The advent of implants has reduced the use of conventional dentures, but there are still many instances where conventional denture is the treatment of choice for various health and economic reasons. Poly methyl methacrylate is biocompatible, easy to process and easily available and therefore repeatedly used to fabricate denture bases. However, one major drawback of this material is the unfulfillment of the mechanical requirements of prosthesis [1].
In the year 1937, Walter Wright publicized Poly Methyl Methacrylate (PMMA) material as a denture base material and it has gained a lot of popularity subsequently [2]. Even though, numerous other materials such as light-activated urethane dimethacrylate and polystyrene were introduced, PMMA continued to remain as the favored choice for both partial and completely edentulous situations [1,3].
Failures of denture prosthesis using PMMA are commonly seen as fractures of the appliances due to fatigue or impact forces of mastication. These forces lead to a concentration of the stress around micro cracks formed within the material because of repeated submission of forces. Continuous force leads to the spread of cracks which diminishes the strength of the denture base and finally results in a midline fracture [1].
Various fillers such as fibres, rubbers, metal powder fillers etc., have been advocated to improve its physical properties. Amongst these, glass fibres have gained popularity because of their good aesthetic qualities and good bonding to polymers. They also improve the mechanical properties of acrylic resin, especially fatigue resistance, impact strength and flexural strength [4-8]. Incorporation of butadiene styrene to PMMA forms a chemically modified high impact denture resin. As its designation suggests, they have high impact resistance and therefore prevent breakage of the dentures. With the advent of nanotechnology, Silver Nanoparticles (AgNPs) have been synthesised which possess chemical, physical, and biological properties distinctive from those presented by outdated bulk materials. The addition of AgNPs have exhibited good biocompatibility and long standing anti-bacterial activity, due to a steady release of ions and low bacterial resistance [9,10].
Since both E-glass as well as silver nanoparticles cause changes in the physical properties of denture base resins, this study was conducted to compare the flexural strengths of various heat cure, high impact denture base resins when reinforced with silver nanoparticles and E-glass fibres.
Materials and Methods
This in-vitro study was conducted in the Department of Prosthodontics, Manipal College of Dental sciences, MAHE, Manipal, India, during the period of June 2016- June 2017. A total of 90 specimens of high impact, heat cure denture base resins were fabricated for testing of flexural strength [11]. Ethical clearance was obtained prior to the study from Manipal College of Dental sciences, MAHE, Manipal, India.
Steps Followed for the Study:
Preparation of the Master Die: Aluminum master die of dimension 65 x 10 x 3 mm3 was fabricated using a milling machine at Manipal Institute of Technology (MIT), Manipal in accordance with ISO 1567:1999, International organization for Standardization, 1999 for Denture Base Polymers [12].
Fabrication of Silicone Samples: The silicone samples were prepared using vinyl polysiloxane putty (Flexceed, GC India Pvt., Ltd.,). It was manipulated according to the manufacturer’s instructions and packed into the aluminum mold cavity and the flask was tightened and kept under 1000 psi in a hydraulic press (Presee, Sirio Dental SRL, Italy) for polymerisation of the vinyl polysiloxane. The putty specimens were retrieved after 15 minutes and the mould was repacked with putty in a similar manner.
Mold Fabrication: The recommended W/P ratio was used for class IV dental die stone (Kalrock, Kalabhai Karson Pvt., Ltd., Mumbai). The water was measured by an accurate graduated cylinder and weighing balance was used to weigh the powder. The measured amount of water and powder was hand mixed in a rubber bowl. The lower portion of the Kavo flasks (Kavo Dental GmbH, Germany) were filled with freshly mixed die stone and the silicone putty specimens were placed into the mixture [Table/Fig-1]. After the initial set, the stone was coated with separating media and left to dry. Upper portion of the flask was then filled with the second mix of stone. The lid of the flask was closed and the flasks were clamped allowing the stone to set. After the stone hardened, the putty specimens were retrieved, and the mold space was obtained to pack the denture base resins.
Preparation of mold space using silicone samples.

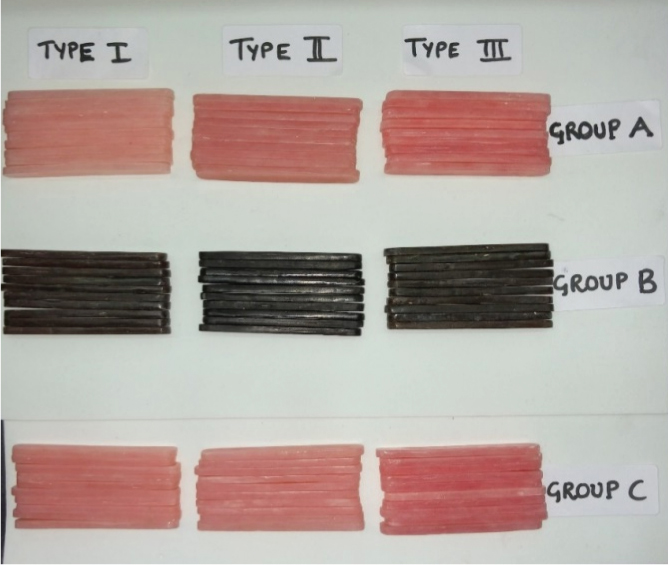
Selection and Manipulation of Denture Base Materials: Three types of high impact, heat cure denture base resins were used for this study and were further subdivided into 3 subgroups of 10 samples each [Table/Fig-2]. Each type of denture base material was manipulated as per manufacturer’s instructions [Table/Fig-3].
Three subgroups of each high impact denture base material.
| Groups | Composition |
|---|
| Group A | 100% PMMA (Control) |
| Group B | PMMA with 0.5% silver nanoparticles |
| Group C | PMMA with 2% E- glass fibres |
Three high impact, heat cure denture base resins selected for the study.
| Types | Brand of acrylic resin used | Polymer: Monomer ratio |
|---|
| Type 1 | Pink poly methyl methacrylate heat cure denture base resin, high impact (Acryl H, Pyrax Polymers, India) | 2.4g by weight of polymer and 1ml by volume of monomer |
| Type 2 | Pink poly methyl methacrylate heat cure denture base resin, high impact (Trevalon HI, Dentsply, Karnataka) | 2.5g by weight of polymer and 1ml by volume of monomer |
| Type 3 | Pink poly methyl methacrylate heat cure denture base resin, high impact (Acralyn H, Asian Acrylates, Mumbai) | 2.5g by weight of polymer and 1ml by volume of monomer |
Fabrication of the Samples: For Group A-Control Group, each type of material was mixed as per manufacturer’s instructions. When the mix reached the dough stage, the resin was packed into the mold space prepared prior using the silicone samples. The flask was then closed tightly and placed under uniform pressure of 2000 psi on a bench press for 30 minutes. Overnight bench curing was allowed and then the samples were acrylized using long curing cycle method as per manufacturer’s instructions for the individual types of acrylic resins. For Group B, 0.5% by weight of Silver Nanoparticles (AgNPs) (Aadarsh innovations, Pune) with a size of 30 nm were measured for the required amount of denture base resin. They were then added to the denture base resin powder and mixed meticulously to ensure uniform mixture with monomer. Following which the mixture was handled at dough stage and the samples were prepared in a similar manner as mentioned for group A. For Group C, 2% by weight of E-glass fibres (Goa glass fiber ltd., Goa) of 10 μm in diameter was weighed and added to monomer denture base resin. Then the required powder was added to it and mixed well. These fibres were chopped using a Bard-Parker knife No. 15 into 2 mm length approximately over a glass slab and added to the denture base resin and mixed thoroughly. The resin was kneaded for uniform distribution at its dough stage. Further preparation of the samples was done in a similar fashion as mentioned earlier. The cured samples were retrieved, cleaned and finished using dental burs. Final polishing of samples was done using pumice for one minute. The measurements of each sample were checked before subjecting them to testing [Table/Fig-4].
All 90 samples from each type with three subgroups each trimmed and polished for testing.
Testing of Samples for Flexural Strength: The samples were placed in a Universal Testing Machine (INSTRON 3366, Norwood USA), which subjected the samples to a 3-point bending test. Each sample was placed in a 50 mm – long support for 3-point flexural testing. A vertical load was then applied at the mid-point of the specimen at a crosshead speed of 5 mm/minute on a load testing machine. Load was applied until failure and fracture load was recorded in Newtons (N). All tests were performed under uniform atmospheric conditions of 23.0±10 C and 50±1% relative humidity [Table/Fig-5].
Mean of Maximum Flexure stress (Mpa) for control group (subgroup A), on addition of silver nanoparticles (subgroup B) and on addition of E-glass fibres (subgroup C) for three types of high impact, heat cure denture base resins.
| Groups(Resins) | Subgroups | Maximum Flexurestress (Mpa) |
|---|
| Type 1 | A- Control | Mean | 97.350000 |
| SD | 7.0798870 |
| B- Silver NPs | Mean | 94.264000 |
| SD | 12.4556192 |
| C- E-glass fibres | Mean | 97.338000 |
| SD | 4.0010188 |
| Type 2 | A- Control | Mean | 84.565000 |
| SD | 5.1537823 |
| B- Silver NPs | Mean | 87.789000 |
| SD | 7.7768852 |
| C- E-glass fibres | Mean | 96.500000 |
| SD | 7.3582848 |
| Type 3 | A- Control | Mean | 99.927000 |
| SD | 10.9429795 |
| B- Silver NPs | Mean | 100.356000 |
| SD | 7.4635443 |
| C- E-glass fibres | Mean | 104.333000 |
| SD | 9.0718809 |
*SD- Standard Deviation
† DBR- Denture base resins
Statistical Analysis
The data was analysed using SPSS version 20.0 (Statistical Package for the Social Sciences). Descriptive statistics was used to summarise the maximum flexure stress and flexure load at maximum flexure stress. One-way analysis of variance (ANOVA) test was performed to compare the flexural properties. For all tests p-value less than 0.05 was considered statistically significant. Dunnett’s test, a multiple comparison procedure to compare each of a number of treatments with a single control was used.
Results
The results obtained showed there was a difference in flexural strength between the three types of high impact, heat cure denture base resins but there was no significant difference between the subgroups of each type of denture base resin except type II denture base resin [Table/Fig-6]. In Type1 resin (Acryl H, Pyrax Polymars), the mean flexural strength decreased on addition of AgNPs and there was negligible decrease in strength on addition of E-glass fibres in comparison with the control group. In Type 2 resin (Trevalon HI, Dentsply), the addition of E- glass fibres to the denture base resin acquired the highest value in flexural strength amongst the subgroups. The difference in strength between group C (incorporated with E-glass fibres) and group A (Control) was of significance (p=0.001) [Table/Fig-7]. The difference in strength of the modified groups i.e., group B (incorporated with silver nanoparticles) and group C (incorporated with E-glass fibres) was significant only for Type 2 (p=0.022). Amongst Type 3-Heat cure denture base resin, high impact (Acralyn H, Asian Acrylates) subgroups, the difference in strength between them was not significant. It showed the highest result for mean flexural strength for all the three subgroups when compared to the subgroups in Type 1 and Type 2.
One-way ANOVA analysis to compare Maximum Flexure stress (Mpa) for the three different subgroups for 3 different types of high impact, heat cure denture base resins.
| DBR | Sum of Squares | Df | Mean Square | F | Sig. |
|---|
| Type-1 | Between Groups | 63.243 | 2 | 31.622 | 0.429 | 0.656 |
| Within Groups | 1991.479 | 27 | 73.758 |
| Type-2 | Between Groups | 762.400 | 2 | 381.200 | 8.100 | 0.002* |
| Within Groups | 1270.672 | 27 | 47.062 |
| Type-3 | Between Groups | 118.045 | 2 | 59.022 | 0.687 | 0.512 |
| Within Groups | 2319.771 | 27 | 85.917 |
* p-value less than 0.05 was considered to be statistically significant
† DBR- Denture Base Resins
The mean difference and standard error of Maximum Flexure stress (Mpa) amongst the various experimental groups when compared to the control group in each type of high impact, heat cure denture base resins.
| DBR | (I)Subgroup | (J)Subgroup | Mean Difference(I-J) | Std. Error | Sig. | 95% Confidence Interval |
|---|
| Lower Bound | Upper Bound |
|---|
| Type-1 | Silver NPs | Control | -3.0860000 | 3.8407933 | 0.640 | -12.048152 | 5.876152 |
| E-glass | Control | -0.0120000 | 3.8407933 | 1.000 | -8.974152 | 8.950152 |
| Type-2 | Silver NPs | Control | 3.2240000 | 3.0679610 | 0.479 | -3.934816 | 10.382816 |
| E-glass | Control | 11.9350000 | 3.0679610 | 0.001* | 4.776184 | 19.093816 |
| Type-3 | Silver NPs | Control | 0.4290000 | 4.1452971 | 0.992 | -9.243685 | 10.101685 |
| E-glass | Control | 4.4060000 | 4.1452971 | 0.472 | -5.266685 | 14.078685 |
* p-value less than 0.05 was considered to be statistically significant
† DBR- Denture Base Resins
Dunnett t-tests treat one group as a control and compare all other groups against it.
Discussion
Residual ridge resorption is an indispensable sequalae of tooth loss. Thus, as the age of the denture advances, it loses its adaptability. This maladaptive denture is subjective to excessive flexural stresses, which further increases during mastication. Darbar UR et al., and Vallittu PK et al., reported that accidental dropping was one of the major causes of denture fracture [13,14]. The most frequent site of fracture in the upper denture is the mid-line. During functional movements, denture base material is exposed to flexural deformation. An acrylic resin capable of supporting increased flexure along with resistance to recurring loading results in better success [15].
Physical and mechanical properties of prosthesis are greatly influenced and altered by the denture base material chosen, filler particles added and processing method involved in polymerisation. Rubber reinforced (butadiene-styrene polymethyl methacrylate) is now available in the market as high impact denture base resins (HI-PMMA) and has proven to increase the life of the dentures provided [16]. In comparison with the conventional denture base resins, they have improved toughness and good flow properties but shows increased haze and reduced tensile properties. Apart from this, other methods to improve the physical and mechanical properties of denture base materials is by reinforcement using filler material such as carbon fibres, aramid fibres, glass fibres, nanotubes, nanoparticles etc.
Glass fibres are often used for reinforcing polymers because of their good aesthetic quality and good bonding abilities with polymers. It has a high alumina, low alkali and low borosilicate content. It has high flexural strength and long-term stability against water and chemical substances. Alla RK et al., reviewed the addition of various types of fillers to PMMA and have stated that E-glass fibres are preferred over the others [1]. The addition of various concentrations of glass fibres to acrylic resins have been tested (1%, 2%, 5%, 10%, 15%) and was concluded that upto 2% concentration by weight, had increased the transverse strength and other mechanical properties. Further increase in concentration significantly reduced its strength [11,17]. Also, the fibres were incorporated in different forms such as chopped strand mat, woven, continuous, unidirectional etc. for comparative purposes and Unalan F et al., concluded in their study that the incorporation of chopped strand mat glass fibres in PMMA was the best form [18].
Denture stomatitis is another common problem with conventional acrylic removable complete dentures. Common association is seen with Candida species and affects the palatal mucosa with a homogeneous erythema [19]. Due to the emergence of many antibiotic-resistant micro-organisms, the use of antiseptics with silver as their base is gaining popularity. Silver has bactericidal effects to a broad spectrum of antimicrobial activities. The addition of silver in the form of nanoparticles has become a new form of interest in dentistry. Bajracharya S et al., investigated the candidal biofilm formation on denture bases which were heat-polymerised and incorporated with Silver Nanoparticles (AgNPs) in concentrations of 0.5%, 1% and 1.5% and it was observed that the flexural strength attained was within the limitations of ISO (≥65MPa) [20]. Sodagar A et al., confirmed that the addition of 0.05% AgNPs changed the flexural strength according to the brand of material used [21]. A study by Kassaee MZ et al., specified that inclusion of 0.5% AgNPs, increased the flexural strength as well as antibacterial effect. Therefore, we saw that the type of denture base resin used; amount and form of nanoparticles incorporated; polar interactions formed between C=O groups of both PMMA chains and silver nanoparticles are the vital aspects which affect the mechanical properties [22].
Thus, the aim of this study was to evaluate and compare the flexural strengths of three types of commercially available heat cure, high impact denture base resins reinforced with either silver nanoparticles or E-glass fibres.
The results obtained showed there was a difference in flexural strength between the three types of materials but there was no significant difference in between the subgroups of each type of denture base resin except Type II. In Type1- high impact, heat cure denture base resin (Acryl H, PyraxPolymars), the mean flexural strength decreased on addition of AgNPs and there was negligible decrease in strength on addition of E-glass fibres in comparison with the control group. Here the control group had the maximum strength and the difference in strength amongst the three subgroups was not significant. In accordance to study conducted in 1998 by Stipho HD [11]. The possible causes for negligible decrease in strength on addition of E-glass fibres may be due to clumping of glass fibers when mixed with monomer which lead to unequal distribution of fibres. Another possible reason may be improper adhesion between the fibers and the matrix or the nanoparticles and matrix. Silver nanoparticles have been known to decrease the strength of the denture base materials in accordance with the study conducted by Xia Y et al., which shows AgNPs can act as impurities and this could decrease the mechanical strength of the material in use. Due to the scattering of nanoparticles in acrylic matrix, there is a decrease in the reaction of monomer and leaving a lot unreacted monomer [23].
In Type 2-Heat cure denture base resin, high impact (Trevalon HI, Dentsply), the mean flexural strength increased on addition of AgNPs and was even higher in strength on addition of E-glass fibres in comparison with the control group. The addition of E- glass fibres to the denture base resin acquired the highest value in flexural strength amongst the subgroups. The difference in strength between the subgroups and between group C (incorporated with E-glass fibres) and group A (Control) was of significance (p=0.002). So was the difference in strength of the modified groups i.e., group B (incorporated with silver nanoparticles) and group C (incorporated with E-glass fibres) (p=0.022). Type 3-Heat cure denture base resin, high impact (Acralyn H, Asian Acrylates) showed the highest result for mean flexural strength for all the three subgroups when compared to the subgroups in Type 1 and Type 2. In Type 3, the mean flexural strength slightly increased on addition of AgNPs and was even higher in strength on addition of E-glass fibres in comparison with the control group. Although the difference in strength between the subgroups was not significant. This increase in flexural strength on addition of E-glass fibres can be explained in accordance to the study conducted by Vallittu PK et al., [24]. It states that the strengthening of the material is probably due to improved adhesion between fibres and resins which enhances the resistance of the resin. Increase in strength on addition of AgNPs can be explained in accordance to the study by Kassaee MZ et al., which suggested that addition of AgNps alters flexural strength of acrylic depending on the brand of resin material selected but can also be due to very high surface area of the nano particles in the resin matrix which is readily transformed from the matrix to the silver particles on application of stress [22].
In this in-vitro study, there was a significant difference in flexural strength amongst the Type 2 (Trevalon HI, Dentsply) subgroups. The contradictory increase and decrease in flexural strength of different types of denture base resins is similar to the results of the study conducted by Sodagar A et al., which demonstrated that the addition of AgNPs is dependent on the brands of resins used. However, the addition of E-glass fibres increased the strength in Type 2 (Trevalon HI, Dentsply) and Type 3 (Acralyn H, Asian Acrylates) but remained almost the same for Type 1 (Acryl H, PyraxPolymars, India), hence concluding that change in the flexural strength after incorporation of E-glass fibres, too depend on the brand of resin material used.
Limitation
Silver nanoparticles (AgNPs) and E-glass fibres used in the study were used in only one desirable concentration which was 0.5% and 2% respectively. The concentrations were selected based on the literature available which supports that these concentrations are biocompatible and non-toxic to the patient. AgNPs when used in a 0.5% concentration, led to a brownish discoloration which would not be an ideal choice for the aesthetic zones of the denture prosthesis. They could be used in the palatal plate region and buccal flanges of denture prosthesis as these regions are prone to denture stomatitis. Degree of polymerisation of the modified specimens which influences the mechanical properties was not recorded in the study. Further studies with the use of SEM analysis can be done for better understanding of the interaction of the particles.
Conclusion
Within the limitations of the in vitro study, it was found that the addition of E-glass fibres provided greater flexural strength in comparison to addition of silver nanoparticles. In this study Acralyn H denture base resin exhibited the greatest flexural strength with E-glass fibre incorporation. The addition of AgNP had no significant effect on flexural strength when compared to controls. The difference in strength of the modified groups was significant only for Trevalon HI. The change in mechanical properties is highly dependent on the brand of material used.
*SD- Standard Deviation
† DBR- Denture base resins
* p-value less than 0.05 was considered to be statistically significant
† DBR- Denture Base Resins
* p-value less than 0.05 was considered to be statistically significant
† DBR- Denture Base Resins
Dunnett t-tests treat one group as a control and compare all other groups against it.