An Unusual Case of Abdominoscrotal Swelling in a Young Patient-hydrocele En Bissac
Samida A Samad1, Suresh Vasant Phatak2
1 Resident, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
2 Professor and Head, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Samida A Samad, Resident, Department of Radiodiagnosis, Jawaharlal Nehru Medical College, Sawangi (Meghe), Wardha-442001, Maharashtra, India.
E-mail: samidasamad91@gmail.com
An abdominoscrotal hydrocele is a rare clinical entity in which there is a large hydrocele that extends from the scrotum into the abdominal cavity through the inguinal canal in an hourglass fashion. It is a condition usually affecting children and is infrequently seen in adults. Unilateral involvement is more common than bilateral. Authors hereby report an unusual presentation of abdominoscrotal hydrocele at an age of 27 years, presented with gradually progressing abdominal mass and bilateral scrotal swelling.
Abdominoscrotal mass, Computed tomography, Hourglass, Ultrasonography
Case Report
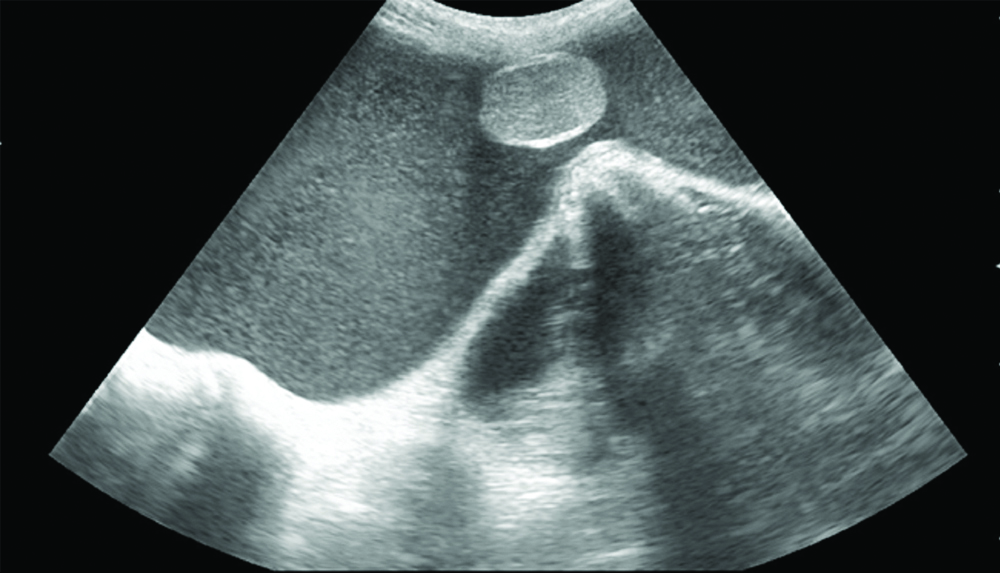
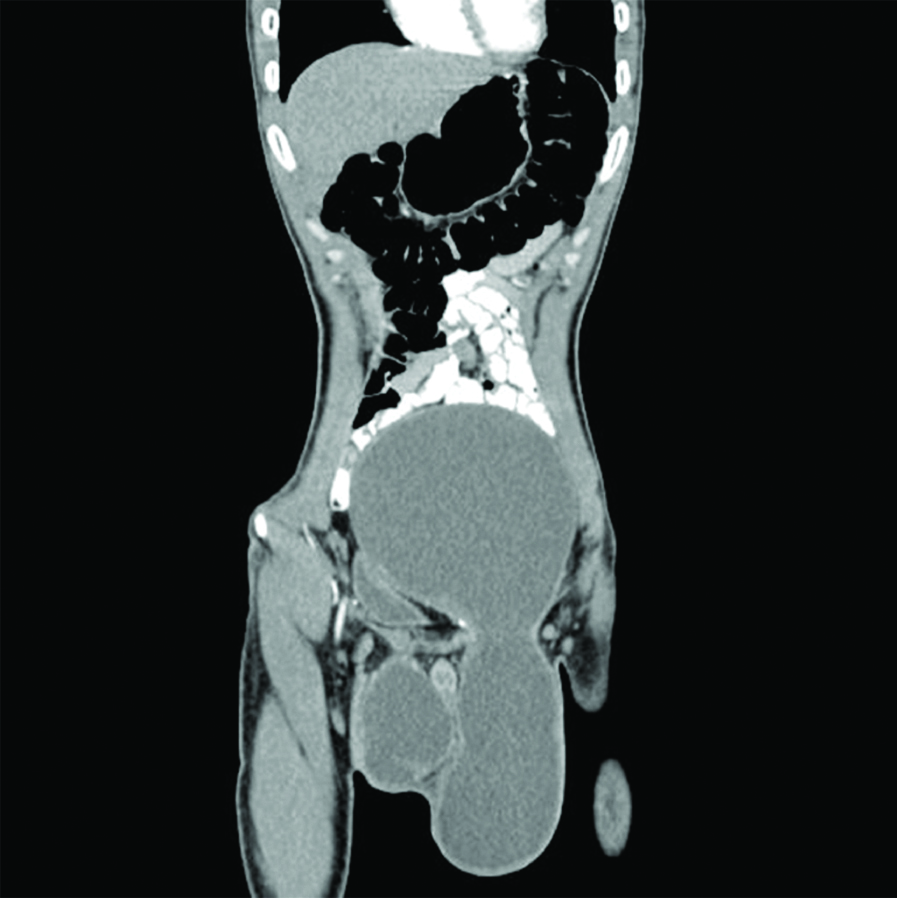
A 27-year-old male presented with bilateral scrotal swelling and gradually progressing abdominal distension since six months, there was no history of trauma, pain or retention of urine. On physical examination, a huge abdominal mass extending from the inguinal crease to costal margin was revealed along with bilateral scrotal swelling. The skin overlying swelling was shiny, oedematous. The scrotum was tense, and the swelling was cystic in consistency. There was no definite expansile cough impulse in the swelling. Swelling was measuring approximately 28×14×10 cm in its constricted area [Table/Fig-1]. It was an irreducible swelling, with non-palpable testis. Cross fluctuation was positive between abdominal and scrotal components. The patient underwent abdominoscrotal ultrasonography, revealed a large cystic mass measuring approximately 32×16×14 cm in the pelvis, separate from the urinary bladder and extending into the abdominal cavity. A clear fluid collection was noted in the tunica vaginalis along with the evidence of an anechoic abdominal fluid collection communicating with associated bilateral hydroceles with bilateral testes located in between abdominal and scrotal component [Table/Fig-2]. Based on these findings a sonographic diagnosis of abdominoscrotal hydrocele was made, which was later confirmed with computed tomography. Subsequent computed tomography demonstrated a well-defined large cystic lower abdominal mass extending into the scrotum through the inguinal canal [Table/Fig-3]. Through an inguinal approach, the cyst was decompressed and the abdominal component was dissected free from the urinary bladder, ureter and the peritoneum through the widened deep ring. Complete evacuation of fluid and excision of the sac with resection of tunica vaginalis was done [Table/Fig-4]. Postoperative course was uneventful.
A huge abdominal mass extending from inguinal crease to costal margin along with bilateral scrotal swelling.

Ultrasonography reveals an anechoic abdominal fluid collection communicating with associated bilateral hydroceles with testes located in between abdominal and scrotal component (left side).
Non-contrast computed tomography demonstrated a well-defined large cystic lower abdominal mass extending into the scrotum through the inguinal canal.
Intraoperative picture showing intra-abdominal extension of sac after decompression.

Discussion
Abdominoscrotal hydrocele was described for the first time by Dupuytrenas ‘hydrocele enbissac’ in 1934 [1]. Abdominoscrotal hydrocele is a rare clinical condition with large scrotal hydrocele communicates with abdominal component, through narrow inguinal canal in an hourglass fashion [1-3]. The aetiology of abdominoscrotal hydrocele is unknown. Different theories such as valve theory, diverticulum theory and displacement as per Laplace’s law have been described to explain the pathogenesis [2,4]. However, the most accepted theory is the one which suggests that the obliteration of processus vaginalis results in fluid accumulation in tunica vaginalis which results in increased intrascrotal pressure. When intrascrotal pressure exceeds the intra-abdominal pressure, inguinal portion of a large hydrocele is pushed into the low-pressure abdominal compartment through the inguinal canal, forming a dumbbell configuration with central constriction at the inguinal ring [4,5]. Abdominal part of ASH may extend into the retroperitoneum or preperitoneal space of Retzius. Sometimes abdominal component is so large that it may reach up to inferior pole of the kidney and causes pressure effects [5]. Most patients are asymptomatic except for the swelling as in the present case. However, occasional pain and bladder symptoms have been reported [3].
Diagnosis of an abdominoscrotal swelling can be made out clinically by performing cross fluctuation between scrotal and abdominal swelling, which is pathognomonic [1,3,4]. Further, the clinical diagnosis can be confirmed by ultrasonography using a multifrequency 3D transducer, which is the first imaging modality of choice to demonstrate the communication between scrotal and abdominal components [4,5]. Typically, ultrasound demonstrates encapsulated anechoic fluid collection extending from the abdomen to the scrotum through an inguinal ring [2,5,6]. Ultrasound can describe the testes as well, so that any abnormalities like testicular dysmorphism and ectopia can be ruled out [6]. Also, hydronephrosis or hydroureter if present, secondary to the pressure exerted by the abdominal component, can be picked up in ultrasonography [6]. Ultrasonography usually helps to eliminate misdiagnosis, especially when hydrocele is accompanied with tumours [7]. However, in selected cases ultrasonography may be inadequate and in these occasions contrast enhanced computed tomography could be used to demonstrate extension of the hydrocele through the inguinal canal into the abdominal cavity. Computed tomography scan is an appropriate imaging modality in patients with complex undiagnosed or difficult to diagnose cases of abdominoscrotal hydrocele on ultrasound [8]. Computed tomography may be helpful for more anatomical delineation cases and hourglass appearance of the communication can be demonstrated better [2,9]. MRI and injection of contrast into cyst are other modalities which help in the diagnosis [9]. The MRI evaluation gives valuable information over the extension of hydrocele and its effect on the underlying structures [3,8].
Gadelkareem RA, studied 579 abdominoscrotal hydroceles and he concluded that abdominoscrotal hydrocele affects paediatrics more than adults with a significantly increased rate of reporting in the last decades. He studied various hypothesis for aetiology and grouped according to the direction of fluid formation and hydrocele growth. He noted that most commonly associated congenital anomalies are contralateral hydroceles and cryptorchidism. Complications of abdominoscrotal hydroceles are as a result of compression, haemorrhage, infection, torsion, and coincident malignancy. A clinical grading system taking into consideration the increased anatomical, pathological or clinical complexities has been planned and provided two categories; simple and complex abdominoscrotal hydroceles with further sub-classes [1].
Parekh BR et al., conducted a study based on abdominoscrotal hydrocele and classified it as follows:
Complete abdominoscrotal hydrocele:
i) Indirect type; (ii) Direct type.
Incomplete abdominoscrotal hydrocele:
(i) Abdomino inguinal hydrocele (indirect/direct); (ii) Inguinoscrotal hydrocele [10].
There are various complications of the abdominoscrotal hydrocele which are mainly due to the pressure exerted by its components. A few of the complications include hydronephrosis, hydroureter, testicular dysmorphism (flattened and elongated or fusiform testis), testicular torsion, appendicitis, deep vein thrombosis, pedal oedema, haemorrhage of abdominoscrotal hydrocele and effect on spermatogenesis [6,9]. Rarely, the malignant transformation like mesothelioma due to neoplastic change in peritoneal lining can occur with abdominoscrotal hydrocele [9].
There is no role of conservative treatment, surgical excision of the sac is the only definitive treatment option [1,5,6,9]. Though several approaches have been recommended, total excision of the abdominoscrotal hydrocele or resection of tunica vaginalis with evacuation of fluid is commonly performed and often done through an inguinal approach [9,11]. Surgery can also be carried out laparoscopically through scrotal approach [9,12].
The inguinal hernia is the most common differential diagnosis [1,5,11]. Cystic lesions in the abdominal cavity should be differentiated from large hydronephrosis, polycystic kidney dysplasia, bladder diverticulum, and pelvic neuroblastoma [11,12].
Conclusion
While hydrocele is among the commonest inguinal anomaly in adult, its extreme form abdominoscrotal hydrocele is a rare condition of unclear aetiology. Abdominal masses connected with hydrocele need to induce a suspicion of this uncommon entity. ASH is associated with many complications ranging from the compression effect to coincident malignancies. The imaging features on both ultrasound and CT are characteristic, so the accurate diagnosis can be obtained, which help in patient management and prevention of complications associated with this condition. Before the era of modern imaging, diagnosis of abdominoscrotal hydrocele was based on clinical examination. Realtime ultrasonography has made it possible to diagnose confidently the abdominal extension, exact amount of fluid and its location. The diagnosis of clinically unsuspected cases has also become possible with modern imaging techniques like ultrasonography, computed tomography and MRI. In spite of the recent trends in treatment toward the less invasive approaches like laparoscopic techniques and conservation, still, surgical excision via the inguinal incision is the standard approach.
[1]. Gadelkareem RA, Abdominoscrotal hydrocele: A systematic review and proposed clinical gradingAfrican Journal of Urology 2018 24(2):83-92.10.1016/j.afju.2018.01.006 [Google Scholar] [CrossRef]
[2]. Singh G, Pandey A, Verma A, Gupta A, Abdominoscrotal hydrocele: A rare cause of a cystic abdominal mass in childrenFormos J Surg 2018 51(2):88-90.10.4103/fjs.fjs_110_17 [Google Scholar] [CrossRef]
[3]. Srinivasan R, Drage M, Olsburgh J, Management of Abdominoscrotal hydrocele (ASH)/Scrotal-Inguino-Retroperitoneal (SIR) hydrocele in a renal transplant patientJournal of Surgical Case Reports 2017 2017(10):rjx20310.1093/jscr/rjx203 [Google Scholar] [CrossRef]
[4]. Kamble PM, Deshpande AA, Thapar VB, Das K, Large abdominoscrotal hydrocele: Uncommon surgical entityInternational Journal of Surgery Case Reports 2015 15:140-42.10.1016/j.ijscr.2015.08.02726363104 [Google Scholar] [CrossRef] [PubMed]
[5]. Czerwińska K, Brzewski M, Majkowska Z, Mosior T, Roszkowska-Blaim M, Warchoł S, The abdominoscrotal hydrocele in the infant-case reportPolish Journal of Radiology 2014 79:108-11.doi:10.12659/PJR.89014810.12659/PJR.89014824847392 [Google Scholar] [CrossRef] [PubMed]
[6]. Blackwell RH, Kouri A, Ellimoottil C, Bresler L, Turk TMT, Massive Abdominoscrotal HydroceleCurrent Urology 2013 7(2):110-12.10.1159/00035625924917769 [Google Scholar] [CrossRef] [PubMed]
[7]. Huang SS, Wu DL, Gui YP, Zhao X, Xie H, Diagnosis and treatment of yolk sac tumor of the testis with hydrocele in children: report of 7 casesZhonghua Nan Ke Xue 2013 19(11):1007-10. [Google Scholar]
[8]. Walker MR, Ernest AJ Jr, McMann LP, Hydrocele: an atypical presentation of metastatic sarcomatoid renal cell carcinomaCan J Urol 2011 18(3):5742-44. [Google Scholar]
[9]. Halilbasic A, Hotic N, Skokic F, Husaric E, Rahmanovic E, Halilbasic M, Both-sided large abdominoscrotal hydrocele associated with testicles atrophyMed Arh 2011 65(3):182-84.10.5455/medarh.2011.65.182-18421776885 [Google Scholar] [CrossRef] [PubMed]
[10]. Parekh BR, Reinboth G, Mishra CP, Abdomino-scrotal hydroceleBr J Surg 1975 62:629-32.10.1002/bjs.18006208111174803 [Google Scholar] [CrossRef] [PubMed]
[11]. Rasalkar DD, Chu WCW, Mudalgi B, Paunipagar BK, Abdominoscrotal hydrocele: an uncommon entity in adults presenting with lower abdominal and scrotal swellingJournal of the Hong Kong College of Radiologists 2009 12(2):76-78. [Google Scholar]
[12]. Tiwary SK, Kumar S, Agarwal A, Khanna R, Khanna AK, Abdomino-scrotal hydrocele in 35-year-old: A case reportKathmandu University Medical Journal 2007 5(18):237-39. [Google Scholar]