Cough Induced Pneumomediastinum due to Tracheal Tear
K Devaraja1, Dipak Ranjan Nayak2, Poonam Ashok Kamath3
1 Assistant Professor, Department of Otorhinolaryngology and Head and Neck Surgery, Kasturba Medical College, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, India.
2 Professor, Department of Otorhinolaryngology and Head and Neck Surgery, Kasturba Medical College, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, India.
3 Intern, Department of Otorhinolaryngology and Head and Neck Surgery, Kasturba Medical College, Manipal Academy of Higher Education (MAHE), Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Devaraja, Assistant Professor, Department of Otorhinolaryngology and Head and Neck Surgery, Kasturba Medical College, Manipal Academy of Higher Education (MAHE), Manipal-576104, Karnataka, India.
E-mail: deardrdr@gmail.com
Spontaneous pneumomediastinum associated with subcutaneous emphysema following a sudden bout of cough is rare. Most of such pneumomediastinum would be associated with pneumothorax and would be a result of the ruptured pulmonary alveolus. Here, authors report a case of a 20-year-old male who developed swelling of neck and chest tightness following a sudden bout of cough. On examination, he was haemodynamically stable but had diffuse subcutaneous emphysema involving the neck and the upper chest. Radiology revealed pneumomediastinum without any pneumothorax. Authors think that the tracheal tear is the probable cause of air leak into soft tissue of the neck and the mediastinum. The patient was managed conservatively by close monitoring and supportive care. In patients with no prior underlying chest disease, and in those with no progressive respiratory distress, conservative treatment with cautious observation can successfully resolve this condition. This is a unique report, which attributes spontaneous pneumomediastinum without pneumothorax to the breach in the trachea.
Spontaneous pneumomediastinum, Subcutaneous emphysema, Tracheal injury
Case Report
A 20-year-old male patient with no prior comorbidities presented to emergency room with bilateral neck swelling for two days. The swelling was sudden in onset preceded by violent bouts of coughing. The patient noticed the gradual progression of the swelling to involve the entire neck and upper chest over the next 24 hours. He presented at the hospital within 48 hours of onset of neck swelling. He did not complain of any respiratory distress, nor was there any swallowing difficulty. He had no history of weight lifting and had not sustained any trauma in the week before the onset of symptoms. The patient had no history of pulmonary tuberculosis or other comorbidities, and there was no history suggestive of cyanosis, orthopnea or chest pain in the past or during these 48 hours. He was a painter by profession, had no habit of smoking and had not taken any medications/abusive substance. The patient was comfortable at rest with maintained saturation in room air. He was afebrile, and his heart rate, as well as blood pressure were within normal limits. Examination of the neck revealed diffuse subcutaneous emphysema extending from the lower mandibular margin to the nipple area on both the sides. Clinical examination of laryngopharynx and the respiratory system did not show any abnormality.
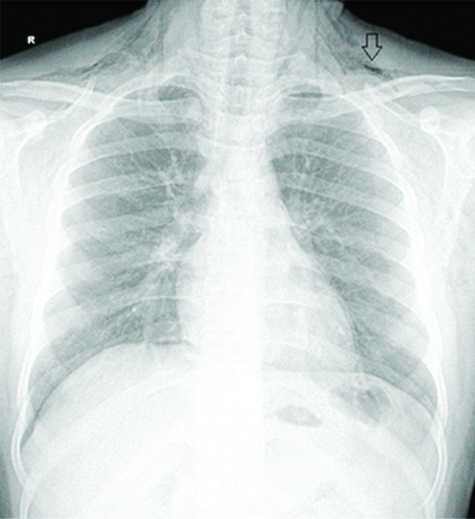
Large subcutaneous emphysema of neck was noted in plain roentgenogram done in the emergency room [Table/Fig-1]. For further characterisation and etiological clue, a Computed Tomography (CT) was asked, which showed the subcutaneous emphysema extending from the skull base to the suprasternal notch and the pneumomediastinum [Table/Fig-2]. The air was trapped subcutaneously from the masticatory space above to the level of nipples below. There was no evidence of any airway compression or narrowing of the major neck vessels. In the CT, the possible site of the leak was identified at the posterior lateral cervical trachea at the level of the C4 cervical vertebra [Table/Fig-3]. Both the plain roentgenogram and the CT revealed the absence of the pneumothorax. Contrast oesophagram with thin barium ruled out any injury of the pharynx or the oesophagus [Table/Fig-4].
Plain roentgenogram showing the cervical subcutaneous emphysema (arrow) in the absence of a pneumothorax.
Coronal image of the contrast-enhanced computed tomography showing extensive subcutaneous emphysema of the neck (white arrow) and the chest wall (stars) along with the pneumomediastinum (arrow through the circle).

Axial image of the contrast-enhanced computed tomography of neck showing the probable site of the tracheal tear (black arrow).

a) Barium swallow study showing the normal flow of contrast in the oropharynx; b) hypopharynx and c) oesophagus.

The patient was closely observed with the serial monitoring of subcutaneous emphysema by measuring the neck and chest circumference. Since he maintained well with no further worsening of subcutaneous emphysema, he was managed non-surgically. The treatment included bed rest, oxygen by mask, anti-reflux and anti-tussive medications. The subcutaneous emphysema started resolving within 24 hours of hospitalisation. The patient was discharged after five days of conservative treatment, by which time, the majority of subcutaneous emphysema was subsided.
Discussion
Bout of a violent cough can rarely lead to spontaneous pneumomediastinum and cervical subcutaneous emphysema [1]. The mechanism of air entrapment in such cases is thought to be the rupture of the alveolus and the centripetal air-leak to the mediastinum [2]. After briefly reviewing the literature related to pathophysiology and clinical manifestations of spontaneous pneumomediastinum, in the subsequent paragraphs, authors give an alternative hypothesis for the cause of air leak seen in the present case.
Apart from cough, subcutaneous emphysema and pneumomediastinum can also occur following some other events like strenuous exercises, vigorous sneezing, emesis, forced Valsalva manoeuver or cocaine abuse [3-8]. However, in 20% to 50% of the patients who develop spontaneous subcutaneous emphysema and pneumomediastinum, there may not be any identifiable triggering event or precipitating factors [4,8-11]. The spontaneous subcutaneous emphysema-pneumomediastinum complex commonly affects young adults in their second and third decades and has a male preponderance [3,6,8,10-13]. This age and sex predilection is due to relatively high workload and muscular activity, this group engages.
The manifestations of spontaneous pneumomediastinum include sudden onset of neck swelling, neck pain, chest pain, dyspnea, with or without preceding rigorous physical activity [6,8-11]. Clinically, the affected individual would generally maintain the normalcy in blood pressure, heart rate and oxygen saturation, unless the subcutaneous emphysema or pneumomediastinum is massive and is compressing on the major vessels [6]. Though the Hamman crunch, i.e., crepitus felt due to the trapped air in the mediastinum is diagnostic of pneumomediastinum, it can be appreciated only in the minority of the diagnosed patients [9]. However, the plain roentgenogram is a very sensitive radiological tool for making the diagnosis of spontaneous subcutaneous emphysema and pneumomediastinum and often is the only investigation necessary to make this diagnosis [9,10,13]. Nevertheless, the CT may be needed in selected cases, to assess the extent of the air leak in thorax and neck, and to aid the identification of the site of air leak as well [6]. CT in the index case did show the probable site of air leak. Authors think that the cervical trachea might have given way at the posterior-lateral junction between membranous and cartilaginous parts, due to a violent cough and a sudden increase in intrathoracic and intra-tracheal pressures.
The pre-existing pulmonary conditions like asthma, post tubercular obstructive airway disease, and bronchial foreign body can predispose to secondary pneumomediastinum in any age group [10,13]. Most of these cases of secondary pneumomediastinum would be due to rupture of pleura or emphysematous bulla and would be associated with pneumothorax [4]. In contrast, the spontaneous pneumomediastinum in the absence of pneumothorax is probably due to air leak from the tracheal breach as seen in the index case. The rupture of the trachea causing spontaneous air leak is more likely when the tracheal wall has already been insulted by surgery like thyroidectomy [14]. These cases of tracheal tear would present as sudden onset of subcutaneous emphysema in the postoperative period. However, such a rupture of the trachea can happen spontaneously also, especially when the intra-tracheal pressure increases enormously against the closed glottis, as seen in activities like a sudden bout of cough or rigorous weight lifting exercise. In general, the breach in cervical trachea presents as subcutaneous emphysema in neck with or without pneumomediastinum (mostly minimal and stable), and the affected patients would maintain the vitals in normal range [14]. Contrarily, if the air leak is from the pulmonary alveolus, the patients would present with pneumothorax, pneumomediastinum and subcutaneous emphysema (mostly rapidly progressive), and the patients would be in distress necessitating quick intervention. Another possible source of the air leak in these cases is the oesophageal tear. According to a recent study the oesophageal perforation is seen in 10% of the spontaneous pneumomediastinum cases [15]. Older age, the presence of pleural effusion and the elevated white blood cells have been shown to predict the possibility of oesophageal perforation in spontaneous pneumomediastinum cases, necessitating at least a contrast swallow study in those cases [15]. However, no such findings were noted in the index case nor did the contrast study yielded positively, supporting present hypothesis and the decision of a minimalist approach.
Almost all of the primary cases and the majority of the secondary cases of spontaneous pneumomediastinum cases can be managed non-surgically by supportive care [1,3-5,8-10,12,16]. The medical management includes hospitalisation, bed rest, analgesics, oxygenation with or without antibiotics and a follow-up roentgenogram after 48-72 hours [6,10]. As against the pneumomediastinum associated with underlying chest pathology, the primary spontaneous pneumomediastinum cases would have a lower association with pneumothorax, would have a shorter hospital stay and exhibit less morbidity [4,8]. Underlying pulmonary pathology and association with pneumothorax are the factors which might complicate the scenario and mandate active surgical intervention in these cases [6,8,13]. Since there were no adverse factors in present case, and as the pneumomediastinum was non-progressive, conservative management was followed effectively.
Conclusion
Primary spontaneous subcutaneous emphysema- pneumomediastinum complex is rare in male patients in their 2nd and 3rd decades. The characteristic clinical features and the plain roentgenogram would lead to diagnosis in the majority of the cases. Computer tomography can help in estimating the extent as well as in identifying the probable cause. In the absence of predisposing parenchymal disease and impending respiratory distress, conservative treatment with cautious observation can successfully resolve this condition.
[1]. Chiba Y, Kakuta H, Massive subcutaneous emphysema, pneumomediastinum, and spinal epidural emphysema as complications of violent coughing: a case reportAuris Nasus Larynx 1995 22(3):205-08.10.1016/S0385-8146(12)80061-7 [Google Scholar] [CrossRef]
[2]. Macklin CC, Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implicationsArch Intern Med 1939 64(5):913-26.10.1001/archinte.1939.00190050019003 [Google Scholar] [CrossRef]
[3]. Gunluoglu MZ, Cansever L, Demir A, Kocaturk C, Melek H, Dincer SI, Diagnosis and treatment of spontaneous pneumomediastinumThorac Cardiovasc Surg 2009 57(4):229-31.10.1055/s-2008-103905919670118 [Google Scholar] [CrossRef] [PubMed]
[4]. Caceres M, Ali SZ, Braud R, Weiman D, Garrett HE, Spontaneous pneumomediastinum: a comparative study and review of the literatureAnn Thorac Surg 2008 86(3):962-66.10.1016/j.athoracsur.2008.04.06718721592 [Google Scholar] [CrossRef] [PubMed]
[5]. Berger N, Nichols J, Yap V, Datta D, An unusual cause of acute-onset chest pain: spontaneous pneumomediastinumConn Med 2015 79(4):201-05. [Google Scholar]
[6]. Perna V, Vilà E, Guelbenzu JJ, Amat I, Pneumomediastinum: is this really a benign entity? When it can be considered as spontaneous? Our experience in 47 adult patientsEur J Cardiothorac Surg 2010 37(3):573-75.10.1016/j.ejcts.2009.08.00219748792 [Google Scholar] [CrossRef] [PubMed]
[7]. Maeder M, Ullmer E, Pneumomediastinum and bilateral pneumothorax as a complication of cocaine smokingRespir Int Rev Thorac Dis 2003 70(4):40710.1159/00007290514512677 [Google Scholar] [CrossRef] [PubMed]
[8]. Bakhos CT, Pupovac SS, Ata A, Fantauzzi JP, Fabian T, Spontaneous pneumomediastinum: an extensive workup is not requiredJ Am Coll Surg 2014 219(4):713-17.10.1016/j.jamcollsurg.2014.06.00125053221 [Google Scholar] [CrossRef] [PubMed]
[9]. Gasser CR-B, Pellaton R, Rochat CP, Pediatric spontaneous pneumomediastinum: narrative literature reviewPediatr Emerg Care 2017 33(5):370-74.10.1097/PEC.000000000000062526855340 [Google Scholar] [CrossRef] [PubMed]
[10]. Macia I, Moya J, Ramos R, Morera R, Escobar I, Saumench J, Spontaneous pneumomediastinum: 41 casesEur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg 2007 31(6):1110-14.10.1016/j.ejcts.2007.03.00817420139 [Google Scholar] [CrossRef] [PubMed]
[11]. Banki F, Estrera AL, Harrison RG, Miller CC, Leake SS, Mitchell KG, Pneumomediastinum: etiology and a guide to diagnosis and treatmentAm J Surg 2013 206(6):1001-06.10.1016/j.amjsurg.2013.08.00924296102 [Google Scholar] [CrossRef] [PubMed]
[12]. Çakmak M, Yüksel M, Kandemir MN, Analysis of patients with spontaneous pneumomediastinumTurk Thorac J 2016 17(3):105-08.10.5578/ttj.3050529404135 [Google Scholar] [CrossRef] [PubMed]
[13]. Panigrahi MK, Suresh Kumar C, Jaganathan V, Vinod Kumar S, Spontaneous pneumomediastinum: Experience in 13 adult patientsAsian Cardiovasc Thorac Ann 2015 23(9):1050-55.10.1177/021849231560630326394630 [Google Scholar] [CrossRef] [PubMed]
[14]. Devaraja K, Kumar R, Sagar P, Kumar R, Delayed presentation of tracheal injury after thyroidectomy-a case reportIndian J Surg 2018 Ahead of print. Available from: https://doi.org/10.1007/s12262-018-1748-x10.1007/s12262-018-1748-x [Google Scholar] [CrossRef]
[15]. Potz BA, Chao LH, Ng TT, Okereke IC, Clinical Significance of Spontaneous PneumomediastinumAnn Thorac Surg 2017 104(2):431-35.10.1016/j.athoracsur.2017.02.05128527963 [Google Scholar] [CrossRef] [PubMed]
[16]. Wong K, Wu H-M, Lai S-H, Chiu C-Y, Spontaneous pneumomediastinum: analysis of 87 pediatric patientsPediatr Emerg Care 2013 29(9):988-91.10.1097/PEC.0b013e3182a26a0823974718 [Google Scholar] [CrossRef] [PubMed]