariate analysis in this study revealed LA diameter and increasing age to be the two most important variables that determine the occurrence of AF when all valvular lesions were considered together. In patients of MS (isolated considered separately, as well as when considered in combination with other valvular lesions), MG and MVA were significantly associated with occurrence of AF. In patients of MS in combination (n=181) the critical point of MVA was <1.7 cm2 and MG was >8 mm Hg. When only isolated pure MS was considered the critical point of MVA was <1.5 cm2 and MG was >9 mm Hg. Henry WL et al., as early as in 1976 evaluated 85 patients with isolated mitral valve disease, 50 patients with isolated aortic valve disease, and 130 patients with asymmetric septal hypertrophy. In all three groups of patients, atrial fibrillation was rare when left atrial dimension was below 44 mm (3 of 117 or 3%) but common when this dimension exceeded 40 mm (80 of 148 or 54%). In the review by Levy S et al., high frequency of AF was described in elderly patients with large left atria [23,26].
In our study, the echocardiopgraphic variables of LVID S and LVID D too had an association with overall arrhythmia. The mean LVID D for patients with MR, AS and AR together associated with an arrhythmia being 48.74±6.25 mm. Similarly, LVID S for patients with MR, AS and AR associated with an arrhythmia being 36.69±5.18 mm. These values are significant with p-value (<0.05). When all the 268 cases were considered (i.e., all the valvular involvements) risk of arrhythmia and of AF in relation to LVID was not found significant. Diker E et al., cited LVID D of 51±20 mm and 49±19 mm developing and not developing an AF respectively, LVID S of 32±14 mm and 30±15 mm for developing and not developing AF respectively and they too did not find any significant relation between LVID D & LVID S with AF when considering all the valvular heart disease [5]. It was found out that the critical point beyond which there is chance of developing an AF is when LA diameter >43 mm, for mitral stenosis patients for developing AF the critical point of MVA and MG are- MVA <1.7 cm2, MG >08 mmHg and critical point of LVID for developing an arrythmia in cases of MR, AR & AS are LVID D >50 mm and LVID S >39 mm.
Limitation
The sensitivity of 24-hour ECG Holter monitoring is low as compared to other modalities of investigations like Telemetry strips and Loop recorders in detecting arrhythmias and therefore, the rate of unknown events might be lower than reported. Second, patients showing positive MPI study were excluded from the study. However, it is known that patients with valvular heart disease may have myocardial perfusion abnormalities that are not associated with angiographic critical coronary stenosis [27]. No follow-up of the patient was done to confirm the CAD with angiography.
Conclusion
Overall the results of this study suggest that Holter monitoring should be done as a routine since asymptomatic arrhythmias are common. A combination of echocardiographic, demographic, and haemodynamic variables should be utilised to predict the likelihood of developing arrhythmias in VHD patients. The results of the current study may be extrapolated to the current incidence and patterns of VHD as it was done in a high volume tertiary care centre in this part of the country. Using the risk factors and the critical points of the echocardiographic variables identified in this study, a scoring system could be developed to further guide the patient care. So, further studies with larger sample size and multicentric studies are recommended.
MS: Mitral Stenosis; MR: Mitral Regurgitation; AS: Aortic Stenosis; AR: Aortic Regurgitation; TR: Tricuspid Regurgitation; PS: Pulmonary Stenosis; AF: Atrial Fibrillation; BAV: Bicuspid Aortic Valve; MVP: Mitral Valve Prolapsed
MS: Mitral Stenosis; MR: Mitral Regurgitation; AS: Aortic Stenosis, AR: Aortic Regurgitation; TR: Tricuspid Regurgitation; PS: Pulmonary Stenosis, AF: Atrial Fibrillation; BAV:Bicuspid Aortic Valve; MVP: Mitral Valve Prolapse
There is a significant relation (p-value <0.05) for these variables in relation to presence of an arrhythmia in these valvular lesions; LVID D: Left Ventricular Internal Dimension In Diastolic Phase; LVID S: Left Ventricular Internal Dimension In Systolic Phase
LA diameter and LVID were considered in all the 268 patients. There is a significant relation (p-value <0.05) for these variables in relation to presence of AF in these valvular lesions except of LVID. LA DIA- Left Atrial Diameter, MVA- Mitral Valvular Area, MG- Transmitral Gradient. Mitral valvular area and mitral gradient was considered in 181 patients with MS (isolated or in combination with other valvular lesions) and also separately in pure MS patients (total 73 patients)