Surgical correction of post-operative aphakia with insufficient capsular support can be performed using one of several methods of secondary IOL implantation. These methods include implantation of Angle-Supported Anterior Chamber lOLs (ACIOLs), Iris-Claw IOLs (IC-IOLs) into either the anterior or posterior chamber, or Scleral-Fixated Posterior Chamber Intraocular Lenses (SF-PCIOLs). ACIOLs are currently rarely used, as they have numerous post-operative complications [1,2]. Therefore, IC-IOLs and SF-PCIOLs are the mainstay for correction of aphakic eyes lacking adequate capsular support, and are used according to pre-operative ocular conditions and the surgeons’ experience.
The IC- or lobster-claw-IOL (a biconvex PMMA IOL) was developed by Worst JG et al., for treating myopia [3]. They subsequently developed anterior chamber IC-IOL implantation to correct refraction of aphakic eyes [4]. To decrease the risk of corneal endothelial cell loss, Amar L et al., modified this technique, by fixing IC-IOLs into the posterior chamber [5]. The Artisan Aphakia Model 205 (convex/concave) (Ophtec BV, Groningen, the Netherlands) is a recent version of such lenses. IC-IOLs are fixated to the midperipheral iris, where the iris is less vascularised and less reactive, by using claw-shaped haptics, facilitating surgical procedures. Fixation of the IC-IOL into the posterior rather than the anterior chamber, ensures a more physiological placement of the IOL away from the corneal endothelium, avoiding progressive endothelial cell loss [6,7]. However, even when an IC-IOL is fixated in the posterior chamber, the direct contact between the iris tissue and the IOL haptics may lead to iris pigment dispersion. Furthermore, the sutured wound induces astigmatism. Additionally, late dislocation of these IOLs has been reported [8].
Given the more physiological position, some surgeons prefer Transscleral (TS)-sutured PCIOL implantation for correction of aphakia with insufficient capsular support, particularly when there are co-existing abnormalities of the anterior segment of the eye or poorly controlled glaucoma. However, this method is technically more difficult and takes longer. Furthermore, suture degradation can lead to dislocation of the TS-sutured IOL [9].
Therefore, the present study compared the results of implantation of retropupillary IC-IOLs with those of TS-sutured PCIOLs, in the early post-operative period, in aphakic eyes with insufficient capsular support.
Materials and Methods
This observational prospective study was conducted at the Department of Ophthalmology, Military Institute of Aviation Medicine, Warsaw, Poland, from February 2017 to December 2017. All patients provided informed consent for participation in the study. The study protocol, which complies with the provisions of the Declaration of Helsinki, was approved by the Ethical Commission of the Military Institute of Aviation Medicine (No. 4/2017) before the start of this study.
The inclusion criterion was post-operative aphakia with insufficient capsular support. The etiology of aphakia was identified in each case. The exclusion criteria were corneal endothelial cell count less than 800, peripheral anterior synechiae, rubeosis iridis, chronic uveitis, macular oedema, proliferative diabetic retinopathy, retinal detachment and monocularity.
The following data were collected: gender, age, axial length of the eye, pre-existent ocular co-morbidity, previous ocular surgery, and date of cataract surgery. IOL calculations were performed pre-operatively with the use of the IOL Master 500 optical biometer (Carl Zeiss Meditec AG, Jena, Germany). Pre-operative data were collected by the resident physician.
Forty one eyes of 41 patients with post-operative aphakia with insufficient capsular support were identified during study period. Of these 41 patients, 3 patients had proliferative diabetic retinopathy and 2 patients had macular oedema and they were not included in the study. Ultimately 36 eyes of 36 Caucasian patients (aged 31-89 years old) were enrolled in the study.
Topical antibiotics and oral acetazolamide were administered to all patients pre-operatively. The choice of the surgical method of aphakia correction (retropupillary IC-IOL or TS-sutured PCIOL) was made by a surgeon, based on the residual capsule condition and iris status. TS-sutured PCIOL was implanted in the eyes with residual capsule less than 180° or if the iris was damaged. Retropupillary IC-IOL implantation was performed in the eyes with residual capsule more than 180° and if the iris was unhurt.
All procedures were performed by one of the three experienced surgeons using the same techniques, under local anesthesia (peribulbar injection of lignocaine).
The iris-claw group included 19 eyes of 19 patients (mean age 71.74±9.06, range 52-89 years). All patients underwent posterior chamber implantation of Artisan Aphakia IOL model 205 (Ophtec BV), which is a rigid, concave-convex, polymethylmethacrylate iris-claw lens with an overall length of 8.5 mm and optical zone of 5.4 mm.
The transscleral fixation group included 17 eyes of 17 patients (mean age: 65.29±16.58, range 31-84 years) who underwent TS-fixation of a foldable hydrophilic acrylic PCIOL SuperFlex 620H (Rayner Intraocular Lenses Ltd., Worthing, UK), with an optic diameter of 6.25 mm and an overall length of 12.5 mm.
BCVA measurements (expressed in Snellen decimal letters) and Goldmann applanation tonometry were performed preoperatively and at one day, one week, one month, and three months post-operatively. The operating time and complications were reported and compared between the two groups. Post-operatively, a patient in both groups received antibiotic drops four times daily for one week and steroid drops five times a day in doses that were gradually reduced over a six-week period.
Surgical Techniques
Posterior Chamber Implantation of the IC-IOL: All surgeons used a standardised technique for IC-IOL implantation, which included creation of two vertical paracentral paracenteses at the 2 o’clock and 10 o’clock positions, preparation of a 5.5-mm wide limbal incision at the 12 o’clock position, pupil constriction by intracameral injection of a carbachol solution (0.10 mg/mL), and injection of a viscoelastic material (1% sodium hyaluronate) into the anterior chamber and behind the iris. Bimanual anterior vitrectomy was performed if vitreous prolapse occurred in the anterior chamber. Then, the iris-claw IOL was inserted through the corneal wound into the anterior chamber in a reversed position (with angulation directed backwards). The IOL was rotated such that the haptics were positioned at 3 o’clock and 9 o’clock, and the lens was slipped through the pupil into the posterior chamber. This was followed by centering the IC-IOL on the pupil, and enclavation of the midperipheral iris between the claw haptics by applying gentle pressure over the slotted centre of the lens haptic by means of a small spatula. Next, a prophylactic peripheral superior iridectomy was performed to avoid post-operative pupillary block. Finally, the viscoelastic device was completely removed and 10-0 nylon sutures were placed close to the limbal incision. Injections of intracameral cefuroxime (1 mg) and subconjunctival dexamethasone (2 mg) were administered after surgery.
Transscleral, posterior chamber suturing fixation of the Super-flex 620H IOL: A 3.0-4.0-mm incision, at 50% depth, was made 1.0-mm posterior to the surgical limbus at the 3:30 o’clock and 9:30 o’clock meridians, avoiding the long posterior ciliary arteries. Two scleral tunnels (width: 3.0-4.0 mm) were subsequently dissected backwards, 180 degrees from each other. Next, a 3.5-mm clear corneal incision was made at the 12 o’clock position. Bimanual anterior vitrectomy was performed if vitreous was observed in the anterior chamber. One needle of a double-armed 9-0 polypropylene suture was introduced into the anterior chamber, passed to the ciliary sulcus and sclera, and externalised on the surface of the conjunctiva in the vicinity of the prepared scleral tunnel. The second needle of the 9-0 suture was passed through the slit in the IOL haptic and subsequently externalised 2.0-3.0 mm away from the location of the first suture on the surface of the conjunctiva in the same manner as the first needle (modified Hoffman technique). The same procedure was performed with the second double-armed 9-0 suture for the second haptic.
The IOL was folded and introduced into the posterior chamber with haptics placed in the ciliary sulcus by pulling on the two sutures. The needles of the 9-0 sutures were then cut, and the sutures were retrieved from both scleral pockets on the corneal surface. The suture ends were tied, and the knots were buried in the scleral tunnels. The main corneal wound was closed by stromal hydration. Intracameral cefuroxime (1 mg) and subconjunctival dexamethasone (2 mg) injections were administered at the end of the surgery.
The operating time was recorded for all procedures.
Statistical Analysis
All statistical analyses were performed using Statistica Version 12.5 PL (StatSoft Inc., Tulsa, OK, USA). Descriptive statistics were used to report demographic and ocular characteristics for both patient groups. Single-factor repeated-measures analysis of variance was performed to determine the statistical significance of differences in the mean BCVA pre-operatively and at each post-operative follow-up. Unpaired t-tests and the Mann-Whitney U test were used to compare patients’ BCVA and IOP as well as the operating time between the two groups. The values are expressed as the mean±Standard Deviation (SD). p<0.05 was considered statistically significant.
Results
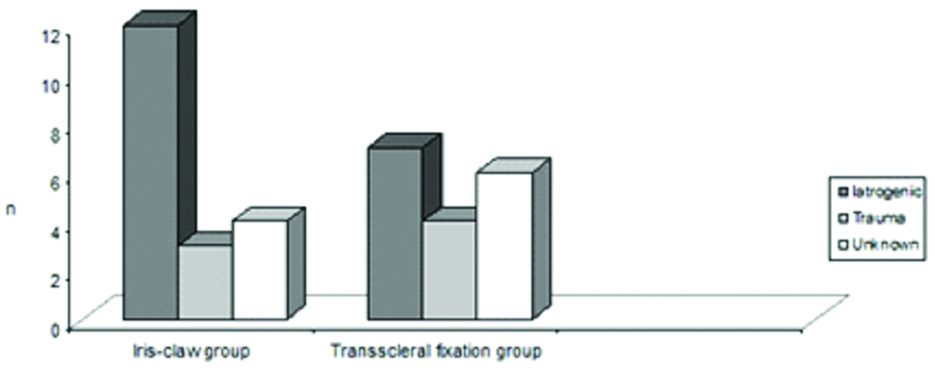
There were no significant differences in age, sex, laterality, and axial length of the eyeball between the two groups (all p>0.05, [Table/Fig-1]). Complications during cataract surgery were the main cause of insufficient capsular support in both groups (iatrogenic cause, [Table/Fig-2]). One eye in the iris-claw group and two eyes in the transscleral fixation group had previously undergone vitrectomy because of complicated cataract surgery.
Patients’ demographic and ocular characteristic of two groups.
| Iris-claw group | Transscleral fixation group | p-value |
|---|
| Eyes/patients | 19/19 | 17/17 | - |
| Age at operation (mean±SD, years) | 71.74±9.06 | 65.29±16.58 | 0.66a |
| Sex (M/F) | 6/13 | 10/7 | 0.18b |
| Glaucoma | 9/19 | 6/17 | 0.52b |
| Pseudoexfoliation syndrome | 3/19 | 2/17 | 1.00b |
| Axial length of eyeball | 23.46±2.19 | 22.85±1.09 | 0.22a |
| Interval between previous cataract surgery and secondary IOL implantation (mean±SD, months) | 3.64±3.84 | 3.72±2.37 | 0.38a |
aMann-Whitney U test; bFisher’s exact test
SD: Standard deviation; M: Male; F: Female; IOL: Intraocular lens
Causes of insufficient capsular support in the iris-claw and transscleral fixation groups.
Visual Recovery
No statistically significant differences were observed in mean pre-surgical BCVA between the two groups (p>0.05, [Table/Fig-3]). Mean BCVA at one day post-operatively was significantly better in the iris-claw group (0.32±0.12) than in the transscleral fixation group (0.21±0.13, p=0.01). No statistically significant changes in mean BCVA were noted between the two groups at one week, one month, and three months post-operatively.
Comparison of mean BCVA of the two groups over time.
| Iris-claw group | Transscleral fixation group | p-value |
|---|
| Preoperative | 0.53±0.28 | 0.50±0.29 | 0.76a |
| 1 day | 0.32±0.12 | 0.21±0.13 | 0.01a |
| 1 week | 0.44±0.17 | 0.40±0.21 | 0.45a |
| 1 month | 0.50±0.23 | 0.43±0.22 | 0.37a |
| 3 months | 0.57±0.24 | 0.49±0.26 | 0.36a |
aTwo-sample independent t test
In both groups, the mean BCVA at one day post-operatively was significantly worse than the pre-operative value (iris-claw group: p=0.002; transscleral fixation group: p=0.0001), but it recovered gradually over the three months’ follow-up. No statistically significant changes in mean BCVA were observed in either group at one week, one month, and three months post-operatively as compared to pre-operatively (p>0.05).
Intraocular Pressure
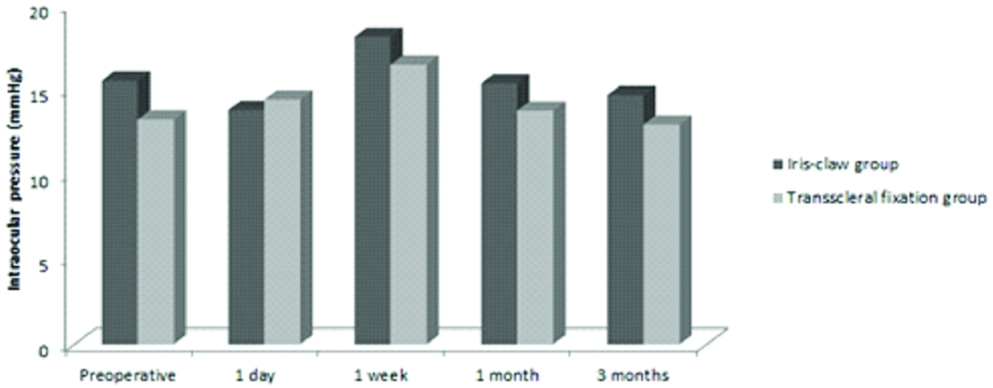
The mean IOP did not differ significantly between the iris-claw and transscleral fixation groups pre-operatively (15.53±5.30 and 13.24±3.87, respectively), at one day (13.79±4.71 and 14.41±4.43, respectively), one week (18.11±7.37 and 16.47±6.91, respectively), one month (15.37±5.21 and 13.76±3.44, respectively) and three months (14.68±3.54 and 12.94±3.09, respectively) after surgery [Table/Fig-4].
Comparison of mean IOP of the two groups over time.
Operating Time
The mean operating time in the iris-claw group was significantly shorter than that in the transscleral fixation group (25.53±9.98 min, 49.76±16.48 min, respectively; p=0.000003).
Complications
No intra-operative complications were noted in any cases in both group and a central or nearly central position of the IOL was achieved in all eyes. In the transscleral fixation group, the IOP increased to more than 25 mmHg post-operatively in three eyes (17.65%). Hyphema and retinal detachment developed in one eye each (5.88%) during follow-up after PCIOL suture fixation. In the iris-claw group, the main post-operative complication was pupil distortion (21.05%). IOP was elevated in one eye (5.26%), which decreased after the application of topical therapy. One case (5.26%) of spontaneous dislocation of one haptic of the IC-IOL occurred at 78 days post-operatively. Cystoid macular oedema occurred in one eye (5.26%) at two months post-operatively in the iris-claw group.
Discussion
Although the surgical techniques for secondary IOL implantation continue to improve, correction of aphakia without a stable lens bag remains challenging. Several studies have compared iris-claw lens with TS implantation of PCIOL for the treatment of aphakia with insufficient capsular support [12,13,15-18]. Previous studies have compared mostly anterior chamber, but not posterior chamber IC-IOLs, with TS-sutured PCIOL fixation [12,13,15-17]. Both IC-IOLs and TS-sutured PCIOLs have advantages and unique complications, and thus, it is unclear which is most appropriate for the management of aphakic eyes without sufficient capsular support. Jing W et al., described no significant difference in safety between these two operations [14], but their meta-analysis included studies of anterior as well as posterior chamber IC-IOLs implantations. The current literature reports no statistically significant difference in post-operative corneal endothelial cell loss between iris-claw implantation and posterior chamber IOL ciliary sulcus suture fixation over an approximately one-year follow-up [12,16,17]. However, given that endothelial cell loss changes occur slowly, further studies with a longer follow-up time are needed to verify the results.
The implantation of a retropupillary IC-IOL combines the advantages of a PCIOL and a time-efficient operation technique; however, various complications may occur intra- and post-operatively [7,8,11,19-23]. In the current study, in the iris-claw group, the post-operative IOP exceeded 25 mmHg in one eye, which was managed medically with topical anti-glaucoma drugs. This eye had pre-existing glaucoma secondary to past endophthalmitis that occurred as a complication of phacoemulsification surgery. The frequency of increased IOP after iris-claw lens implantation in this study is comparable with that in some previous reports [20,21].
The convex/concave IC-IOLs implanted in all patients in this study are one of the latest types designed for aphakia. The convexity of the optical surface of an IC-IOL reduces the contact between the iris and lens, thereby reducing pigment release from the iris. However, we observed gentle accumulation of pigmented precipitates on the IOL surface in one eye in the iris-claw group, probably due to an inflammatory reaction associated with the operation. The pigment dispersion did not lead to BCVA deterioration, and no additional surgery was needed. Moreover, we observed pupil ovalisation in four cases (21,05%), similar to the report by Gonnermann J et al., [21]. This may be caused by asymmetric enclavation or differences in the volume of the clamped iris tissue, and should be considered during enclavation.
One case (5%) in our study had spontaneous dislocation of the haptic of the iris-claw lens, which occurred 78 days post-operatively. The IOL was successfully refixed with enclavation. No total luxation of an IC-IOL was observed.
Cystoid macular oedema occurred in one eye at two months after implantation of an IC-IOL. The patient was effectively treated with oral acetazolamide, and the patient’s BCVA was 0.9 at the end of follow-up. The ocular history of this patient included glaucoma, epiretinal membrane, and non-proliferative diabetic retinopathy in the operated eye.
Sutured SFIOL surgery is not without complications [9,24-28], which may vary based on the surgeon’s experience and the technique used to anchor the IOL to the sclera. The incidence of post-operative elevated IOP after TS fixation of a PCIOL reportedly ranges from 2.2% to 44% [9,24-27] and increases when pars plana vitrectomy precedes the surgery [15,29,30]. In this study, two of three patients with post-operative ocular hypertension had pre-existing glaucoma (one case each of post-traumatic glaucoma and primary open-angle glaucoma), and the third patient had previously undergone pars plana vitrectomy. Thus, the IOP elevation in present study can be partly explained by the pre-existing risk factors for glaucoma, such as prior trauma, rather than the surgery itself. In all cases, the post-operative increase in IOP was transient and responded to topical treatment.
In some series of TS-fixation of PCIOLs without pars plana vitrectomy, the retinal detachment rates were found to be 1.4-5.0% [12,24,26,28]. However, in aphakic eyes after combined pars plana vitrectomy and lensectomy, the incidence of retinal detachment after secondary scleral fixation of PCIOL implantation with sutures was 15.63% [9]. In our cohort, we found one case (5.88%) of retinal detachment at three months after TS-suture fixation of a PCIOL. This patient had undergone pars plana vitrectomy with removal of intravitreal lens fragment three months before secondary implantation of the IOL. Teng H et al., also observed retinal detachment at three months after TS-sutured PCIOL implantation [12]. These observations suggest that the risk of retinal detachment should be discussed with patients before undertaking this surgical procedure, especially if previous vitrectomy has been performed.
In the present study, only one eye (5.88%) in the transscleral fixation group developed hyphema. Kjeka O et al., retrospectively analysed 91 eyes after TS-suture fixation of a PCIOL and reported a 3.3% incidence rate of anterior chamber haemorrhage [24]. Similar findings were described in other studies [9,12,27]; however, some studies reported a higher incidence of hyphema, of up to 13.3% [31]. We encountered no cases of post-operative suture breakage, lens tilting, IOL dislocation, uveitis, choroidal or vitreous haemorrhage, or Cystoid Macular Edema (CME) in the transscleral fixation group; however, our follow-up period was short. A long-term retrospective study with a mean follow-up of 23 months reported dislocation of the implanted lens in three cases (2%), post-operative CME in five cases (4%) and vitreous haemorrhage in 23 cases (19%) [25].
In our study, post-operative BCVA at one day post-operatively was significantly better in the iris-claw group than in the transscleral fixation group (0.32 vs. 0.21, p=0.01). Hara S et al., also reported earlier visual recovery after posterior chamber IC-IOL implantation in aphakic eyes without capsular support than after TS-suture fixation of a PCIOL [13]. Our visual acuity results are comparable with those of Teng H et al., who also observed patients for three months, but their study included patients who underwent anterior chamber IC-IOLs [12].
The surgical technique for fixation of an iris-claw IOL is much easier than that involved in implantation of a TS-sutured PCIOL, which accounts for the statistically significantly shorter mean operating time required for insertion of the IC-IOL than for TS-suture fixation of the PCIOL in our study (p=0.000003). Hara S et al., [13] reported similar findings. Although Jing W et al., did not confirm a direct relationship between complications and operation time in their meta-analysis [14], it is likely that shorter operating time would result in less trauma to the ocular tissues and would thereby, facilitate faster visual recovery.
Limitation
The main limitations of this study are its non-randomised design and short follow-up duration of three months. Further studies with longer follow-up and more patients are warranted to compare these two surgical methods.
Conclusion
The present findings suggested that secondary retropupillary implantation of an iris-claw IOL in aphakic eyes without capsular support is an efficient surgical procedure, with a low incidence of post-operative complications. Compared with TS-suture fixation of a PCIOL, the IC-IOL method takes less time to perform and patients achieve earlier post-operative visual improvement.
aMann-Whitney U test; bFisher’s exact test
SD: Standard deviation; M: Male; F: Female; IOL: Intraocular lens