Idiopathic Photodermatosis are a group of skin diseases caused by chronic exposure to Ultra-Violet Radiations (UVR). UVR are part of the electromagnetic spectrum, and are of special interest to dermatologists as many skin disorders are caused by these wavelengths. The UV range (200–400 nm) is subdivided into UVA (320–400 nm), which is not visible to human eyes; UVB (290-320 nm), often referred to as sunburn spectrum and is biologically most active wavelengths reaching earth surface and UVC (200 to 290 nm) [1]. UVB forms 1% of the UVR reaching the earth and is highly energetic, while UVA forms 99% of UVR reaching the earth and is lower in energy [2]. The effects on skin are due to various biochemical mediators like IL-1, IL-10, serotonin, histamine, by-products of arachidonic acid metabolism etc released from keratinocytes, mast cells and other inflammatory cells [3]. The immunological changes result from effects on Langerhans cells, suppressor and other subtypes of T cells and release of cytokines like IL-1 and IL-6 [4,5].
The morphology of skin lesions varies considerably ranging from micropapules or papules to violaceous papules or plaques and lesions may be hypopigmented, skin coloured or hyper-pigmented. Condition may be acute or chronic and common presenting symptoms are intense itching, local swelling, burning sensation, blister formation or even peeling of skin. The usual sites of lesions are photoexposed areas of neck, upper limbs and face. These lesions are usually benign but cause cosmetic concerns to patient.
The most common type of idiopathic photodermatosis is PMLE. Other less common types are Actinic prurigo, Chronic actinic dermatitis, Solar urticaria and Hydroa vacciniforme. Histopathology depends on the age of the lesion and various patterns are spongiotic, lichenoid, psoriasiform or perivascular infiltrate [6,7]. PMLE which is most common type of idiopathic photodermatosis is common in the first three decades of life and females are more often affected than males. The mean age in females and males is 33 years and 35 years respectively [8].
The aim of this study was to study the clinical and histopathological patterns of photodermatosis and to correlate between the clinical and histopathological findings.
Materials and Methods
In this cross-sectional observational study, 100 consecutive cases of photodermatosis attending the Department of Skin and VD of tertiary care hospital, North India over a period of two years from October 2014 to June 2016, were included after getting approval from ethical committee of our institution.
All cases of idiopathic photodermatosis attending the dermatology clinic with fresh lesions irrespective of age, sex, associated diseases and who were not on treatment were included. All non-idiopathic photodermatosis cases due to metabolic disorders, genetic disorders and exogenous (drugs) and patients not willing to participate in the study were excluded.
The clinical history like age, sex, duration of the disease, site of lesion, any associated systemic disease and history of drug intake etc were noted in a pre-tested and pre-designed proforma after taking informed and written consent. Diagnosis was established by history and clinical examination. Elliptical incisional biopsies under local anaesthesia were taken from well developed lesions under aseptic conditions after taking consent.
Results
Age of the cases varied from minimum of 10 years to 70 years with average age being 41.5 years. Among them, 49% were males and 51% were females and all patients were divided into four age groups. Maximum number (20/51) of female patients presented in the age group 26-40 year while 14 female cases presented in the age group 41-55 year. In comparison most male cases (16/49) presented in the older age group of 56-70 year followed closely by 13 presenting in the age group 41-55 year.
Multiple photo-exposed sites were involved and many patients had more than one site affected at the time of presentation. Lesions on photoexposed parts of upper limbs (the dorsum of forearm and hand) were present in 95% patients. Face involvement was seen in 21% patients while neck and trunk in 51% and 15% respectively.
The most common symptom was itching, seen in 98% patients followed by burning in 46% patients. Erythema was present in 48% patients while oedema and induration was seen in 6% and 2% respectively. Seventy patients had their lesions start in summer season. Spring was distant second with 13 cases followed by winter with 12 cases and 5 occurring in autumn.
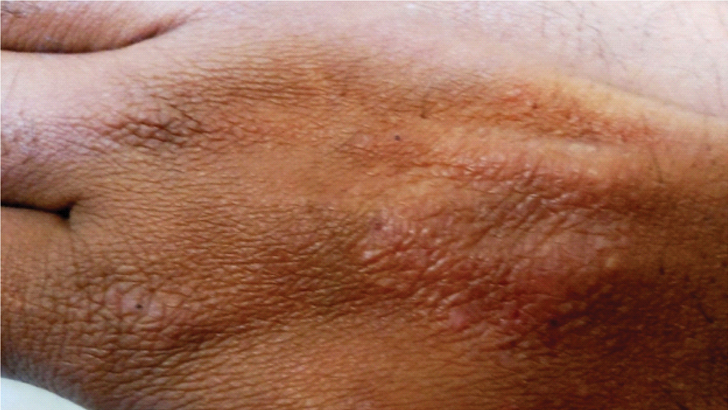
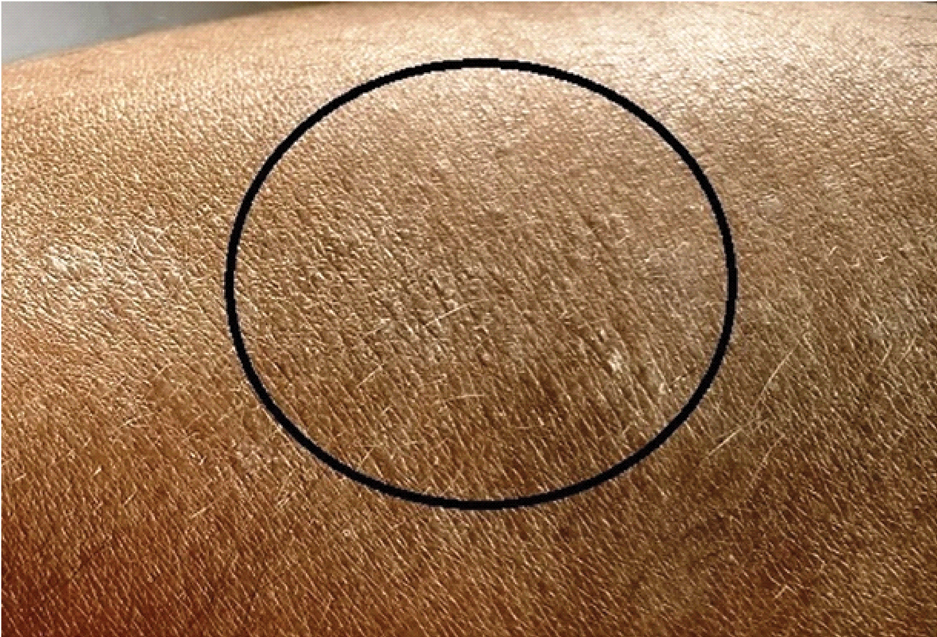
Majority of the patients presented with lesions of multiple morphologies. Papular [Table/Fig-1] and micropapular [Table/Fig-2] lesions were most common presenting lesions, present in 53 and 58 patients respectively. Many patients had micropapular and papular lesions coexisting in the same patient. Plaques were present in 17 patients either alone or in combination with other morphologies.
Photolichenoid eruptions on dorsum of hand.
PMLE: Multiple skin coloured micropapules on the dorsal aspect of forearm.
Hyperpigmented lesions were the most common, presenting in 60% cases and lesions with violaceous hue were present in 26%. Lesions were hypopigmented in 9% while skin coloured lesions were found in just 5% cases. In 97 cases the clinical diagnosis was PMLE [Table/Fig-3].
PMLE: Lichenoid plaques on the photoexposed parts of neck.

There were only two cases of Chronic Actinic Reticuloid (CAD) [Table/Fig-4] and one of Solar Urticaria (SU). No cases of Actinic prurigo and Hydroa vacciniforme were seen.
Actinic Reticuloid:- Multiple erythematous & violaceous indurated plaques on the face of 70-year-old patient.

Ten cases were found to be associated with other diseases. Three were known cases of diabetes mellitus, two had hypothyroidism, two were using hair dye, and one each of hypertension, HIV and cement allergy.
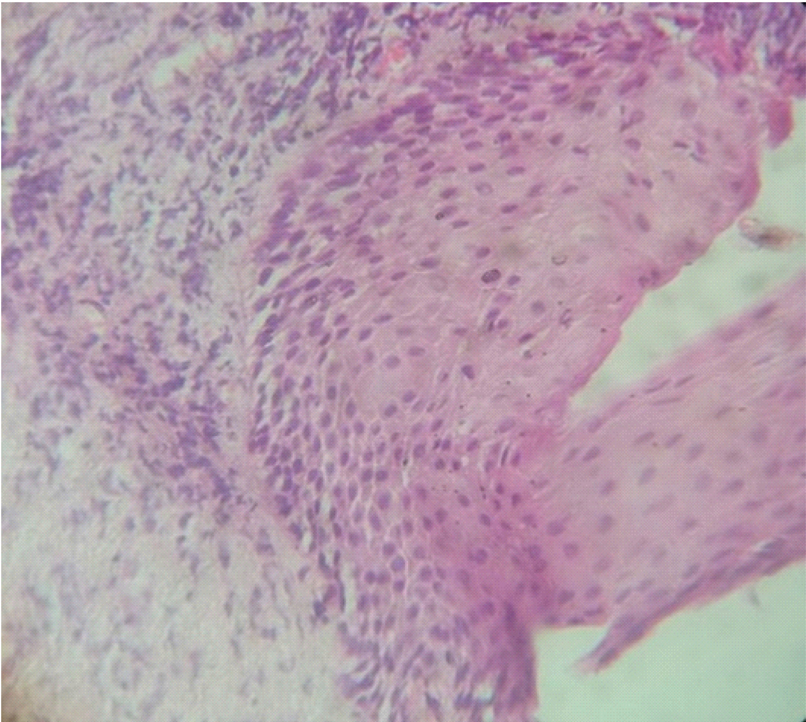
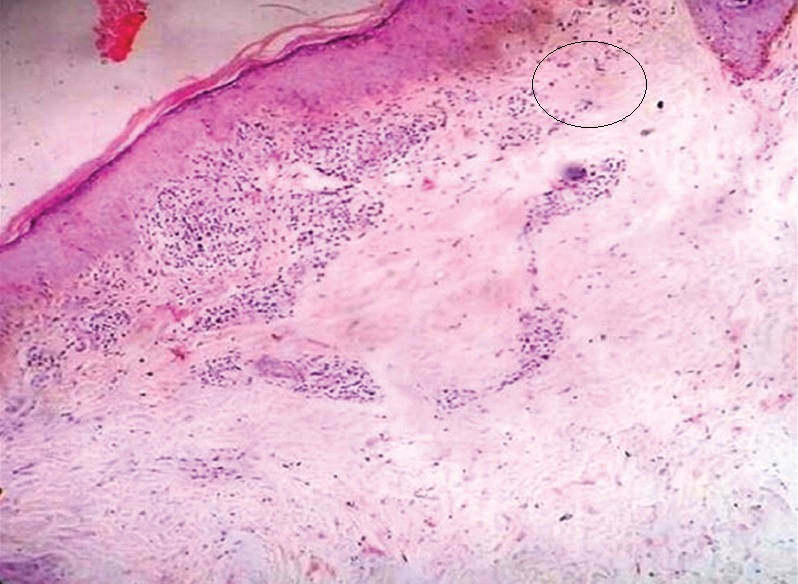
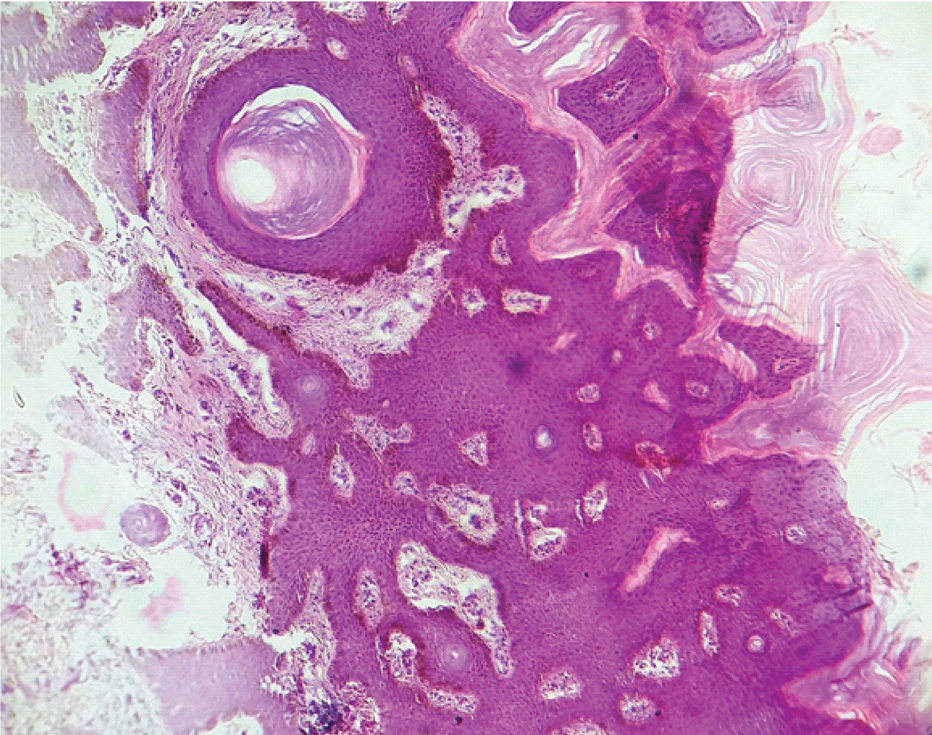
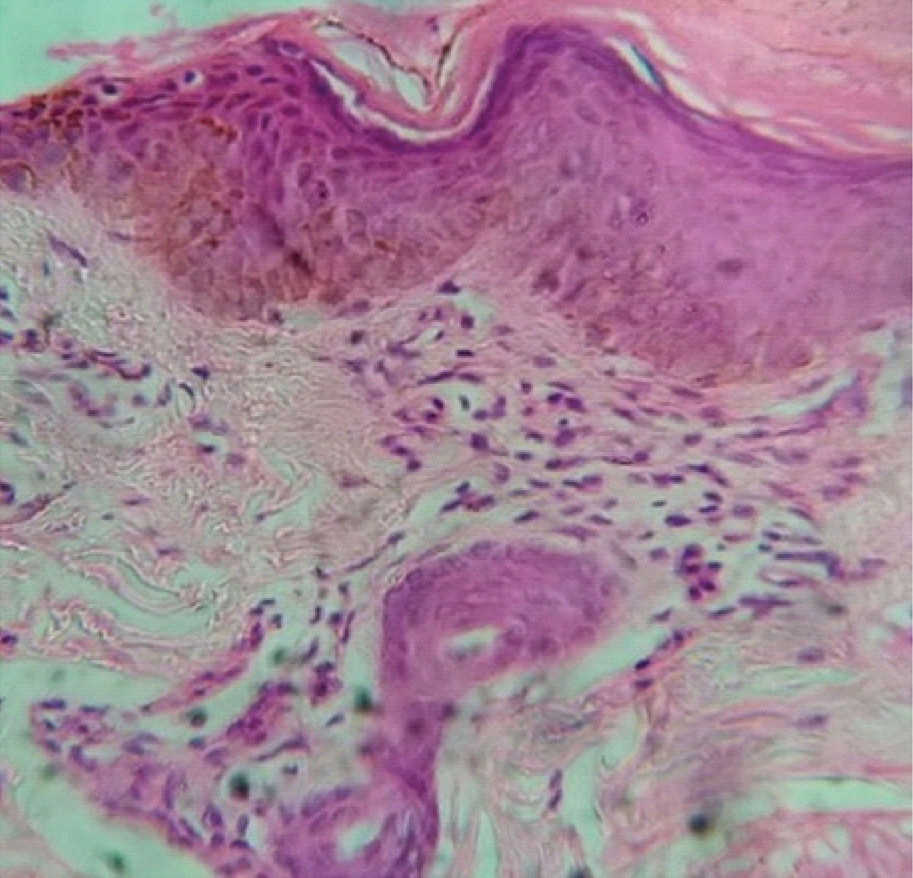
The most common histology pattern observed was spongiotic pattern [Table/Fig-5a,b], seen in 46% cases. This was followed by lichenoid in 27% [Table/Fig-6] and psoriasiform [Table/Fig-7] in 18% cases. Perivascular pattern [Table/Fig-8] was present in only 4% cases and in 5% cases the pattern was non-specific.
Spongiotic pattern: marked spongiosis along with acanthosis and superficial inflammatory infiltrate. (H&E,100X).
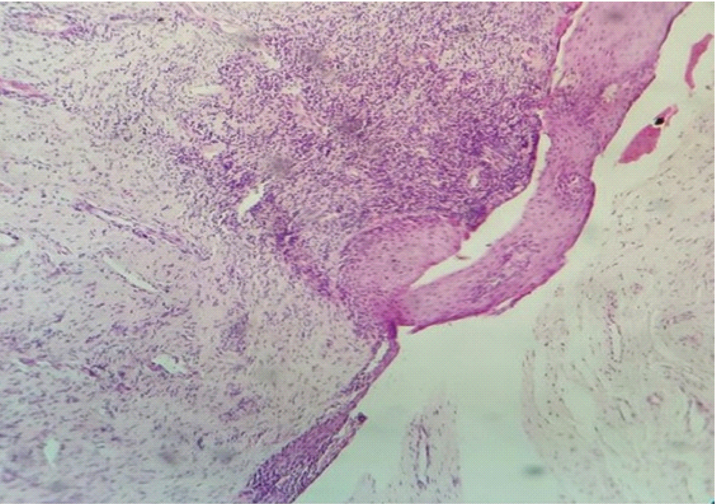
Spongiotic pattern: marked spongiosis along with acanthosis and superficial inflammatory infiltrate. (H&E, 400X).
Lichenoid pattern:Mild hyperkeratosis along with pigmentation incontinence (encircled area) and lichenoid band like infiltrate in superficial dermis. (H&E,100X).
Psoriasiform pattern: Marked hyperkeratosis along with mild spongiosis. (H&E, 100X).
Perivascular pattern: Mild hyperkeratosis and spongiosis and deep perivascular inflammatory infiltrate. (H&E, 400X).
In majority cases (97/100) clinical diagnosis made was PMLE and among these, the most common pattern seen on histology was spongiotic. The p-value between clinical and histopathological patterns was found to be statistically significant (p= 0.002) and thus a positive correlation could be drawn between clinical and histo-pathological diagnosis in patients diagnosed to have PMLE [Table/Fig-9]. Both of the patients diagnosed clinically as CAD showed lichenoid pattern on histology and the patient with SU had non-specific findings on histopathological examination.
Clinico-histopathological correlation.
| Spongiotic | Lichenoid | Psoriasiform | Perivascular | Other/Non-specific | Total | p-value (X2) |
|---|
| PMLE | 46 (47.42%) | 25 (25.77%) | 18 (18.56%) | 4 (4.12%) | 4 (4.12%) | 97 (100%) | 0.002 (25.3) S |
| CAD | 0 (0%) | 2 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (100%) | 1.000 (0.00) NS |
| SU | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (100%) | 1 (100%) | 1.000 (0.00) NS |
The p-value in both these groups was found to be non significant (p=1).
Discussion
In this study of 100 cases, the female and male ratio was 1.04:0.96 and their mean age was 41.5 years. There were more number of middle aged male attending our OPD with PMLE. This might be due to the fact that Punjab is agriculture based state and male farmers are chronically photoexposed while working in their fields. Duration of the disease was less than a month to maximum of 60 months at the time of presentation.
In comparison, in the study conducted by Khaitan B et al., there were 48 females, and 24 males with mean age of 29.2±10.4 years (range 12-65 years) [7]. The mean age at onset was 27.1±10.4 years (range 9-64 years) while duration of disease ranged from 15 days to 17 years (mean: 2.2 years).
In the study conducted by Bedi TR on 25 Indian patients clinically diagnosed with Summertime Actinic Lichenoid Eruption (SALE), there were 75% female cases in their 2nd to 4th decade [9]. Their ages varied from 8 to 50 years with mean age of onset being 26.36. In the study conducted by Chen YA et al., on 34 Taiwanese patients the male:female ratio was 1:1, mean age 33.5 years and age range was 9–62 years while in a study by Chiam LY et al., there were 14 (66.7%) males and seven (33.3%) females. The mean age of presentation was 28 years and duration of disease was 0.5 months to 10 years [10,11].
In this study itching was present in 98% of cases while in the study conducted by Khaitan B et al., itching was mild in 31 (43.1%) patients, moderate in 30 (41.7%), severe in 10 (13.9%) and absent in a patient [7]. In a study by Bedi TR 88% patients had itching and burning as their main symptoms [9].
In present study, upper limbs involvement was seen in 95% of cases, neck involvement in 51%, face in 21% and trunk in 15% of cases which correlated very well with other studies. In the study conducted by Khaitan B et al., the most common site of onset was forearms in 47.2% cases, followed by nape, sides of the neck and upper back in 32%, face in 11%, dorsa of hands in 4%, and arms 4% [7]. (Upper limb involvement was seen in 57% of cases).
In the study by Bedi TR photoexposed parts of upper limbs were involved in 96%, neck in 40% and upper back in 20% cases [9]. In the study by Chiam LY et al., arms and forearms involvement was seen in 95% cases while face and neck involvement was seen in 48% [11].
In this study, 83% cases presented in summer and spring seasons and rest in winter and autumn seasons showing strong correlation with the study conducted by Khaitan B et al., in which 80% had onset in summer, early rainy season and spring season while 9.7%, had onset in autumn and winter season [7]. Also in the study by Bedi TR 100% of cases noticed their first lesion in summer months [9].
In this study, micropapular lesions (1-2mm) were seen in 53%, papular in 58% and plaque type lesions in 17% while in the study conducted by Khaitan B et al., the eruption also consisted of papules and plaques [7]. Both papules and plaques were predominant in 34.7% cases each. Among them, 9.7% had only papules while 1.4% patient had plaques alone. Papules were ranging in size from 1-2 mm (micro papules) in 66.2% to 2-4 mm in 33.8% cases.
In this study, PMLE was commonest clinical diagnosis made (97%) but in a study by Kerr A et al., photodermatosis was studied in African Americans and Caucasians and frequency of PMLE was 67.4% and 41.1%, respectively [12]. The reason for higher frequency of PMLE in present study may be that this part of India has agriculture based economy and population work in fields for long hours thus exposing themselves to photodermatosis.
In this study, spongiotic pattern was seen as most common, observed in 46% patients. Biopsies revealed parakeratosis, spongiosis, acanthosis, exocytosis of lymphocytes and histiocytes and oedema of dermal papillae with an infiltrate of lymphocytes and histiocytes. Lichenoid pattern was present in 27% patients. There was thinning of epidermis with mild parakeratosis, basal cells show vacuolization, melanin incontinence and lichenoid infiltrate in band like pattern.
A total of 18% patients had psoriasiform pattern, showing compact hyperkeratosis with bulbous rete pegs and some degree of papillary fibrosis in few cases. Perivascular pattern was seen in 4% and other/non-specific in rest of 5% cases. The severity of the changes varied in the biopsies.
So these results had strong correlation with the study conducted by Khaitan B et al., in which three common specific histopathological patterns were observed: spongiotic (43.7%), lichenoid (22.5%), psoriasiform (18.7%) and fourth less common perivascular pattern in 5% [7]. Even in other studies the most common histological pattern was found to be spongiotic followed by lichenoid pattern [9,10].
Conclusion
This observational study correlates various cases of photodermatosis with associated histopathological patterns. Young females in their 2nd to 4th decade are more commonly affected with photodermatosis and micropapular and papular lesions are more common. Middle aged males also contributed in significant number as they work in agricultural fields for long hours under sun. Also, population in North India may be at high risk for photodermatosis because they expose their skin in spring and summer to sun after the end of winter season when their skin is fully covered.
In the present study, PMLE was the most commonly diagnosed subtype of photodermatosis. All diagnosis made clinically were proved to be true by histolpathological findings. It is found that spongiotic pattern is most common histopathological pattern associated with photodermatosis, as photodermatosis is a type of eczema and spongiosis on histopathology signifies eczematous change. Depending on the duration of lesion early lesions shows spongiotic or licehnoid pattern whereas the late lesions start showing psoriasiform changes.