Optic Disc Melanocytoma Associated with Choroidal Neovascular Membrane: An Unusual Presentation
Gladys Reshma Rodrigues1, Teena Mariet Mendonca2, Shobha G Pai3, KS Amruthavalli4
1 Consultant, Department of Ophthalmology, Manipal Academy of Higher Education (MAHE), Mangalore, Karnataka, India.
2 Senior Resident, Department of Ophthalmology, Manipal Academy of Higher Education (MAHE), Mangalore, Karnataka, India.
3 Professor, Department of Ophthalmology, Manipal Academy of Higher Education (MAHE), Mangalore, Karnataka, India.
4 Junior Resident, Department of Ophthalmology, Manipal Academy of Higher Education (MAHE), Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gladys Reshma Rodrigues, Consultant, Department of Ophthalmology, Kasturba Medical College, Mangalore-576104, Karnataka, India.
E-mail: gladysdoc@rediffmail.com
Optic disc melanocytoma is a unilateral benign lesion of the optic nerve head, rarely causing visual disturbances. Vascular changes causing central retinal vein occlusion, compressive or mechanical effects of the mass over the optic nerve head can cause decrease in visual acuity. Here, authors report a case of optic disc melanocytoma associated with Choroidal Neo-Vascular Membrane (CNVM) causing visual impairment which is one of the rare association.
Choroidal neovascularisation, Optic disc pigment anomaly, Unilateral benign lesion
Case Report
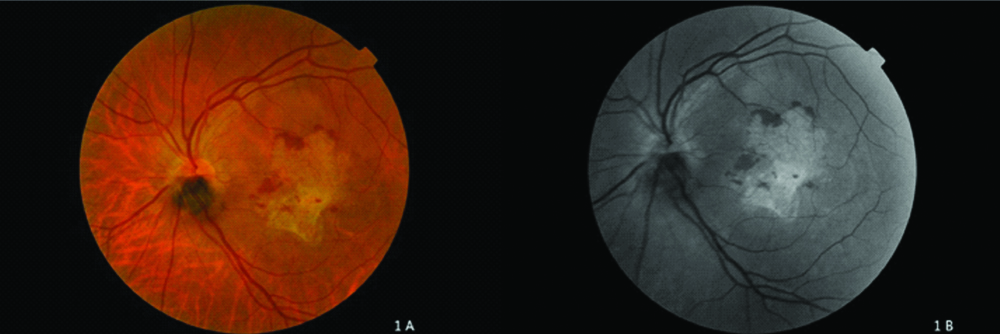
A 49-year-old female patient presented to the Department of Ophthalmology with gradually progressive decreased vision in the left eye of five to six months duration. She was not a known hypertensive or diabetic. Her best corrected visual acuity in the right eye was 6/6 and in the left eye was finger counting at ½ m. The extraocular motility, external examination, pupillary responses were unremarkable. On slit lamp examination, anterior segment was normal except for nuclear sclerosis of the lens. Retinal examination in the left eye revealed dark black elevated mass of 1 Disk Diameters (DD) in size occupying inferior half of the optic disc extending on to the adjacent inferior peripapillary retina [Table/Fig-1a]. The retinal vessels were normal and the superior disc margins were well defined. A greyish white membrane of 3.5 DD was present at the macula. The nasal border of the membrane was about 0.5 DD from the temporal disc margin and the superior and inferior borders were about 1 DD from the temporal arcades. An area of subretinal fluid is seen above the superior border of the membrane of about 1 DD. The inferotemporal area of the membrane occupying the foveal region was slightly denser than the rest of the membrane suggestive of scarring. Subretinal haemorrhages are present at the superior and nasal borders of the membrane which were better seen on red-free fundus photo [Table/Fig-1b].
Colour fundus photograph (Fig 1a) shows black elevated lesion occupying the inferior half of the optic disc extending onto the adjacent peripapillaryretina. A yellowish membrane is seen over the macula with few interspersed h’ages at the nasal and superior border of the membrane. Red free photograph (Fig 1b) shows more clearly the extensions of the choroidal neovascular membrane and the retinal h’ages.
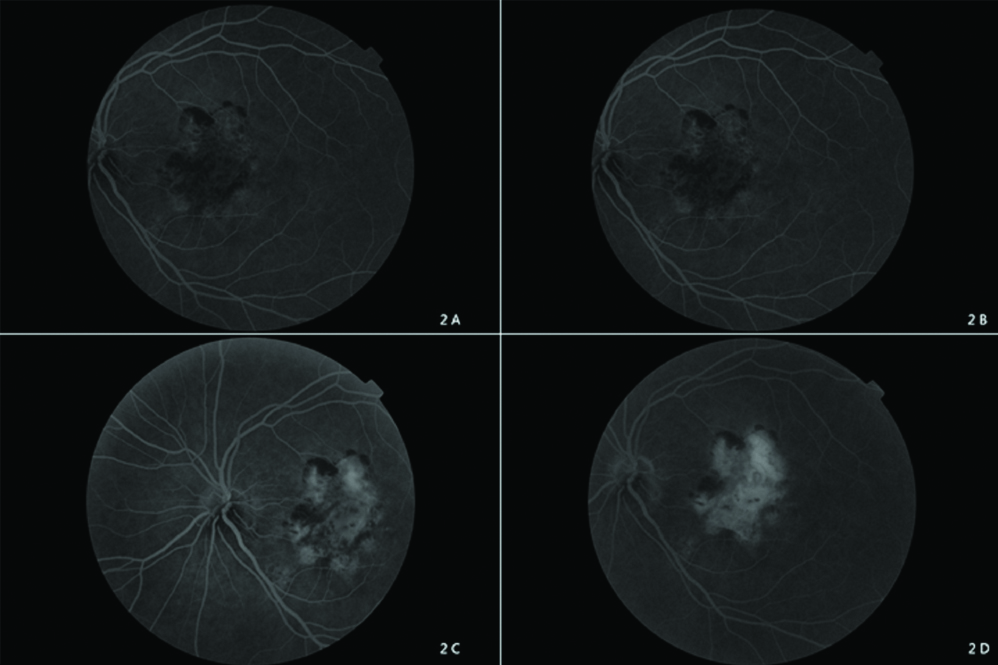
On Fundus Fluorescein Angiography (FFA) the optic disc melanocytoma was hypo-fluorescent throughout the procedure due to blocking effect by the pigment [Table/Fig-2]. An irregular area of hypo-fluorescence was seen over the macular area with hyper-fluorescent borders in early stages which gradually increased both in size and intensity in the later stages, suggestive of the choroidal neovascular membrane. Blocked fluorescence was seen over the area of haemorrhages. Spectral domain OCT revealed altered foveal contour with hyper-reflective Retinal pigment-choriocapillary complex with mild intraretinal fluid and minimal subretinal fluid [Table/Fig-3a].
Fundus fluorescein angiography (Figure2a-d) shows areas of hyperfluorescence increasing in size and intensity in later stages suggestive of CNVM, and areas of blocked fluorescence corresponding to the areas of haemorrhage.
Spectral domain OCT (Fig 3a) shows altered foveal contour with increased intra-retinal thickness and hyper-reflective RPE-CC complex suggestive of CNVM.
B-scan (Fig 3b) reveals a smooth rounded elevated area in the region of the optic nerve head.

B-Scan revealed an elevated rounded lesion in the optic nerve region with regular internal reflectivity [Table/Fig-3b].
Hence, authors arrived at a diagnosis of Left eye Optic disc melanocytoma with CNVM with predominant scarring over the macula. The guarded visual prognosis was explained and anti-VEGF injection was advised but patient was lost for follow-up.
Discussion
Melanocytoma is defined as a specific variant of melanocytic naevus which is located in the optic disc or anywhere in the uveal tract [1]. Optic disc melanocytoma is usually a stable lesion and does not affect vision in most cases. In the present case, the vision loss was due to CNVM which is a rare complication seen in less than 1% of optic disc melanocytoma. Subretinal choroidal neovascular membrane can occur either due to damage of Bruch’s membrane directly by the tumour cells or by local inflammatory events leading to choroidal neovascular tissue formation. Various treatment modalities have been attempted. Treatment with Anti-VEGF agents such as Bevacizumab has shown good results. Urrets-Zavalia JA et al., reported regression of CNVM after three Bevacizumab injections [2], whereas Kamisasanuk T et al., reported improvement of CNVM with a single injection of Bevacizumab [3]. Argon Laser photocoagulation is a treatment option for Polypoidal Choroidal Vasculopathy (PCV) associated with optic disc melanocytoma [4]. Photo-Dynamic Therapy (PDT) is a treatment option for CNVM overlying papillomacular bundle. Chalam KV et al., reported the efficacy of PDT in optic disc melanocytoma with juxtafoveal CNVM with good visual recovery and regression of the CNVM [5]. Pars plana vitrectomy and submacular removal of the membrane has been reported for optic disc melanocytoma associated with peripapillary CNVM [6].
Vision may be affected due to the mechanical effects of the mass over the optic nerve head or due to secondary vascular effects. Mechanical effects of the mass over the optic nerve head can cause disc oedema, central retinal artery occlusion, central retinal vein occlusion, ischaemic tumour necrosis, retinal exudation and rarely CNVM. These complications may result in the visual loss which is usually mild [7]. Afferent pupillary defect if present, is due to compression of the optic nerve by the mass optic disc melanocytomas may be locally invasive but malignant transformation is rare and can occur in 1-2% of the cases [8,9]. There are also reported cases of vitreous seeding with cataract, secondary glaucoma. Vitreous seeding is due to the necrosis of the tumour and the necrotic tissue and the melanin are phagocytosed by the macrophages which produce an inflammatory reaction that causes trabecular plugging and secondary glaucoma. On the other hand, malignant melanoma, even though it’s rare, also can simulate melanocytoma [10].
One of the main differential diagnosis of optic disc melanocytoma is malignant melanoma which needs to be ruled out. Mass of more than 1.5 mm thickness, presence of orange pigment over the mass, presence of subretinal fluid suggests malignant changes which can be confirmed with the help of B scan ultrasound and FFA [11,12]. Choroidal nevus, hyperplasia of the retinal pigment epithelium, adenoma of the retinal pigment epithelium and metastatic melanoma of the optical disc are the other differential diagnosis. It is very difficult to distinguish these lesions clinically. Hence procedures like FFA, OCT and B-Scan are helpful. On FFA, there was hypo-fluorescence throughout, in the inferior part of the optic disc as compared to melanoma which is hyper-fluorescent in the later stages. The hypofluorescence in the area of the optic disc is due to the deeply pigmented cells and the compact arrangement.
Visual field analysis usually shows changes in 90% of the patients even though the patients are asymptomatic. The changes include enlarged blind spot or nerve fibre layer defect which suggests an extension of the mass onto the adjacent retina and choroid. Visual field analysis in the present case was not possible due to poor vision.
Conclusion
Vision loss though very rare in optic disc melanocytoma is mainly due to the compression of the optic nerve fibres or ischaemia due to compromised vascular supply of the optic nerve head.
Vision loss may also be caused by secondary effects such as tumour necrosis causing ischaemic optic neuropathy. CNVM is one of the rare complications associated with optic disc melanocytoma leading to poor vision. Hence, regular follow-up to look for malignant changes and also associated complications such as CNVM is important. CNVM can be treated with intravitreal anti-VEGF injections. Other modalities such as focal laser and PDT can be used to treat the exudation but the visual benefit may be limited due to damage to adjacent neural tissue. Present patient presented at a later stage when there was significant scarring associated with CNVM which limited her visual recovery.
[1]. Paul R, Kulshrestha M, Shanmugalingam S, Barr D, Melanocytoma of optic disc: clinical manifestations, imaging characteristics and follow upAmerican Journal of Medical Case Reports 2015 3(4)Science and Education Publishing Co., Ltd:113-6.Available from: http://dx.doi.org/10.12691/ajmcr-3-4-810.12691/ajmcr-3-4-8 [Google Scholar] [CrossRef]
[2]. Urrets-Zavalia JA, Crim N, Esposito E, Correa L, Gonzalez-Castellanos ME, Martinez D, Bevacizumab for the treatment of a complicated posterior melanocytomaClin Ophthalmol 2015 9:455-59.10.2147/OPTH.S8015225834382 [Google Scholar] [CrossRef] [PubMed]
[3]. Kamisasanuk T, Uchino E, Sakamoto T, Choroidal neovascularization of optic disk melanocytoma treated with bevacizumabEur J Ophthalmol 2012 22(3):503-05.10.5301/ejo.500006021959681 [Google Scholar] [CrossRef] [PubMed]
[4]. Nicolás El-Haddad M, Clement Fernández F, Pérez-Salvador E, Martín Reyes C, Polypoidal choroidal vasculopathy in a patient with a melanocytoma of the optic nerveArch Soc Esp Oftalmol 2002 77(8):455-58. [Google Scholar]
[5]. Chalam KV, Gupta SK, Shah GY, Agarwal S, Successful management of melanocytoma-associated choroidal neovascularization with photodynamic therapyEur J Ophthalmol 2006 16(5):776-78.10.1177/112067210601600523 [Google Scholar] [CrossRef]
[6]. Tran HV, Bovey EH, Uffer S, Zografos L, Peripapillary choroidal neovascularization associated withmelanocytoma of the optic disc: a clinicopathologic case reportGraefes Arch Clin Exp Ophthalmol 2006 244(10):1367-79.10.1007/s00417-006-0270-116523299 [Google Scholar] [CrossRef] [PubMed]
[7]. Al-Rashaed S, Abboud E, Nowilaty S, Characteristics of optic disc melanocytomas presenting with visual dysfunctionMiddle East African Journal of Ophthalmology. Medknow 2010 17(3):24210.4103/0974-9233.6548820844679 [Google Scholar] [CrossRef] [PubMed]
[8]. Mansour AM, Zimmerman L, La Piana FG, Beauchamp GR, Clinicopathological findings in a growing optic nerve melanocytomaBr J Ophthalmol 1989 73(6):410-15.10.1136/bjo.73.6.4102751972 [Google Scholar] [CrossRef] [PubMed]
[9]. Shields JA, Demirci H, Mashayekhi A, Eagle RC, Shields CL, Melanocytoma of the optic disk: A review. Vol. 51Survey of Ophthalmology 2006 :093-104.10.1016/j.survophthal.2005.12.01116500211 [Google Scholar] [CrossRef] [PubMed]
[10]. Erzurum SA, Jampol LM, Territo C, O’Grady R, Primary malignant melanoma of the optic nerve simulating a melanocytomaArch Ophthalmol 1992 110(5):684-86.10.1001/archopht.1992.010801701060341580845 [Google Scholar] [CrossRef] [PubMed]
[11]. Shields JA, Demirci H, Mashayekhi A, Shields CL, Melanocytoma of optic disc in 115 cases: the 2004 Samuel Johnson Memorial Lecture, part 1Ophthalmology 2004 111(9):1739-46.10.1016/S0161-6420(04)00543-3 [Google Scholar] [CrossRef]
[12]. Reese AB, Congenital melanomasAm J Ophthalmol 1974 77(6):789-808.10.1016/0002-9394(74)90382-1 [Google Scholar] [CrossRef]