PONV is an unpleasant feeling of nausea, retching, or vomiting that occurs within the first 48 hours following surgery [1]. It is considered as a distressing event, resulting in patient discomfort and dissatisfaction following anaesthesia [2].
Patients following surgery, experience fear for PONV more than that of the post operative pain, besides making patients suffer and feel uncomfortable, it can also delay patient discharge from the post anaesthesia care unit causing an increased morbidity and unanticipated prolonged hospital admissions due to poor wound healing, hypoglycaemia, increased postoperative pain and wound infection as a consequence of nausea and vomiting [1]. Despite the various improvements made in anaesthetic techniques, anaesthetic agents and identification of various risk factors like age, female predominance, smoking, obesity, type and duration of surgery, incidences of PONV is estimated to be 25-30% in all post-surgical patients and up to 80% in patients with multiple high-risk factors [1,3]. The incidence of PONV with middle ear surgeries is estimated to be between 50-80% [4]. It has been observed that the highest emetic sequalae was seen in patients receiving general anaesthesia compared to the other modalities of anaesthesia [5]. Various pharmacological techniques were employed earlier in preventing PONV like corticosteroids (dexamethasone), gastrointestinal prokinetics (metoclopramide), neuroleptic butyrophenones (droperidol) phenothiazines (promethazine /prochlorperazine) and serotonin antagonists (ondansetron), of which the first generation serotonin 5-HT3 receptor antagonists like ondansetron are the most commonly used prophylactic agents in the management of PONV [6].
Palonosetron, a second generation 5HT3 receptor antagonists, with its distinct pharmacological features of greater binding affinity, longer half life and eliciting 5HT3 receptor internalization results in extended inhibition of receptor thereby preventing PONV for a extended period [3]. Dexamethasone a synthetic steroid is now being used widely as an antiemetic in patients following chemotherapy and surgery. Though the mechanism of action is not fully understood, it is said to exert its action by inhibition of prostaglandin synthesis and prevention of release of serotonins [7]. Because of its low cost and safety in use, dexamethasone is considered as a drug of choice in preventing PONV. Metoclopramide, a gastrointestinal prokinetic acts by centrally anatgonizing the Chemoreceptor Trigger Zone (CTZ) and thereby is been effectively used as an antiemetic agent over 40 years. The efficacy of the drug is increased when used along with combination therapies of 5HT3 receptor anatagonists and corticosteroids owing to complete responses by 80-90% with minimal side effects.
Our study has aimed to compare the efficacy of Palonosetron and dexamethasone in preventing PONV.
Materials and Methods
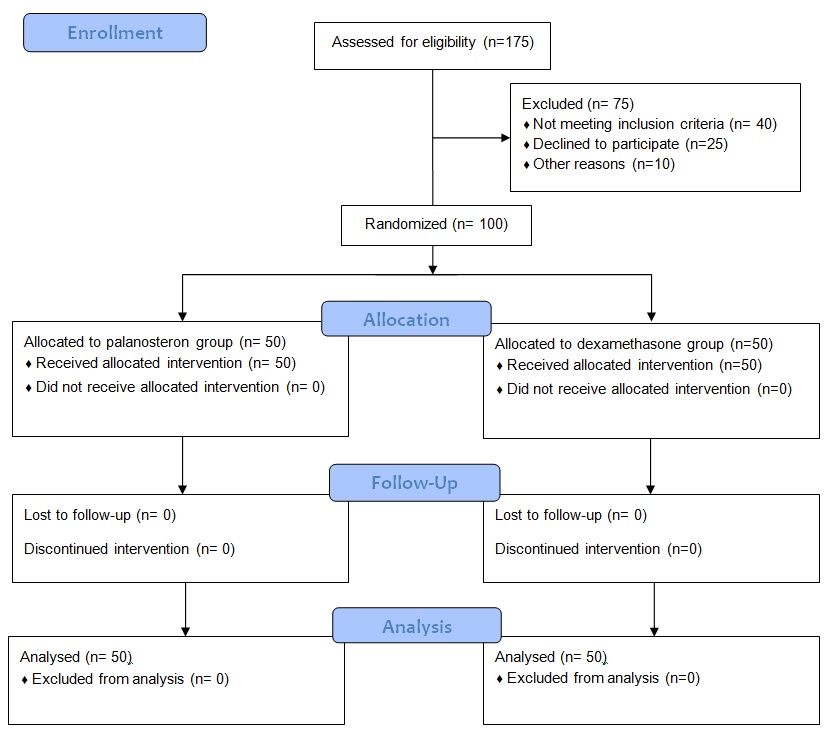
This prospective randomised double blinded study was conducted after obtaining the institutional ethical committee approval (REF NO: IEC: RC/15/22). This study was conducted in the Department of Anaesthesiology and critical care at Pondicherry Institute of Medical Sciences between October 2015 to April 2017. After explaining the procedure an informed and written consent was obtained from all patients a day before the surgery. A total of 100 adult patients aged 18-60 years, of American Society of Anaesthesiologists (ASA) physical status I & II of both genders were scheduled for ear and nose surgeries requiring endotracheal intubation for more than one hour were enrolled. Sample size was calculated based on a previously published clinical trial comparing the efficacy of palanosteron and dexamethasone showing complete response of 90.2% in palaonosteron group and 85% in dexamethasone group [8]. The calculated sample size was 100 with 50 in each group and having 80% power, at 0.05 level of significance.
Patients who have undergone chemotherapy within four weeks or emetogenic radiotherapy within eight weeks of study entry, body mass index of > 30kg/m2, pregnant patients, use of investigational study drugs within 30 days of study entry, use of drugs with potential anti emetic efficacy, any episode of nausea, vomiting, or retching within 24 hours prior to anaesthesia, ASA physical status ≥ III and also patients with known allergy to any of the study drugs were excluded from the study.
Those patients willing to participate in the study were divided into two groups using computer generated block randomization. Group P patients received 75mcg of Palonosetron IV diluted to 5 ml with saline and Group D patients received 8mg of Dexamethasone IV diluted to 5 ml with saline [Table/Fig-1]. All patients were premedicated with Tab.lorazepam 1mg and Tab.Rantidine 150 mg, given per orally night before surgery and also in the morning two hours prior to surgery. Preoperative routine investigations like Haemoglobin, total count, differential count, urine routine were asked for and results were reviewed. On the day of surgery after shifting to operation theatre, non invasive monitors like electrocardiogram, noninvasive BP, and pulse oximeter were connected and baseline blood pressure, heart rate and saturation were recorded. Intra venous access was established with 18 gauge cannula and a slow infusion of Ringer lactate was started.
On table, patients were pre medicated with Inj.Glycopyrolate 10mcg/kg iv, Inj.Fentanyl 2mcg/kg iv, Inj.Midazolam 0.03mg/kg iv. The study drug was prepared by the anaesthesiologists (operator), the observer and the patient were blinded to the drug and the operator administered the study drug to the patients over five minutes, three minutes prior to induction. Anaesthesia was induced with Inj. Thiopental 3-5mg/kg iv and muscle relaxant Inj.Vecuronium 0.1mg/kg iv. Patients were then intubated with an appropriate size endotracheal tube and were maintained with O2: Air (50:50), Isoflurane (MAC 1) and inj.Vecuronium 0.03mg/kg. Intraoperatively BP and HR were noted every 15 minutes for one hour after administration of study drug. Intraopeartive analgesia was supplemented by administering Inj.Paracetamol 1g iv for all patients half an hour prior to extubation. At the end of the surgery patients were reversed from neuromuscular blockade with Inj. Neostigmine 60mcg/kg along with Inj.Glycopyrolate 10mcg/kg iv. Patients were then shifted to recovery room and postoperatively for the first 24 hours patients were reviewed every 4 hourly for the presence of retching, nausea, vomiting and was scored using four point scale [9]. 0=no nausea/vomiting, 1= nausea alone, 2= vomiting once, 3= vomiting twice or more times in 30 minutes interval. If patient experiences nausea and vomiting with score >2, Inj metoclopramide 10 mg iv was given as a rescue antiemetic medication. Incidence of side effects like headache, dizziness and drowsiness if any were noted in the next 24 hours and postoperative analgesia was supplemented by administering NSAIDS, Diclofenac 75mg IM, eight hourly.
Parameters Studied:
• Intraoperative hemodynamic changes from the baseline BP, HR were noted every 15 minutes for one hour after administration of study drug.
• Postoperatively, the presence of retching, nausea, vomiting and was scored using four point scale were noted by reviewing patients every four hourly.
• Incidence of side effects like headache, dizziness and drowsiness if any were noted in the next 24 hours.
Statistical Analysis
The data were presented as descriptive statistics for continuous variables and percentages for categorical variables and was subjected to Z-test/Chi-square test/ Fisher-exact test. All the data was analysed using SPSS package (version 21.0 SPSS INC, Chicago, IL, USA) software for windows. In all parameters, the value of p<0.05 was considered as significant.
Results
The study was assessed in terms of incidence of PONV, number of patients requiring rescue antiemetics and the episodes of side effects if any. The demographic profile was comparable between the groups and was not statistically significant [Table/Fig-2]. Intraoperative haemodynamic parameters like mean systolic blood pressure and diastolic blood pressure [Table/Fig-3,4] were comparable among two groups, while significant differences were noted in mean heart rate [Table/Fig-5] among the two groups at baseline and 30 minutes. The incidence of nausea and vomiting were observed at 0-4 hours, 4-8 hours, 8-16 hours and 16-24 hours [Table/Fig-6]. The requirement of rescue antiemetic was observed in both groups [Table/Fig-7] and also the four point scale was noted to be higher in the dexamethasone group [Table/Fig-8]. The side effect profile of both the drugs was also comparable and commonly seen were headache, dizziness and drowsiness.
| Palonosetron (P) | Dexamethasone (D) | p-value |
|---|
| Mean Age (yr) | 30.26 (18-55) | 32.28 (18-57) | 0.283 (NS) |
| Gender (M:F) | 37:13 | 24:26 | 0.008 (NS) |
| Mean Weight (kg) | 61.74 (42-84) | 62.26 (40-86) | 0.800 (NS) |
| Mean Height (cm) | 164.20 (150-178) | 164.10 (155-186) | 0.950 (NS) |
| Mean BMI (kg/m2) | 22.83(18.66-26.51) | 23.14 (16.64-24.64) | 0.655 (NS) |
| Smoker: non smoker | 6:44 | 8:42 | 0.564 (NS) |
| ASA grade I:II | 47:3 | 44:6 | 0.487 (NS) |
| Duration of anaesthesia (hours) | 3.430 | 3.000 | 0.119 (NS) |
p<0.05 is significant; NS: Non Significant
Mean systolic blood pressure of study participants among 2 groups.
| Study drug | N | Mean | Std. Deviation | p-value* |
|---|
| SBP Preop BP | Dexamethasone | 50 | 126.30 | 11.626 | 0.109 (NS) |
| Palonosetron | 50 | 122.74 | 10.358 |
| SBP 15 min | Dexamethasone | 50 | 114.74 | 14.199 | 0.718 (NS) |
| Palonosetron | 50 | 115.76 | 13.988 |
| SBP 30 min | Dexamethasone | 50 | 109.28 | 10.371 | 0.224 (NS) |
| Palonosetron | 50 | 112.12 | 12.694 |
| SBP 45 min | Dexamethasone | 50 | 105.46 | 9.355 | 0.499 (NS) |
| Palonosetron | 50 | 106.94 | 12.260 |
| SBP 60 min | Dexamethasone | 50 | 104.46 | 9.414 | 0.262 (NS) |
| Palonosetron | 50 | 106.82 | 11.416 |
Z Test for difference between 2 means; p-value < 0.05 is significant
NS – Non Significant, N-No of patients
Mean diastolic blood pressure of study participants among 2 groups.
| Study drug | N | Mean | Std. Deviation | p-value* |
|---|
| DBP PreopBP | Dexamethasone | 50 | 78.12 | 8.863 | 0.693 (NS) |
| Palonosetron | 50 | 78.76 | 7.224 |
| DBP 15 min | Dexamethasone | 50 | 73.60 | 9.626 | 0.946 (NS) |
| Palonosetron | 50 | 73.46 | 10.990 |
| DBP 30 min | Dexamethasone | 50 | 70.32 | 8.532 | 0.478 (NS) |
| Palonosetron | 50 | 71.70 | 10.727 |
| DBP 45 min | Dexamethasone | 50 | 67.22 | 7.859 | 0.612 (NS) |
| Palonosetron | 50 | 68.08 | 9.003 |
| DBP 60 min | Dexamethasone | 50 | 66.74 | 7.450 | 0.548 (NS) |
| Palonosetron | 50 | 67.76 | 9.367 |
Z Test for difference between 2 means; p-value <0.05 is significant
NS: Non Significant; N:No of patients
Mean Heart Rate (HR) of study participants during baseline and intraoperatively.
| Study drug | N | Mean | Std. Deviation | p-value* |
|---|
| Preop HR (beats/min) | Dexamethasone | 50 | 92.98 | 12.296 | 0.001# |
| Palonosetron | 50 | 84.48 | 13.089 |
| HR 15 min | Dexamethasone | 50 | 98.04 | 14.479 | 0.055 |
| Palonosetron | 50 | 92.46 | 14.312 |
| HR 30 min | Dexamethasone | 50 | 89.78 | 10.424 | 0.034# |
| Palonosetron | 50 | 84.68 | 13.147 |
| HR 45 min | Dexamethasone | 50 | 83.60 | 8.843 | 0.133 |
| Palonosetron | 50 | 80.48 | 11.536 |
| HR 60 min | Dexamethasone | 50 | 79.28 | 9.664 | 0.385 |
| Palonosetron | 50 | 77.34 | 12.407 |
*Z-test for difference between 2 means; # p-value (<0.05) is significant
| DexamethasoneN (%) | PalonosetronN (%) |
|---|
| 0-4 hours | 21 (42.0%) | 9(18.0%) |
| 4-8 hours | 4 (8.0%) | 0 (0.0%) |
| 8-16 hours | 0 (0.0%) | 0 (0.0%) |
| 16-24 hours | 0 (0.0%) | 1 (2.0%) |
| 0-24 hours | 25 (50.0%) | 10 (20%) |
Chi-square test; p-value=0.006; there is statistically significant differences in PONV episodes between two groups; N: no of patients
Requirement of rescue medication.
| Study drug | Total |
|---|
| Dexamethasone | Palonosetron |
|---|
| Rescue antiemetic, inj. perinorm 10 mg iv | Yes | 15 | 5 | 20 |
| No | 35 | 45 | 80 |
| Total | 50 | 50 | 100 |
Chi-square test; p-value=0.012 there is statistically significant differences
Comparison of the mean four point scale among the 2 groups.
| Study drug | Total |
|---|
| Dexamethasone | Palonosetron |
|---|
| Four point scale | 0 | 28 | 40 | 68 |
| 1 | 6 | 5 | 11 |
| 2 | 11 | 4 | 15 |
| 3 | 5 | 1 | 6 |
| Total | 50 | 50 | 100 |
Chi-square test; p-value=0.0185; there is statistically significant differences
Discussion
PONV is a distressing event. The aetiopathogenesis of PONV is very complex and is triggered by various inputs that arrive from multiple areas [10]. There are certain risk factors that have been identified for the development of PONV and are classified into preoperative-patient-related, intraoperative–surgery and anaesthesia-related and also postoperative factors like pain, dehydration etc., [6]. Anaesthetic agents initiate vomiting reflexes by stimulating the 5HT3 receptors on the chemoreceptor trigger zone CTZ, thereby releasing serotonin from the enterochromaffin cells [6]. With various pharmacological agents being employed prophylactically in the prevention of PONV, 5HT3 receptor antagonists are commonly used. Palonosetron, the second generation serotonin 5HT3 receptor antagonists has unique structural, pharmacological features unlike the other antagonists thereby making it an efficacious antiemetic agent with less side effects like headache, dizziness and constipation [11]. In recent times, dexamethasone the synthetic steroid although used earlier for preventing nausea and vomiting following chemotherapy, has also shown to be effective in preventing PONV though the exact mechanism is not clear [12,13]. The SAMBA society has recommended various PONV prophylaxsis guidelines among which dexamethasone and Palonosetron play an important role [14].
Candiotti KA et al., observed that palonosetron of 75 mcg is an effective dose in preventing PONV following major gynaecological and laparoscopic surgery than 25 mcg and 50 mcg in the 0-48 hour period [3]. In our study we compared the efficacy and safety of intravenous Palonosetron 75 mcg 5HT3 antagonists and intravenous dexamethasone 8 mg in preventing PONV for patients undergoing ear and nose surgeries following general anaesthesia.
The overall incidence of PONV in 0-24 hours were maximum with dexamethasone group with 50% (n=25) and 20% (n=10) in Palonosetron group which was comparable to the study conducted by Tahir S et al., which showed the PONV incidence in group D at 6-24 hours was 40% (n=16) and group P was 20% (n=8) [15]. In the study conducted by Candiotti KA et al., the incidence of PONV was 26% between 0 – 24 hours in patients who received 75 mcg Palonosetron as compared to 57% in patients who received placebo [3]. Kovac AL et al., observed a PONV incidence of 44% in patients receiving Palonosetron 75mcg in 0-24 hours [16]. This value is higher than the value observed in our study 20% in Palonosetron group in 0-24 hours and may be due to difference in the surgical technique, residual pneumoperitoneum and use of different anaesthetics.
The four point scale was observed to be higher in dexamethasone group compared to Palonosetron group and was statistically significant with p<0.05, therefore the requirement of rescue antiemetic medication was 30% (n =15) in dexamethasone group and 10% (n=5) in Palonosetron group. This was similar to the study conducted by Tahir S et al., where the overall use of rescue medication was 15% (n=6) in group P (palonosetron) and 42.5% (n=17) in group D (dexamethasone) [15]. Kovac AL et al., showed that the requirement of rescue antiemetic was 46% in placebo group and 27% in palonosetron group [16].
The adverse effects with a single therapeutic dose of study drugs were not statistically significant and this was similar to the incidence found in study of Gugale AA et al., [17]. These side effects may be the effects of surgical procedure itself or due to the post anaesthetic sequelae and not directly linked to the study drugs.
Limitation
The baseline incidence of PONV was not evaluated by the inclusion of a placebo group because it would be unethical to withhold prophylactic antiemetic drugs in patients at high risk for PONV. Patients were followed up for only 24 hours postoperatively. Ideally, follow-up upto 48 hours could have been done.
Conclusion
Our study has shown that Palonosetron is more effective in the prevention of PONV with superior antiemetic efficacy in first 24 hours compared to dexamethasone with decreased incidence of PONV, decreased requirement of rescue medication with minimal side effects as compared to dexamethasone.
p<0.05 is significant; NS: Non Significant
Z Test for difference between 2 means; p-value < 0.05 is significant
NS – Non Significant, N-No of patients
Z Test for difference between 2 means; p-value <0.05 is significant
NS: Non Significant; N:No of patients
*Z-test for difference between 2 means; # p-value (<0.05) is significant
Chi-square test; p-value=0.006; there is statistically significant differences in PONV episodes between two groups; N: no of patients
Chi-square test; p-value=0.012 there is statistically significant differences
Chi-square test; p-value=0.0185; there is statistically significant differences