GERD is a public health problem having significant impact on society because it leads to huge economic burden and decreased quality of life. The various agents currently used for treatment of GERD include PPIs, prokinetic agents, mucoprotective substances, antacids and H2-blockers [1]. Of these, PPIs and combination of PPI and prokinetics provide the most effective control of gastric acidity and related symptoms like epigastric pain, heartburn, reflux and are treatment of choice. Combination of PPIs and prokinetic agents is increasingly used by medical practitioners for severe and resistant GERD [2].
India drug market is oversupplied with many drug formulations of Domperidone and pantoprazole, where many of them are available in combination. The efficacy and safety of combined prokinetic and PPI therapy for GERD remain controversial [3-6]. While a few studies have shown the clinical efficacy of adding prokinetics to PPI therapy in GERD, others have shown no therapeutic benefit. The question still remains whether there is sufficient evidence of efficacy and cost effectiveness of PPI and prokinetic combination.
It has been difficult until now, to identify GERD patients who will benefit from the addition of a prokinetic to PPI therapy prior to treatment. The introduction of Frequency Scale for the Symptoms of GERD (FSSG) [7,8] provides useful assistance for making the initial diagnosis of GERD, and also allows quantitative assessment of the effects of treatment and changes in symptoms over time from the addition of a prokinetic to PPI therapy.
When it comes to price, there is a big difference between various classes of drugs used for GERD. PPIs are one of the most frequently dispensed therapeutic classes. However, PPIs cost more than other acid inhibiting agents and the volume of prescribing has had a substantial impact on prescribing budgets. In India, there is a big difference in the prices of generic medicines vis-a-vis the prices of the branded medicines.
There is a general misconception that pharmacoeconomic evaluation is merely a means to find the least expensive alternative or getting the most bangs for a buck but in actual reality, it is a comparison tool [9]. It will not always indicate a clear choice, but will evaluate options quantitatively and objectively based on a defined model which has, not yet been established for GERD treatment.
Hence, we conducted this study with the aim to perform pharmacoeconomic evaluation of Pantoprazole and Pantoprazole plus Domperidone used in the management of GERD.
Materials and Methods
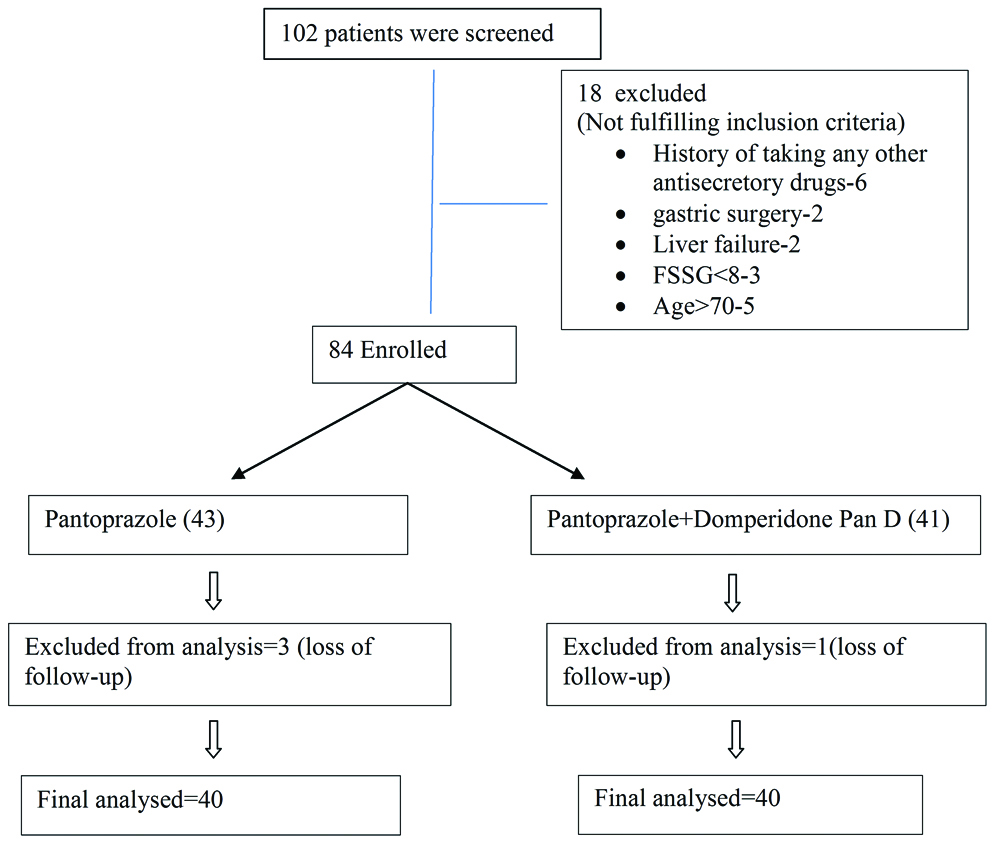
This was randomised control open label study on 80 patients at Medicine OPD/IPD of tertiary care hospital. Sample size was based on prevalence rate of GERD in India (7.6%) [10]. It was calculated based on the following formula 4 pq/n2
(p=prevalence of GERD in India=7.6%, q=100-p, n=error (6% in our study)
Sample Size=4×7.6×(100-7.6)/62
=78.2
The study was started after getting approval from institutional Ethics committee (Ref SKNMC/Ethics/App/2016/142). Patients were screened by convenient sampling method. Drug allotment was done by simple randomisation method.
Inclusion criteria were: age ≥18 years and <70 years, the presence of any gastrointestinal symptoms like heartburn (burning sensation in the chest accompanied by pain) and/or regurgitation (acid taste and bitter to the tongue), diagnosis of initial clinical or previous symptomatic GERD with FSSG Symptom score ≥8 and no history of taking any antisecretory drugs, antacids and prokinetics for at least 14 days.
Exclusion criteria were: presence of oesophagitis requiring intervention, oesophageal varices, Barrett’s oesophagus, scleroderma, ulcers (gastric or duodenal), atrophic gastritis, eradication treatment of H. pylori completed less than 15 days of starting treatment, Gastric or oesophageal surgery, gastric surgery, or upper gastrointestinal diseases such as gastric cancer or peptic ulcer; females in pregnancy, lactation, or who wish to become pregnant if they refuse to use adequate contraception during the study period and concomitant serious diseases such as kidney failure, heart and liver failure; use of other scheduled medications metabolised by cytochrome CYP3A4 during the study like benzodiazepines, warfarin and phenytoin.
After taking a written informed consent, patients were allotted randomly into following two groups: One group was given Tab. PanD that is Pantoprazole (40 mg)+Domperidone (30 mg) once daily for two weeks, while another group was only given Tab Pan 40 that is Pantoprazole (40 mg) once daily for two weeks. Both the drugs are from Alkem Company, procured and supplied by researcher to patients [Table/Fig-1].
The FSSG questionnaire [7,8] was administered pre-treatment and after treatment at two weeks. FSSG results were considered in terms of total score, reflux score, and dyspeptic score (maximum; TS 48, RS 28, DS 20 points, respectively). Total score was considered to carry out the pharmacoeconomic analysis.
Following parameters were used to evaluate cost effectiveness [11]:
a) Cost effectiveness ratio: Cost effectiveness ratio for two groups was calculated by dividing the cost of treatment by its clinical outcome (FSSG score) to yield the ratio in terms of rupees.
b) Cost minimization analysis: Cost minimization analysis was carried out assuming that health benefits obtained from two alternative therapies are identical. Market price (maximum retail price) of both drugs was obtained from the hospital pharmacy and retailer’s shop. The percentage of price difference between each of the prescribed drug groups and its generic version was calculated.
Statistical Analysis
The characteristics of all treatment groups were compared for both demographic and efficacy variables (FSSG score). All the data was recorded in the entry form and presented as mean±SEM/SD for numerical data, and proportion (%) for the categorical data. In all tests mean values of pre and post score compared with Student’s paired t-test. Difference between improvement of FSSG score of Pan and PanD group compared with unpaired t-test significance. Data was analysed using graph pad prism software version 6. The p<0.05 was considered as significant.
Results
Out of 80 patients enrolled in this study, most patients were in age group 19-38 with male predominance. Symptoms are more common in patients with mix diet. Average FSSG total prescore is 15.23 with Pan and 18.45 with PanD [Table/Fig-2].
Baseline characteristics of the study population (N=80).
| | Total No of patients | Pantoprazole (N=40) | PAND (N=40) |
|---|
| Gender | Male | 55 | 27 | 28 |
| Female | 25 | 13 | 12 |
| Age Group (years) | 19-38 | 36 | 17 | 19 |
| 39-58 | 25 | 15 | 10 |
| 59-78 | 19 | 8 | 11 |
| Diet | Vegetarian | 29 | 14 | 15 |
| Mix Diet | 51 | 26 | 25 |
| Addiction | Addicted to alcohol/smoking | 49 | 19 | 30 |
| Non Addicted | 31 | 21 | 10 |
| FSSG prescore | RS | 80 | 7.75 | 9.95* |
| DS | 80 | 7.45 | 8.50 |
| TS | 80 | 15.23 | 18.45* |
RS: Reflux score; DS: Dysmotility score; TS: Total score
FSSG prescore of Pan and PanD group compared with paired t-test significance *-p<0.05, p-0.04 for TS, P-0.32 for DS, p-0.03 for RS
After treatment for a period of two weeks there is statistically highly significant change observed in all types of FSSG score in both groups [Table/Fig-3].
Results of the mean improvement of FSSG score in both groups after two week treatment.
| FSSG scores | Prescore | Postscore | Mean of Difference | 95% Confidence Interval | T value | p-value |
|---|
| Pan (N=40) | Rs | 7.75 | 1.92 | 5.850 | 4.511-7.189 | 8.84 | <0.001 |
| Ds | 7.45 | 2.10 | 5.350 | 4.282-6.418 | 10.13 | <0.001 |
| Ts | 15.23 | 3.90 | 11.33 | 9.713-12.940 | 14.21 | <0.001 |
| PanD (N=40) | Rs | 9.95 | 3.18 | 6.775 | 5.468-8.082 | 10.49 | <0.001 |
| Ds | 8.50 | 3.35 | 6.150 | 4.952-7.348 | 10.39 | <0.001 |
| Ts | 18.45 | 5.52 | 12.93 | 10.971-14.880 | 13.34 | <0.001 |
Pan: Pantoprazole; PanD: Pantoprazole+Domperidone; RS: Reflux score; DS: Dysmotility score, TS: Total score
Difference between pre and postscore of each group compared with Students paired t-test. Significance at p<0.05
Comparison of individual improvement scores (difference in pre and post score) between Pan and PanD groups showed no statistically significant difference although PanD group has higher improvement score compared to Pan group [Table/Fig-4].
Comparison between improvement of FSSG score of Pan and PanD group (N=40/group).
| Pan (Mean±SEM) | PanD (Mean±SEM) | 95% confidence interval | T value | p-value |
|---|
| Rs | 5.850±0.6617 | 6.775±0.064 | -0.9190-2.769 | 1 | 0.32 |
| Ds | 5.350±0.5281 | 6.150±0.592 | -0.7822-2.382 | 1.008 | 0.31 |
| Ts | 11.321±0.7969 | 12.930±0.9683 | -0.9007-4.101 | 1.276 | 0.21 |
Pan: Pantoprazole; PanD: Pantoprazole+Domperidone; RS: Reflux score; DS: Dysmotility score; TS: Total score
Difference between improvement of FSSG score of Pan and PanD group compared with unpaired t-test significance p<0.05
It was found out that for having the same unit improvement 9.7 Rs are required for Pan and 11.2 Rs required for PanD. Thus Pan is more cost effective than PanD [Table/Fig-5].
Comparison of average cost effective ratio (cost/outcome) between Pan and PanD.
| Pan (n=40) | PanD (n=40) |
|---|
| a) Cost in rupees/2 wk | 110.6 | 145.6 |
| FSSG (pre) | 15.23 | 18.45 |
| FSSG (post) | 3.9 | 5.525 |
| b) Difference in scores | 11.32 | 12.92 |
| a/b | 9.76 | 11.27 |
There is difference between prices of Pan and PanD. Moreover, for each of these drugs, there is also a vast difference in prices at hospital pharmacy (Generic by Archies life sciences) and at retailer (MRP of same drug, branded by the same company). Price of Branded drugs is four to five times more than their generic counterpart [Table/Fig-6]. Few adverse effects were observed with both the drugs during study period [Table/Fig-7].
Cost minimisation analysis of Pan and PanD.
| Drug | Branded (Cost in rupees/10 tab) | Generic (Cost in rupees/10 tab) |
|---|
| Pan | 79 | 15.4 |
| PanD | 104.5 | 21 |
List of adverse effect in Pan and PanD group.
| Symptoms | Pan | PanD |
|---|
| Dizziness | | |
| Headache | 2 | |
| Abdominal pain | | |
| Nausea | 1 | |
| Diarrhoea | 1 | 1 |
| Arthralgia | | |
| Other | | |
Discussion
In this prospective study a total of 80 patients were included. Most patients studied in this study were in age group 19-38 with male predominance as seen in [Table/Fig-2]. The FSSG score analysis was done where in the reflux, dysmotility and total scores for Pan and PanD before and after treatment were compared. As expected, total scores for both Pan and PanD decreased significantly. Total score of Pan decreased from 15.23 to 3.91 and for PanD decreased from 18.45 to 5.52 and the values are statistically significant as seen in [Table/Fig-3].
Few studies are available with combination of pantoprazole plus mosapride, omeprazole plus cisapride, omeprazole plus domperidone as seen in [Table/Fig-8] [2,4,12-19]. In these studies additional benefit of prokinetics to a standard dose of PPI in patients with GERD, was seen mostly in the subgroup of severely symptomatic patients [3,4,13,15,20]. Probable reason for this beneficial action is the combination of PPI and prokinetics acting synergistically by decreasing acid production as well as improvement of lower oesophageal sphincter function, improvement of oesophageal motility, and acceleration of gastric emptying, thus producing a better therapeutic response [21].
Compilation of studies comparing PPI Vs PPI+Prokinetics [2,4,12-19].
| Author | Drug and Dosage | Parameter | Duration | Sample size | Outcome |
|---|
| Ndraha S [2] | Omeprazole 40 mg+domperidone 30 mg, Vs omeprazole 40 mg. | FSSG | 2 wks | 60 | Combination is more superior compared to monotherapy in GERD patients with high FSSG score. |
| Madan K et al., [4] | Pantoprazole 40 mg BD+mosapride 5 mg TDS Vs Pantoprazole 40 mg BD | oesophageal pH-metry endoscopy | 8 wks | 61 | Combination is more effective than pantoprazole alone in providing symptomatic relief to patients with erosive GERD but with non-erosive GERD there was no significant difference. |
| Hsu YC et al., [12] | Lansoprazole (30 mg once daily)+Placebo Vs lansoprazole 30 mg OD+Mosapride 5 mg TDS | FSSG | 4 wks | 96 | Mosapride generally does not provide additional benefit to a standard dose of lansoprazole in patients with reflux oesophagitis, except possibly in the subgroup of severely symptomatic patients. |
| Cho YK et al., [13] | Esomeprazole 40 mg/day+mosapride 30 mg TDS | high resolution manometry | 4 wks | 50 | Combined therapy in GERD may reduce the number of reflux episodes but not the duration of acid exposure time |
| Miwa H et al., [14] | Omeprazole 10 mg OD+mosapride 5 mg TDS Vs Omeprazole 10 mg OD+Placebo | Visual analogue scale | 4 wks | 200 | The addition of mosapride to omeprazole was not effective than omeprazole alone |
| Van Rensburg CJ et al., [15] | Pantoprazole 40 mg/d+cisapride 20 mg bid | Endoscopy | 8 wks | 350 | Combination provides no further benefit in the treatment of GERD. |
| Hunchaisri N et al., [16] | Domperidone 10 mg TDS+omeprazole 20 mg BD VS omeprazole BD | Reflux Symptom Index (RSI) | 3 months | 65 | Combination is not superior to omeprazole alone in the treatment of LPR. |
| Yamaji Y et al., [17] | Mosapride 5 mg TDS+Omeprazole 10 mg OD Vs Omeprazole 10 mg OD | FSSG | 4 wks | 60 | Combining provided no additional amelioration of reflux symptoms compared to PPI alone. |
| Lim HC et al., [18] | Pantoprazole 40 mg OD Vs pantoprazole 40 mg OD+mosapride citrate 5 mg TID | gastric emptying scan Questionnaire for symptoms plasma gastrin and plasma CCK | 8 wks | 38 | Mosapride showed to be effective in preventing delayed gastric emptying and the increase in plasma gastrin level induced by PPI treatment, but did not show prominent clinical symptom improvements. |
| Pradeep Kumar BT [19] | Pantoprazole 40 mg BD alone Vs Pantoprazole 40 mg BD+Tab. Itopride 50 mg TDS | Endoscopy FSSG scores | 4 wks | 100 | Combination is more effective in endoscopic healing of oesophagitis and in ameliorating the symptoms of GERD than Pantoprazole alone. |
PPIs with prokinetics combination also improve the effect of PPIs. PPIs are unstable at a low pH, further dysmotility will slow down gastric emptying, resulting in retention of PPIs. Retention of PPIs inside the stomach for a long time may result in an impaired acid suppressive effect, so rapid transit of the PPIs to the upper intestine may be of benefit [8]. So, even this combination can be used in patients with GERD even without symptoms of dysmotility.
But in current study when we compared the individual improvement scores between Pan and PanD the results were not statistically significant as seen in [Table/Fig-4]. Pantoprazole is the more acid stable PPI [22]. Add on action of Domperidone that is increased gastric emptying and rapid transit of PPI to the upper intestine might not have helped with Pantoprazole. Thus, instead of Pantoprazole combination of other acid unstable PPI like omeprazole and prokinetc agents may have better efficacy than PPI alone as seen in some previous studies [2]. Current findings were in accordance with meta-analysis conducted by Ren L-H et al., where he concluded that there is no advantage for the addition of prokinetics to a PPI therapeutic regimen, relative to PPI alone [6]. However, combined therapy of PPI plus prokinetic may partially improve patient’s quality of life, but has no significant effect on symptom or endoscopic response of GERD.
There are many preparations in the market of about 120 for Pantoprazole in price range of 18-80 rupees and for 131 for PanD in range of 55 to 117 rupees [23,24]. Thus, due to wide price ranges, cost effective ratio is very important having impact on budget.
The ACER (Average Cost Effectiveness Ratio) was calculated by dividing the cost of treatment by its clinical outcome (FSSG score). Thus Pan is more cost effective than PanD.
On doing the cost minimisation analysis where only cost and not the efficacy were considered, the costs included in our study were Rs 79 for 10 tablets of Pan and 105 Rs for PanD. Thus Pan is cheaper than PanD. Other notable observation was that generic brands of both drugs (procured from Hospital pharmacy that is non Branded Generic) are cheaper than branded drugs (available at medical store and sell at MRP). Therapeutic switching to an equivalent cheaper or generic PPI would reduce financial burden on the patients without affecting the quality of patient care. Other studies in India have shown a very significant difference of prices between branded and generic drugs. The cost of branded drugs prescribed was 20% to 21.8% more than the generic versions [25,26]. There is need to start more no of generic stores or Janaushadhi stores programme initiated by Government of India.
We observed few adverse drug reactions in present study where two patients had headache, one had nausea in Pan group and one each had diarrhoea for Pan and PanD as seen in [Table/Fig-6]. Other studies also reported few adverse effects with PPI and Prokinetics [6,27]. This may be the reason for giving these drugs for long time and with good patient compliance.
Limitation
Limitation of our study was that follow-up was not done and recurrence was not seen which commonly occurs in patients with acid peptic disease after stopping treatment. It was not feasible to co-relate FSSG score with Endoscopic finding as endoscopy was not advised to these patients. Pharmmacoeconomic analysis should be done with using different brands.
Conclusion
Pantoprazole is most commonly available PPI with 120 brands with price range Rs18-80 cheaper than PanD. There is vast difference between Branded and Generic drugs. Both drugs provide the most effective control of gastric acidity and related symptoms. PAN is more cost effective than PanD. PanD should be preferred only for PPI resistant GERD, patients with nausea and vomiting, in the subgroup of severely symptomatic patients.
RS: Reflux score; DS: Dysmotility score; TS: Total score
FSSG prescore of Pan and PanD group compared with paired t-test significance *-p<0.05, p-0.04 for TS, P-0.32 for DS, p-0.03 for RS
Pan: Pantoprazole; PanD: Pantoprazole+Domperidone; RS: Reflux score; DS: Dysmotility score, TS: Total score
Difference between pre and postscore of each group compared with Students paired t-test. Significance at p<0.05
Pan: Pantoprazole; PanD: Pantoprazole+Domperidone; RS: Reflux score; DS: Dysmotility score; TS: Total score
Difference between improvement of FSSG score of Pan and PanD group compared with unpaired t-test significance p<0.05