Inflammatory Bowel Disease is a chronic, relapsing inflammatory disorder of gastrointestinal tract of uncertain aetiology that encompasses chronic UC and CD [1]. Traditionally, IBD was regarded as a disease of western countries such as North America and Europe. However, it started gaining popularity in south East Asia only after mid 1980s with a wider availability of colonoscopy. Before then, it was often difficult to diagnose and distinguish from more prevalent non specific colitis. Moreover, CD was often undiagnosed and labelled as tuberculosis and rarely, it use to be reported on surgical specimens [2].
Later on, at the turn of 21st century, there has been an epidemiological shift, with increased detection and reporting of IBD from Africa, South America and Asia including India, with spread of specialist gastroenterology, availability of modern equipment and technology to visualise the entire gut [3,4]. With this rise, there has been increased detection of IBD cases in our centre (eastern Nepal) over the last two years (2015-2017), as compared to preceding six years (2009-2015). Only anecdotal report of IBD cases from our centre of Eastern Nepal has been published and there is not much literature on incidence and management of this so called uncommon disease in the country [5,6]. Only a single review of 18 cases of CD with extraintestinal manifestations over a six year period (2009 to 2014) by a Gastroenterology unit from central Nepal has been studied till date [7]. The aim of this study was to review the experience in the disease profile and management of IBD, and increase the awareness of this specific bowel disease among the treating physician, radiologist and the pathologist.
Materials and Methods
All patients who had attended the Department of Surgery, BP Koirala Institute of Health Sciences (BPKIHS), a tertiary care centre in Eastern region of Nepal between January 2009 to May 2017, and had been diagnosed with UC and CD were included. The patients were divided into two time period (first period: January 2009 to March 2015; second period: April 2015 to May 2017) as a separate Surgical Gastroenterology unit with its specialised team was established from 2015. This institute is an academic, referral centre, which cater around 1.5 million population. Retrospective study of prospective collected data included: patient demographics, extent and severity of disease as per Montreal classification, surgical interventions and recurrence. Descriptive analysis was performed and the data are presented as mean for continuous variables or median and ranges as appropriate. Total count and percentages are reported for categorical variables. The study was approved by the Institutional Ethics Committee (IRC/1178/017) and proper informed consent was taken from the patients.
Results
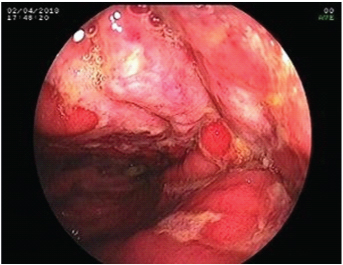
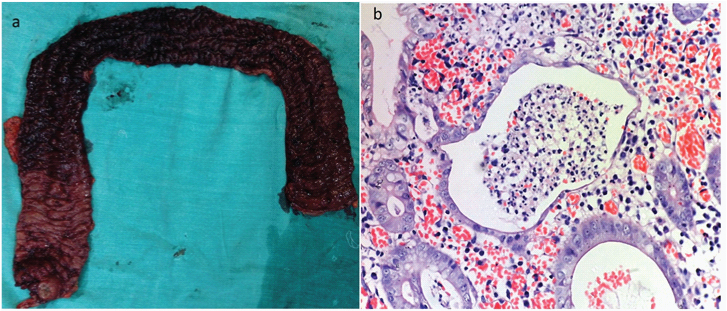
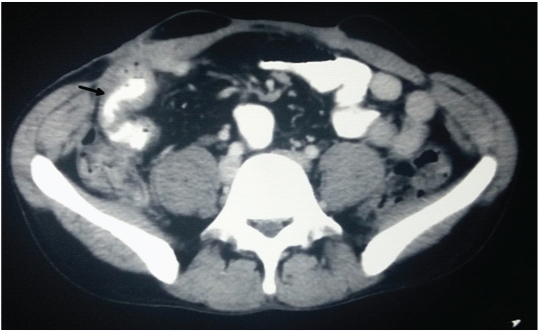
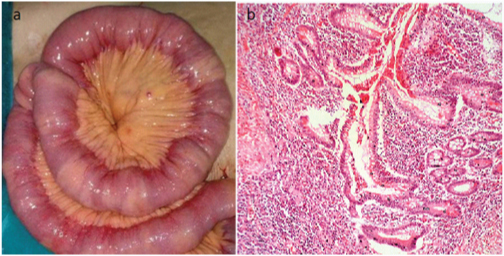
Thirty inflammatory bowel disease patients were managed at our unit, 11 in first time period (UC-8, CD-3) and 19 in the second period (UC-11, CD-8). There was a sharp increase in management of IBD cases in second period as compared to the first (9.5 vs 1.8 cases/year). Out of total 30 IBD cases, 19 (63%) patients were of UC [Table/Fig-1,2] and 11 (37%) patients were of CD [Table/Fig-3,4,5]. The ratio of UC: CD was 1.7:1. The patient demographics, treatment and outcome are shown in [Table/Fig-6].
Colonoscopic view of left colon showing complete loss of vascular pattern, multiple superficial ulceration (>5mm in size) with mucopurulent exudates suggesting severe colitis.
Ulcerative colitis: (a) Total colectomy specimen showing evidence of colitis extending continuously from rectum to ascending colon suggesting pancolitis; (b) Histologic section of active ulcerative colitis showing cryptitis and crypt abscess (H&E, X100).
Contrast- enhanced computed tomogram of Crohn’s disease patient showing long-segment, asymmetrical thickening of distal ileum (arrow).
(a) Crohn’s disease of small bowel showing skip areas, mesenteric fat creeping and multiple passable strictures; (b) Microscopic features of Crohn’s disease showing crypt distortion and cryptitis (H&E, x100).
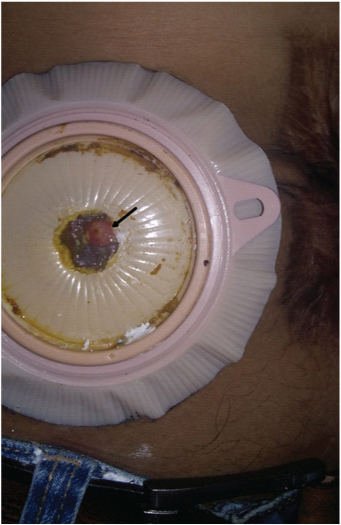
Showing matured enterocutaneous fistula (arrow) at previous ileostomy closure site in a patient with Crohn’s disease, suggesting recurrence of disease.
Patient Demographics, treatment and outcome.
| UlcerativeColitis (N=19) | Crohn’sDisease (N=11) |
|---|
| Median Age (yr) (range) | 45.1 (28-70) | 55 (28-75) |
| Sex (M:F) | 1.3:1 | 1.7:1 |
| Current Smokers | 5 (26.3%) | 4 (36.3%) |
| Median duration of Illness in months (Range) | 15 (3-48) | 6 (3-36) |
| Presenting symptomsRectal bleedingPain abdomenPerianal discharge | 19 (100%)8 (42.1%)- | 1 (9%)9 (81.8%)1 (9%) |
| Disease LocationL1 (Terminal Ileum)L2 (Colonic)L3 (Ileocolonic)L4 ( Proximal Small bowel) | - | 7 (63.6%)2 (18.2%)1 (9%)1 (9%) |
| Disease behaviourB1 (Inflammatory)B2 (Structuring)B3 (Fistulizing) | - | 4 (36.3%)3 (27.3%)4 (36.3%) |
| Disease extentProctitisLeft sided colitisPancolitis | 1 (5.2%)10 (52.6%)8 (42.1%) | - |
| Severity of colitisMildModerateSevereFulminant | 7 (36.8%)5 (26.3%)5 (26.3%)2 (10.5%) | - |
| Extraintestinal manifestation | 2 (10.5%) | 1 (9%) |
| TreatmentMedicalSurgical*Anti-TNF therapy | 12 (63.6%)7 (36.3%) | -11 (100%)2 (18.2%) |
| Recurrence ** | | 3(27.3%) |
* No 90-day postoperative mortality
* There were three (15.9%) patients with major postoperative complication (small bowel obstruction, ischaemic hepatitis and controlled Ileal pouch anal anastomotic leak) in UC group managed conservatively, and three (27.3%) patients (anastomotic leak) in CD group requiring re-exploration and stoma.
** Enterocutaneous fistula at stoma closure site, small bowel involvement in perianal chron’s following fistulectomy and Ileal stricture at ileocolic anastomotic site
UC patients (n=19): The median age of the patient was 45.1 (range: 28-70) years with a M:F ratio of 1.3:1. The most common presenting symptom was rectal bleeding (n=19, 100%) and pain abdomen (n=8, 42.1%). Pancolitis was seen in 8 (42.1%) patients; left sided colitis in 10 (52.6%); rectosigmoid involvement in 1 (5.2%) patient. Severe to fulminant colitis was seen in 37% of patients. Extraintestinal manifestation (sacroilitis and peripheral arthritis each) was seen only in 2 (10.5%) patients. Seven patients (36.3%) required surgical intervention (staged restorative total proctocolectomy with an ileoanal pouch- 6, total proctocolectomy with end ileostomy for carcinoma in situ- 1). Total three surgeries including single stage proctocolectomy/end ileostomy were performed in the first period, while the remaining four were performed in the second period. The remaining twelve cases (63.6%) of total UC were managed with a non operative treatment. At 12 months post surgery, all patients reported a good pouch function with high satisfaction and adjustment.
CD patients (n=11): The median age of the patient was 55 (range: 28-75) years with a M:F ratio of 1.7:1. The most common presenting symptom was pain abdomen (81.8%). Six (54.5%) patients presented to emergency with acute abdomen (intestinal obstruction- 4 and perforation- 2) and 1 (9%) patient with rectal bleeding and ileus requiring an emergency surgery. Eight (72.7%) patients had a predominant small bowel involvement while one (9%) patient had both small and large bowel involvement. Extraintestinal manifestation (peripheral arthritis) was seen in 1 (9%) patient. Associated gallstone requiring cholecystectomy was seen in two (18.2%) patients. Eight (72.7%) patients required small bowel resection and anastomosis, while 1(9%) patient underwent a lymph node biopsy for diffuse small bowel involvement with a passable stricture. There was 1 (9%) patient with isolated transverse colon stricture requiring resection and anastomosis. One (9%) patient had perianal fistula, requiring fistulectomy, who later developed small bowel recurrence. Postoperatively, 2 (18.2%) patients in high risk group had recurrence at the anastomotic site within one year of surgery [Table/Fig-6]. They required initiation of anti-tumour necrosis factor (adalimumab) therapy. Remaining 8 (72.7%) patients (excluding one recurrence in perianal crohn’s) were of low risk group for recurrence, and had been under regular surveillance till date.
Discussion
Inflammatory bowel disease is a chronic non-specific disorder of unknown aetiology triggered by complex interaction of environmental exposure strong genetic susceptibility and dysregulated gut mucosal immune responses to luminal antigens. In the patients, IBD used to be the disease of western countries, areas of highest occurrence, but now for unknown reason, the incidence and detection is increasing in Asian countries and catching up with the west [1,8]. The rapid rise in IBD also includes middle age at onset (mean age-UC: 45.1 years; CD: 55 years) and higher incidence of pancolitis (42%) as seen in the present study.
In a review summarising the global epidemiology of IBD, the higher estimate of incidence of UC and CD per 100,000 person-years were reported to be 57.9 and 15.6 in Europe, 0.68 and 0.41 in Southern Asia, and 23.14 and 23.82 in North America in the years 1930-2008 respectively [4,9]. Similarly, a recent epidemiological study between April 2011 to March 2012, from 8 Asian countries, reported crude overall incidence of IBD, UC, and CD to be 1.37, 0.76, and 0.54 per 100,000 respectively, which was highest for China and India (countries surrounding Nepal) [10].
Hence, rise in incidence of IBD cases seen in neighbouring countries have paralleled in Nepal. This rapid rise may be multifactorial and could be attributed to environmental factor changes like lifestyle, diet, hygiene, childhood infections, lack of breastfeeding, exposure to helminthes, smoking, more exposure to antibiotics, proton pump inhibitors and psychosocial stress [2,11]. Similarly higher cases detection in the second period (2015-2017) in our setting can be attributed to increased healthcare and patient awareness, modern equipments and resources (chromoendoscopy, narrow band imaging endoscopes, capsule endoscope, CT/MR enterography). Moreover, the establishment of dedicated surgical gastroenterology unit in 2015, made access to the specialised team. The surgical team had been well versed with the clinical presentations, identifying the gross pathological specimen, and further assisting the pathologist to remain focused to identify the ailment.
Another possible explanation for the rising detection may be that the intestinal tuberculosis closely mimicks CD [12]. It used to be difficult to differentiate the two diseases in the endemic region like Nepal on the basis of clinical, endoscopical, radiological and histological characteristics. This led to therapeutic antituberculous therapy trial because CD-specific therapy (steroids, immunomodulators) can be disastrous if patient turned out to have tuberculosis [13]. But now with the rise in dedicated specialists in IBD field (clinicians and pathologists), and availability of CT/MR enterography helps frequently in differentiating the entity. In a recent meta-analytic Bayesian Model study by Limsrivilai J et al., for differentiating CD from tuberculosis, the findings that favored CD included male gender, haematochezia, intestinal obstruction, asymmetrical stricture and fibrofatty proliferation. Similarly, the findings that significantly favored intestinal TB included fever, night sweats, lung involvement, ascites, caecal involvement and short symmetrical strictures. The sensitivity, specificity, and accuracy for differentiating were 90.9%, 92.6%, and 91.8% respectively [14]. Based on the above model, in the present scenario, both entities were frequently differentiated by trained radiologists, pathologists and subsequently treated by the clinicians.
Recently, the need for surgical intervention may have decreased significantly over the last decades with the introduction of immunomodulators and biologic agents. The estimated colectomy rate and the overall cumulative risk of surgical intervention for UC and CD ranges between 3% to 17% and 30% respectively over a 10-year period [15,16]. However, in the present study, 36.3% of patients in UC group and almost all (100%) the patients in CD group required surgical intervention, though the sample size was small. The reason behind the higher need of surgical intervention may be because of the unrecognised symptoms leading to delayed presentation, inappropriate treatment by non-gastrointestinal specialists, middle age at presentation and the aggressive nature of the disease at presentation in our setting.
Limitation
This paper highlights the disease burden, clinical characteristics and surgical management of IBD patients in our centre at the Eastern region of Nepal, with the limitation of limited number of IBD patients.
Conclusion
Inflammatory Bowel Disease is no more a rare disease in a country like Nepal. With the global rise in incidence in Asian countries, there has been increased burden and more detection of IBD cases at our centre (9.5 cases/year in the second period vs 1.8 cases/year in the first period), with almost 36% of UC cases and almost all CD cases requiring surgical intervention, probably due to the aggressive disease profile among our patients. Although this was a small scale study from a single tertiary care centre of the Eastern Nepal, an ideal epidemiological study in a large population group involving many healthcare centres should be carried out to determine the real status of this disease.
* No 90-day postoperative mortality
* There were three (15.9%) patients with major postoperative complication (small bowel obstruction, ischaemic hepatitis and controlled Ileal pouch anal anastomotic leak) in UC group managed conservatively, and three (27.3%) patients (anastomotic leak) in CD group requiring re-exploration and stoma.
** Enterocutaneous fistula at stoma closure site, small bowel involvement in perianal chron’s following fistulectomy and Ileal stricture at ileocolic anastomotic site