The Prognostic Value of ANGPTL-4 in Acute Coronary Syndrome: A Prospective Cohort Study
Luxitaa Goenka1, Ritwika Sinha Ray2, Vengatesh Munnusamy3, VE Dhandapani4, Melvin George5
1 Clinical Research Associate, Department of Clinical Pharmacology, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
2 Clinical Research Intern, Department of Clinical Pharmacology, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
3 Associate Professor, Department of Cardiology, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
4 Professor and Head, Department of Cardiology, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
5 Assistant Professor, Department of Clinical Pharmacology, SRM Medical College Hospital and Research Centre, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Melvin George, Assistant Professor, Department of Clinical Pharmacology, SRM Medical College Hospital and Research Centre, Kattankulathur, Kancheepuram, Chennai-603211, Tamil Nadu, India.
E-mail: melvingeorge2003@gmail.com
Introduction
Coronary Artery Disease (CAD) is one of the leading causes of mortality and morbidity worldwide and Acute Coronary Syndrome (ACS) is one of the predominant causes of Cardiovascular Deaths (CVD).
Aim
To determine if Angiopoietin-like Protein-4 (ANGPTL-4) might be a potential predictor of Major Adverse Cardiac Events (MACE) in ACS patients.
Materials and Methods
This prospective cohort study was conducted in the Department of Cardiology and Clinical Pharmacology, SRM MCH and RC, Kattankulathur, between January 2016 and March 2018. Authors measured serum ANGPTL-4 at admission in 120 ACS patients using Enzyme-linked Immunosorbent Assay (ELISA) with a commercially available (Ray Biotech Human ANGPTL-4 ELISA, GA, USA) kit. The patients were followed up through a telephonic interview to record MACE. Independent Samples t-test and chi-square test were used to compare the differences in the continuous and categorical data, between the groups respectively. Receiver Operating Curve (ROC) was plotted to predict the ability of ANGPTL-4 to predict MACE among ACS patients. Kaplan-Meier survival analysis was performed and the survival rate between those with high and low ANGPTL-4 levels was compared using the log-rank test. All statistical analyses were performed with SPSS version 16.0 (SPSS Inc., Chicago, IL). All p-values<0.05 were considered statistically significant.
Results
A total of 120 ACS patients were included for the study. During the median follow-up of 24 (22-25.75) months, MACE had occurred among 14 patients. Ten patients were lost to follow-up. Kaplan Meier survival curve was plotted for patients with low and high ANGPTL-4 levels and the log-rank test failed to show a significant difference in the survival rate between the two groups (χ2=0.100, p=0.75). ANGPTL-4 failed to show any significant difference in the survival rate in both diabetic (χ2=0.002, p=0.97) and hypertensive (χ2=0.002, p=0.96) ACS patients.
Conclusion
In conclusion, the present study data failed to demonstrate that ANGPTL-4 could be a potential biomarker for the prediction of MACE among ACS patients. However, larger studies are warranted to investigate the prognostic value of ANGPTL-4 among ACS patients.
Angiopoietin-like protein 4, Cardiac events, Prognostication
Introduction
Coronary artery disease is one of the leading causes of mortality and morbidity worldwide and ACS is one of the predominant causes of CVD. The highest number of CVD below the age of 70 years has been reported in 52% of the India population as compared to 23% of the western population [1]. The prevalence of CAD in South India is approximately 11% and the age-standardised prevalence was found to be 9% [2]. The term ACS refers to a range of acute myocardial ischaemic states comprising of Unstable Angina (UA), ST-Segment Elevation Myocardial Infarction (STEMI) and Non-ST Segment Elevation Myocardial Infarction (NSTEMI) [3]. In the current clinical practice, the diagnosis of ACS is based on the presence of clinical symptoms, Coronary Angiography (CAG), echocardiography parameters, electrocardiogram parameters and laboratory investigations [4,5]. Several traditional risk assessment tools such as Global Registry of Acute Coronary Events (GRACE) risk score, SYNTAX score and Thrombolysis in Myocardial Infarction (TIMI) risk score are available to measure the severity and prognostic value of the disease. However, the utilisation of these traditional risk scores to predict MACE are limited due to their variable sensitivities and specificities; leading to concerns regarding the validity and reliability of these clinical risk scores [6].
Angiopoietin-like Protein-4 (ANGPTL-4) is a newly emerging circulatory biomarker that is being studied extensively in CVD. This circulatory biomarker is a multifunctional protein which takes part in the process of inflammation, angiogenesis, energy metabolism and lipid regulation. Lipoprotein Lipase (LPL) is the primary enzyme that hydrolyses lipoprotein triglycerides and phospholipids in Toll-Like Receptors (TLRs) resulting in release of free fatty acids and monoglycerides. The acute phase protein ANGPTL-4 inhibits the enzyme lipoprotein lipase that hydrolyses triglycerides and phospholipids. Therefore, it can be hypothesised that ANGPTL-4 has a strong association with the development of atherosclerosis [7-9]. The relationship between the levels of ANGPTL-4 and cardiometabolic traits has been studied extensively in animal models; however, the data on human population is sparse [10,11]. Therefore, the primary objective of this prospective cohort study was to determine if ANGPTL-4 might be a potential predictor of MACE in ACS patients. The secondary objective was to determine if ANGPTL-4 can predict MACE among diabetic and hypertensive ACS patients.
Materials and Methods
This prospective cohort study was conducted in the Department of Cardiology and Clinical Pharmacology, SRM MCH and RC, Kattankulathur, between January 2016 and March 2018. The study was approved by the SRM Institutional Ethics Committee (IEC), India (664/IEC/2014), SRM Medical College Hospital and Research Centre, Kancheepuram and all study procedures were performed in accordance with the provisions of the Declaration of Helsinki. Written Informed consent was obtained from all the patients who participated in the study.
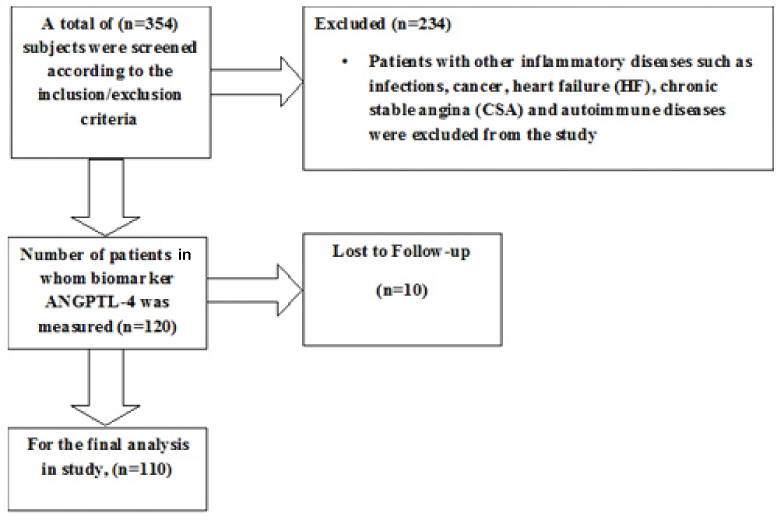
Study population: The study group comprised of consecutive patients who presented with ACS and were hospitalised in the Department of Cardiology between January and August 2016. Patients above 18 years of age, of both gender and willing to give informed consent and comply with all study-related procedures, were included in the study. ACS patients comprised of both STEMI and NSTEMI/UA. The condition STEMI was defined as a clinical syndrome with the presence of clinical symptoms associated with myocardial ischaemia, a constant ST elevation and release of biomarkers associated with necrosis [12]. NSTEMI/UA was defined as a clinical syndrome where there is a persistent absence of ST elevation and the release of necrotic markers [13]. Patients with other inflammatory diseases such as infections, cancer, Heart failure (HF), Chronic Stable Angina (CSA) and autoimmune diseases were excluded from the study [Table/Fig-1].
Flow chart illustrating the recruitment process.
Laboratory investigations: From each patient, 4 mL of peripheral blood was collected from the vein in the forearm prior to CAG in an Ethylenediaminetetraacetic Acid (EDTA) coated vacutainer tubes within 48 hours of admission in the cardiac intensive care unit. After adequate centrifugation at 2500 revolutions per minute (rpm) for 10 minutes, the serum samples were extracted and were stored at -80°C in deep freezer. The level of Serum ANGPTL-4 was estimated using ELISA with a commercially available (Ray Biotech Human ANGPTL-4 ELISA, GA, USA) kit. The inter and intra assay coefficient of variation was 8.8% and 8% respectively. The laboratory measurements were performed in a blinded manner and the investigators performing the assay were unaware of the patient diagnosis.
Follow-up: The patients were followed up through a telephonic interview to record MACE. MACE was defined as cardiovascular mortality, re-hospitalisation, recurrent MI, cerebrovascular diseases and CABG [14].
Statistical Analysis
The normality of data for continuous variables was checked using Q-Q plot in SPSS. Continuous variables were summarised as the mean±standard deviation (SD) or median (IQR) and categorical data were expressed as frequency with percentages. Differences in the categorical variables between groups were evaluated using the chi-square test. Parametric or non parametric tests were used based on the distribution of data. The differences in continuous variables between groups were analysed with Independent samples t-test based on the normality of data. The optimal cut-off level of ANGPTL-4 to predict MACE in ACS patients was evaluated using the area under the ROC curve. Kaplan-Meier survival analysis was performed and the survival rate between those with high and low ANGPTL-4 levels was compared using the log-rank test. All statistical analyses were performed with Statistical Package for the Social Sciences (SPSS) software version 16.0 (SPSS Inc., Chicago, IL). All p-values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of study patients: The study sample comprised of ACS patients namely NSTEMI/UA (n=63) and STEMI (n=57). The study patients were compared for characteristics such as age, gender, diabetes mellitus, hypertension, smoking habits, dyslipidaemia, and family history of coronary artery disease, renal disorders and sedentary lifestyle [Table/Fig-2]. In comparison, the study showed no significant differences in study characteristics like age, laboratory parameters and clinical risk factors.
Baseline characteristic of study patients.
| Variables | STEMI (n=57) | NSTEMI/UA (n=63) | p-value |
|---|
| Age, years | 55.39±11.88 | 54.10±9.76 | 0.518 |
| Blood Glucose, mg/dL | 166.06±64.92 | 167.45±80.11 | 0.924 |
| Blood Urea, mg/dL | 28.58±13.25 | 24.82±8.80 | 0.078 |
| Serum Creatinine, mg/dL | 0.90±0.24 | 0.84±0.29 | 0.184 |
| Haemoglobin, g/L | 13.64±2.18 | 13.40±1.55 | 0.492 |
| pcv | 40.38±5.50 | 39.11±4.81 | 0.187 |
| Total Leukocyte Count | 12580±12544 | 10474±9103.9 | 0.352 |
| ANGPTL-4, ng/ml | 9.42±4.94 | 10.45±4.97 | 0.257 |
| BMI, (kg/m2) | 26.53±4.08 | 27.58±5.17 | 0.259 |
| wc: hc | 0.93±0.03 | 0.91±0.04 | 0.031 |
| LVEF% | 46±7.42 | 57.47±8.56 | 0.0001 |
| Gender, % (Male) | 49 (86) | 42 (66.7) | 0.014 |
| RWMA, (%) | 6 (10.5) | 19 (30.2) | 0.001 |
| Diabetes Mellitus, (%) | 20 (35.1) | 28(44.4) | 0.338 |
| Hypertension, (%) | 15 (26.3) | 32 (50.8) | 0.007 |
| Smoking, (%) | 20 (35.1) | 13 (20.6) | 0.061 |
| Dyslipidemia, (%) | 5 (8.8) | 9 (14.3) | 0.370 |
| Renal disorders, (%) | 0 | 1 (1.6) | 0.345 |
| Family history of CAD, (%) | 9 (15.8) | 16 (25.4) | 0.216 |
| Sedentary lifestyle, (%) | 3 (5.3) | 4 (6.3) | 0.825 |
| Coronary Angiography | | | |
| Normal and minimal coronaries (%) | 2 (3.5) | 21 (33) | 0.0001 |
| SVD (%) | 29 (50.9) | 17 (27) | |
| DVD (%) | 15 (26.3) | 11 (17.5) | |
| TVD (%) | 10 (17.5) | 13 (20.6) | |
ANGPTL-4: Angiopoietin-like-4; BMI: Body mass index; CAD: Coronary artery disease; DVD: Double vessel disease; LVEF: Left ventricular ejection fraction; NSTEMI: Non-ST-elevation myocardial infarction; pcv: packed cell volume; RWMA: Regional wall abnormality motion; SVD: Single vessel disease; STEMI: ST-Elevation Myocardial Infarction; TVD: Triple vessel disease; UA: Unstable Angina; wc: hc: waist to hip circumference
Follow-up: During the median follow up of 24 (22-25.75) months, MACE had occurred among 14 patients. The total number of events occurring among NSTEMI/UA and STEMI patients were 9 (7.5%) and 5 (4.16%) respectively. Among the STEMI patients, five patients died due to cardiovascular causes and among the NSTEMI/UA patients, five died due to cardiovascular causes, three were re-hospitalised and one underwent CABG. Ten patients were lost to follow-up. Moreover, there were no significant differences in the demographic, clinical and laboratory study characteristics among the study patients based on the status of MACE. However, the presence of diabetes (p=0.002) and hypertension (p=0.013) were significantly higher among patients with MACE than among patients without MACE [Table/Fig-3]. ROC was plotted to predict the ability of ANGPTL-4 to predict MACE among ACS patients. However, ANGPTL-4 failed to predict MACE among ACS patients {AUC=0.493, p=0.935; (95% CI 0.321-0.665)}. Kaplan Meier survival curve was plotted for patients with low and high ANGPTL-4 levels and the log-rank test failed to show a significant difference in the survival rate between the two groups (χ2 = 0.100, p=0.75) [Table/Fig-4].
Comparision of patient characteristics based on MACE status.
| Variables | MACE (+) (n=14) | MACE (-) (n=96) | p-value |
|---|
| Age, years | 59.71±9.51 | 54.05±10.82 | 0.06 |
| Blood Glucose, mg/dL | 181.08±53.68 | 164.91±75.40 | 0.48 |
| Blood Urea, mg/dL | 31.62±8.94 | 25.97±11.37 | 0.08 |
| Serum Creatinine, mg/dL | 0.85±0.20 | 0.87±0.28 | 0.76 |
| Haemoglobin, g/L | 13.22±1.66 | 13.55±1.90 | 0.54 |
| pcv | 37.86±4.49 | 39.96±5.22 | 0.15 |
| Total Leukocyte Count | 19200±3519 | 11760±11515 | 0.43 |
| ANGPTL-4, ng/mL | 10.27±6.22 | 9.92±4.81 | 0.80 |
| BMI, (kg/m2) | 29.03±6.08 | 26.84±4.47 | 0.13 |
| wc: hc | 0.92±0.04 | 0.92±0.04 | 0.99 |
| LVEF% | 50±9.12 | 53±9.97 | 0.39 |
| Gender, % (Male) | 9(64.3%) | 82(85.4%) | 0.28 |
| RWMA, (%) | 7(50%) | 62(64.6%) | 0.49 |
| Diabetes Mellitus, (%) | 10(71.4%) | 38(39.5%) | 0.002* |
| Hypertension, (%) | 9(64.3%) | 38(39.5%) | 0.013* |
| Smoking, (%) | 2(14.3%) | 31(32.3%) | 0.312 |
| Dyslipidemia, (%) | 0 | 14(14.6%) | 0.17 |
| Renal disorders, (%) | 0 | 1(1%) | 0.73 |
| Family history of CAD, (%) | 3(21.4%) | 22(23%) | 0.80 |
| Sedentary lifestyle, (%) | 1(7.1%) | 6(6.3%) | 0.75 |
| Coronary Angiography | | | |
| Normal and minimal coronaries (%) | 9(64.3%) | 82(85.4%) | 0.09 |
| SVD (%) | 4(28.6%) | 42(43.8%) | |
| DVD (%) | 1(7.1%) | 25(26%) | |
| TVD (%) | 6(42.9%) | 17(17.7%) | |
ANGPTL-4: Angiopoietin-like-4; BMI: Body mass index; CAD: Coronary artery disease; DVD: Double vessel disease; LVEF: Left ventricular ejection fraction; NSTEMI: Non-ST-elevation myocardial infarction; MACE: Major Adverse Cardiac Events; MACE (+): Presence of major adverse cardiac events; MACE (-): Absence of major adverse cardiac events; pcv: packed cell volume; RWMA: Regional wall abnormality motion; SVD: Single vessel disease; STEMI: ST-Elevation Myocardial Infarction; TVD: Triple vessel disease; wc: hc: waist to hip circumference
Comparision of survival curves between patients with high and low angiopoietin-like 4 (ANGPTL-4).
High ANGPTL-4 was not a significant predictor of major adverse cardiac events in acute coronary syndrome patients (χ2=0.100, p=0.75)
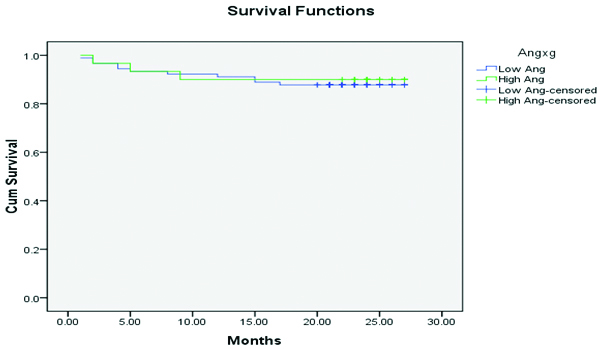
Prediction of MACE in diabetic and hypertensive ACS patients: As the occurrence of MACE was higher among diabetic and hypertensive ACS patients, the Kaplan Meier survival curve was plotted for patients with low and high ANGPTL-4 levels for both the diabetic and hypertensive patients with ACS. On performing the analysis, the log-rank test failed to show any significant difference in the survival rate in both diabetic (χ2=0.002, p=0.97) and hypertensive (χ2=0.002, p=0.96) ACS patients. ROC was plotted to predict the occurrence of MACE among diabetic and hypertensive ACS patients. With regard to the diabetic {AUC=0.466, p=0.741; (95% CI 0.251-0.681)} and hypertensive {AUC=0.386, p=0.292; (95% CI 0.166-0.606)} ACS subjects, ANGPTL-4 failed to predict MACE among the study patients.
Discussion
To the best of our knowledge, this is the first prospective cohort study conducted in the Indian population, where authors have investigated the prognostic ability of ANGPTL-4 for predicting MACE in ACS patients. However, the present work failed to demonstrate the prognostic ability of ANGPTL-4 in predicting MACE among ACS patients. In an earlier study reported by Muendlein A et al., among 490 Caucasian patients, no significant difference was observed in the levels of circulating ANGPTL-4 between patients with and without CAD [15]. In a prospective study, the plasma ANGPTL-4 and ANGPTL-4 variants predicted cardiovascular events independently from conventional cardiovascular risk factors. In another recent study performed among COPD patients, it was reported that ANGPTL-4 was a predictor of atherosclerosis and cardiac dysfunction in COPD patients independent of established risk factors such as high sensitivity C-reactive protein (hsCRP) [16]. The difference in the study population, sample size and follow-up period may have led to the different study findings. The study reported by Muendlein A et al., included a larger group of CAD patients and the follow-up period was much longer compared to the present study [15]. The study reported by Waschki B et al., included COPD patients, which is a population very diverse from present study. ANGPTL-4 encodes a glycosylated; secreted protein containing a C-terminal fibrinogen domain which is highly expressed in the liver, heart, muscle and adipose tissue. This encoded protein is induced by the peroxisome proliferator-activated receptors and acts as a serum hormone that is involved in the regulation of glucose homeostasis, lipid metabolism, and insulin sensitivity [16]. Furthermore, this protein is a strong LPL inhibitor and plays a significant role in modifying LPL activity in conditions of fasting and exercise [17,18].
In present study, the occurrence of MACE events was significantly higher among diabetic and hypertensive ACS patients. Therefore, authors investigated the prognostic ability of serum ANGPTL-4 for predicting the occurrence of MACE among both diabetic and hypertensive ACS patients, but the biomarker did not help in distinguishing patients who were likely to develop events in this subset. Diabetes and hypertension are well-known risk factors for the occurrence of cardiovascular disease [19]. However, not all patients with these risk factors have similar outcomes. Having a circulatory biomarker with prognostic ability will enable us to identify the subset of diabetic and HTN patients; who require more aggressive therapeutic measures. The protein marker ANGPTL-4 is being widely studied among diabetic and hypertensive subjects [20]. Previous genomic studies have reported that ANGPTL-4 variants E40K and T266M were associated with the cardiovascular disease risk among T2DM (type II diabetes mellitus) patients [21,22]. Furthermore, Smart-Halajko C et al., reported that ANGPTL-4 E40K and T266M variant were linked with lower triglyceride levels in T2DM patients and the ANGPTL-4 genotype position did not modify the triglyceride reaction even after the lifestyle alteration [23]. In one of the cross-sectional study, the plasma levels of ANGPTL4 were considerably elevated amongst hypertensive patients than the non-hypertensive. It was also observed that the plasma levels of ANGPTL-4 were elevated among subjects with T2DM and hypertension than in those with T2DM but not hypertension [24].
Limitation
The sample size of present study population was relatively smaller, and hence this precluded us from getting a greater number of major adverse cardiac events. There was heterogeneity in the follow-up periods as they were performed at different intervals of time. It is not known if the patients who were lost to follow-up had any MACE. Moreover, authors could not collect information on the prior use of drugs which might have potentially influenced the level of ANGPTL-4 in the study population.
Conclusion
In conclusion, the present study failed to demonstrate that ANGPTL-4 could be a potential biomarker for the prediction of major adverse cardiac events among acute coronary syndrome patients. Serial measurement of ANGPTL-4 should be performed at different time intervals to understand the pathophysiology of ANGPTL-4 during acute coronary syndrome. However, larger studies are warranted to investigate the prognostic value of ANGPTL-4 among patients with acute coronary syndrome.
ANGPTL-4: Angiopoietin-like-4; BMI: Body mass index; CAD: Coronary artery disease; DVD: Double vessel disease; LVEF: Left ventricular ejection fraction; NSTEMI: Non-ST-elevation myocardial infarction; pcv: packed cell volume; RWMA: Regional wall abnormality motion; SVD: Single vessel disease; STEMI: ST-Elevation Myocardial Infarction; TVD: Triple vessel disease; UA: Unstable Angina; wc: hc: waist to hip circumference
ANGPTL-4: Angiopoietin-like-4; BMI: Body mass index; CAD: Coronary artery disease; DVD: Double vessel disease; LVEF: Left ventricular ejection fraction; NSTEMI: Non-ST-elevation myocardial infarction; MACE: Major Adverse Cardiac Events; MACE (+): Presence of major adverse cardiac events; MACE (-): Absence of major adverse cardiac events; pcv: packed cell volume; RWMA: Regional wall abnormality motion; SVD: Single vessel disease; STEMI: ST-Elevation Myocardial Infarction; TVD: Triple vessel disease; wc: hc: waist to hip circumference
[1]. Prabhakaran D, Jeemon P, Roy A, Cardiovascular Diseases in India: Current Epidemiology and Future DirectionsCirculation 2016 133(16):1605-20.10.1161/CIRCULATIONAHA.114.00872927142605 [Google Scholar] [CrossRef] [PubMed]
[2]. Mohan V, Deepa R, Rani SS, Premalatha G, Chennai Urban Population Study (CUPS No.5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No. 5)J Am Coll Cardiol 2001 38(3):682-87.10.1016/S0735-1097(01)01415-2 [Google Scholar] [CrossRef]
[3]. Grech ED, Ramsdale DR, Acute coronary syndrome: unstable angina and non-ST segment elevation myocardial infarctionBMJ 2003 326(7401):1259-61.10.1136/bmj.326.7401.125912791748 [Google Scholar] [CrossRef] [PubMed]
[4]. Crea F, Libby P, Acute coronary syndromes: the way forward from mechanisms to precision treatmentCirculation 2017 136(12):1155-66.10.1161/CIRCULATIONAHA.117.02987028923905 [Google Scholar] [CrossRef] [PubMed]
[5]. Kumar A, Cannon CP, Acute coronary syndromes: diagnosis and management, part IMayo Clin Proc 2009 84(10):917-38.10.4065/84.10.91719797781 [Google Scholar] [CrossRef] [PubMed]
[6]. Littnerova S, Kala P, Jarkovsky J, Kubkova L, Prymusova K, Kubena P, GRACE Score among Six Risk Scoring Systems (CADILLAC, PAMI, TIMI, Dynamic TIMI, Zwolle) demonstrated the best predictive value for prediction of long-term mortality in patients with ST-Elevation Myocardial InfarctionPLoS One 2015 10(4):e012321510.1371/journal.pone.012321525893501 [Google Scholar] [CrossRef] [PubMed]
[7]. Grootaert C, Van de Wiele T, Verstraete W, Bracke M, Vanhoecke B, Angiopoietin-like protein 4: health effects, modulating agents and structure-function relationshipsExpert Rev Proteomics 2012 9(2):181-99.10.1586/epr.12.1222462789 [Google Scholar] [CrossRef] [PubMed]
[8]. Dijk W, Beigneux AP, Larsson M, Bensadoun A, Young SG, Kersten S, Angiopoietin-like 4 promotes intracellular degradation of lipoprotein lipase in adipocytesJ Lipid Res 2016 57(9):1670-83.10.1194/jlr.M06736327034464 [Google Scholar] [CrossRef] [PubMed]
[9]. Myocardial Infarction Genetics and CARDIoGRAM Exome Consortia InvestigatorsStitziel NO, Stirrups KE, Masca NG, Erdmann J, Ferrario PG, Coding Variation in ANGPTL4, LPL, and SVEP1 and the Risk of Coronary DiseaseN Engl J Med 2016 374(12):1134-44.10.1056/NEJMoa150765226934567 [Google Scholar] [CrossRef] [PubMed]
[10]. Mandard S, Zandbergen F, van Straten E, Wahli W, Kuipers F, Müller M, The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposityJ Biol Chem 2006 281(2):93-44.10.1074/jbc.M50651920016272564 [Google Scholar] [CrossRef] [PubMed]
[11]. Yoshida K, Shimizugawa T, Ono M, Furukawa H, Angiopoietin-like protein 4 is a potent hyperlipidemia-inducing factor in mice and inhibitor of lipoprotein lipaseJ Lipid Res 2002 43(11):1770-72.10.1194/jlr.C200010-JLR20012401877 [Google Scholar] [CrossRef] [PubMed]
[12]. O’Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the American College of Emergency Physicians and Society for Cardiovascular Angiography and InterventionsCatheter Cardiovasc Interv Off J Soc Card AngiogrInterv 2013 82(1):E1-27.10.1002/ccd.24776 [Google Scholar] [CrossRef]
[13]. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice GuidelinesJ Am Coll Cardiol 2014 64(24):e139-228.10.1161/CIR.0000000000000134 [Google Scholar] [CrossRef]
[14]. Hicks KA, Mahaffey KW, Mehran R, Nissen SE, Wiviott SD, Dunn B, 2017 Cardiovascular and stroke endpoint definitions for clinical trialsCirculation 2018 137(9):961-72.10.1161/CIRCULATIONAHA.117.03350229483172 [Google Scholar] [CrossRef] [PubMed]
[15]. Muendlein A, Saely CH, Leiherer A, Fraunberger P, Kinz E, Rein P, Angiopoietin-like protein 4 significantly predicts future cardiovascular events in coronary patientsAtherosclerosis 2014 237(2):632-38.10.1016/j.atherosclerosis.2014.10.02825463098 [Google Scholar] [CrossRef] [PubMed]
[16]. Waschki B, Kirsten AM, Holz O, Meyer T, Lichtinghagen R, Rabe KF, Angiopoietin-like protein 4 and cardiovascular function in COPDBMJ Open Respir Res 2016 3(1):e00016110.1136/bmjresp-2016-00016127933182 [Google Scholar] [CrossRef] [PubMed]
[17]. La Paglia L, Listì A, Caruso S, Amodeo V, Passiglia F, Bazan V, Potential role of ANGPTL4 in the cross talk between metabolism and cancer through PPAR Signaling PathwayPPAR Res 2017 2017:818723510.1155/2017/818723528182091 [Google Scholar] [CrossRef] [PubMed]
[18]. Olshan DS, Rader DJ, Angiopoietin-like protein 4: A therapeutic target for triglycerides and coronary disease?J Clin Lipidol 2018 12(3):583-87.10.1016/j.jacl.2018.01.01229548670 [Google Scholar] [CrossRef] [PubMed]
[19]. Hajar R, Framingham contribution to cardiovascular diseaseHeart Views Off J Gulf Heart Assoc 2016 17(2):78-81.10.4103/1995-705X.18513027512540 [Google Scholar] [CrossRef] [PubMed]
[20]. Tjeerdema N, Georgiadi A, Jonker JT, van Glabbeek M, Dehnavi RA, Tamsma JT, Inflammation increases plasma angiopoietin-like protein 4 in patients with the metabolic syndrome and type 2 diabetesBMJ Open Diabetes Res Care 2014 2(1):e00003410.1136/bmjdrc-2014-00003425512873 [Google Scholar] [CrossRef] [PubMed]
[21]. Abid K, Trimeche T, Mili D, Msolli MA, Trabelsi I, Nouira S, ANGPTL4 variants E40K and T266M are associated with lower fasting triglyceride levels and predicts cardiovascular disease risk in Type 2 diabetic Tunisian populationLipids in Health and Disease 2016 15:6310.1186/s12944-016-0231-627004807 [Google Scholar] [CrossRef] [PubMed]
[22]. Talmud PJ, Smart M, Presswood E, Cooper JA, Nicaud V, Drenos F, ANGPTL4 E40K and T266M: effects on plasma triglyceride and HDL levels, postprandial responses, and CHD riskArteriosclerThrombVasc Biol 2008 28(12):2319-25.10.1161/ATVBAHA.108.17691718974381 [Google Scholar] [CrossRef] [PubMed]
[23]. Smart-Halajko MC, Kelley-Hedgepeth A, Montefusco MC, Cooper JA, Kopin A, McCaffrey JM, ANGPTL4 variants E40K and T266M are associated with lower fasting triglyceride levels in Non-Hispanic White Americans from the Look AHEAD Clinical TrialBMC Med Genet 2011 12:8910.1186/1471-2350-12-8921714923 [Google Scholar] [CrossRef] [PubMed]
[24]. Abu-Farha M, Cherian P, Qaddoumi MG, AlKhairi I, Sriraman D, Alanbaei M, Increased plasma and adipose tissue levels of ANGPTL8/Betatrophin and ANGPTL4 in people with hypertensionLipids Health Dis 2018 17(1):3510.1186/s12944-018-0681-029490644 [Google Scholar] [CrossRef] [PubMed]