Pseudomyxoma Peritonei Secondary to Rupture of Intraductal Papillary Neoplasm of Pancreas (IPMN)
Saurabh Kumar1, Alok Kumar Mittal2
1 Consultant Radiologist, Department of Radiology, Star Imaging, New Delhi, India.
2 Consultant Radiologist, Department of Radiology, Star Imaging, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Saurabh Kumar, F-7 Bali Nagar New Delhi-110015, India.
E-mail: sunny_mamcd911@yahoo.com
Pseudomyxoma peritonei is the intraperitoneal accumulation of a gelatinous ascites secondary to mucinous tumour rupture, more commonly associated with ovarian and appendiceal mucinous tumour. However, pancreatic mucinous tumour, rarely Intraductal Papillary Mucinous Neoplasm (IPMN) is sometimes the aetiological factor. IPMN is either main pancreatic duct, branch duct or mixed duct type and is characterised by abundant extracellular mucin production and mucin retention in the pancreatic duct. This case report highlights the rare occurrence of Pseudomyxoma peritonei secondary to IPMN rupture.
Adenocarcinoma, Cytoreduction, Mucinous, Pancreatic fistula
Case Report
A 55-year-old female presented with increased abdominal girth, diffuse abdominal pain and generalised weakness for last three months. Physical examination revealed distended abdomen with mild epigastric area tenderness, rest of systemic examination was unremarkable. Patient was anicteric with normal peripheral counts.
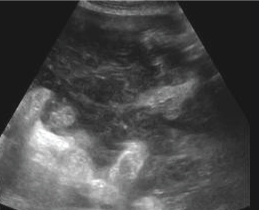
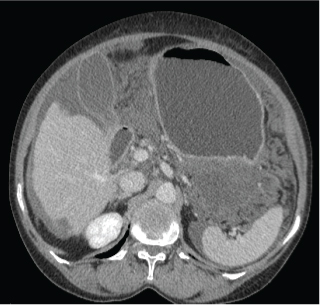
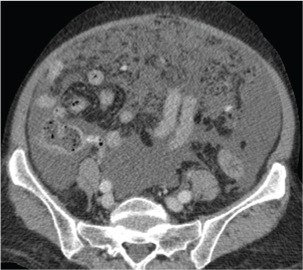
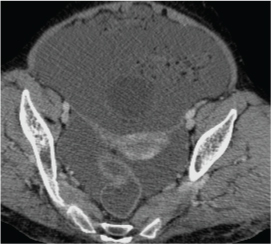
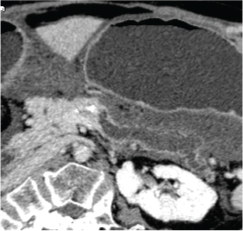
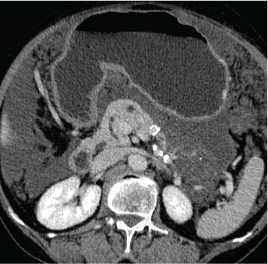
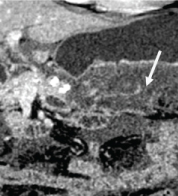
Routine ultrasound showed moderate ascites with non movable echoes within [Table/Fig-1]. CECT abdomen was advised which revealed features of Pseudomyxoma peritonei as low density fluid with loculations causing liver scalloping [Table/Fig-2], extending to pelvis and associated omental thickening/caking [Table/Fig-3,4]. Pancreas revealed normal parenchymal enhancement and bulk with moderate dilatation (11mm) of main pancreatic duct in body and tail without side branch dilatation [Table/Fig-5,6]. Ill-defined hypodense multiloculated lesion seen abutting to pancreatic tail extending to lesser sac with focal discontinuity of pancreatic tail parenchyma and direct communication between the lesion and dilated main pancreatic duct [Table/Fig-7,8]. Few foci of calcification were seen within the lesion. Appendix and bilateral adnexa showed no abnormality.
Transverse ultrasound image of abdomen showing ascites with non movable echoes within.
Axial CECT abdomen showing right lobe liver scalloping (arrow).
Pseudomyxoma peritonei with omental thickening (arrow), pelvic ascites with normal appendix (small arrow).
Normal bilateral adnexa (arrows).
Axial CECT abdomen image.

Curved MPR image - showing main pancreatic duct dilatation in body and tail (arrows) without parenchymal atrophy or side branch dilatation.
Axial image showing hypodense lesion adjacent to pancreatic tail with internal fine septa and soft calcification.
Curved coronal MPR image showing focal discontinuity of pancreatic parenchyma in tail.
Based on imaging findings of pancreatic duct dilatation with multiloculated lesion abutting pancreatic tail and features of Pseudomyxoma peritonei the final diagnosis of Mucinous Neoplasm of Pancreas (IPMN) with rupture causing Pseudomyxoma peritonei was made.
Preoperatively, similar findings were observed as were described on CT with mucinous implants accumulating in the pelvis and subphrenic regions. Histopathological analysis of lesion abutting pancreatic tail revealed mucin pools with low cellularity bland cytology Peritoneal lesions contain histologically benign mucinous epithelium within abundant extracellular mucin with hyalinising fibrotic reaction separating pools of mucin. Pancreatectomy specimens reveal dilated main duct filled with mucin with low grade dyplasia with focal parenchymal breach in pancreatic tail region.
Discussion
Pseudomyxoma peritonei is a rare condition and is characterised by slow accumulation of large volumes of mucinous ascites with mucin implantation on the omentum and peritoneal surface [1]. More frequently it originates from a ruptured adenoma or a well-differentiated mucinous adenocarcinoma of the appendix or ovary and is rarely associated with mucinous carcinomas of the pancreas, such as mucinous cystic neoplasms and IPMNs [2]. The pathogenesis of Pseudomyxoma peritonei is divided into two types [3]. When it occurs secondary to benign/borderline or from well-differentiated (low-grade) mucinous carcinomas it is referred as disseminated peritoneal adenomucinosis which is amenable to surgical debulking. And when it occurs secondary to a mucinous carcinoma of the gastrointestinal tract, pancreas, or ovary it is termed as peritoneal mucinous carcinomatosis which has a fatal course. IPMN of the pancreas is a distinct mucinous tumour of pancreas which arises either in the main pancreatic duct or one of its branches and is characterised by extracellular mucin production and mucin retention in the pancreatic duct [4]. They generally tend to have a good prognosis and surgically resectable. However when they are associated with invasive carcinoma, the prognosis is worse [4].
In our case, CT images showed findings of diffuse main pancreatic ductal dilatation without side branch dilatation or parenchymal calcification, which are consistent with diagnosis of main pancreatic duct IPMN. In addition, there was multiloculated lesion adjacent to pancreatic tail with focal discontinuity of pancreatic parenchyma and communication between the dilated pancreatic duct and the lesion which further suggested possibility of focal rupture of IPMN. The collaborative findings of Pseudomyxoma peritonei with normal appendix and bilateral adnexa further strengthened our diagnosis. Few isolated cases of Pancreatic IPMN rupture associated with Pseudomyxoma peritonei have been reported in literature [5,6].
The cause of IPMN rupture is exactly not known but proposed theory of gradual increase in intraductal pressure by mucin plugging/duct stenosis with subsequent rupture and extrapancreatic mucin spillage in few earlier described cases of pancreatic fistula secondary to IPMN rupture looks appropriate [6]. Other possible explanation in absence of duct blockage stressing upon pancreatic parenchymal consistency of either hard or soft pancreas which determines the risk of pancreatic fistula after pancreaticoduodenectomy, needs further consideration [7].
Treatment of IPMN is well established and main duct, combined or symptomatic branch duct types are to be resected [8]. While treatment of Pseudomyxoma peritonei depending upon aetiology; includes debulking and cytoreductive surgery, with intraperitoneal chemotherapy and radiotherapy reserved for peritoneal carcinomatosis cases [9]. Our patient was taken up for pancreatectomy with debulking for Pseudomyxoma peritonei.
Conclusion
This case highlights towards the fact that Pseudomyxoma peritonei can be the first presentation of pancreatic mucinous tumour like IPMN and radiologist must be aware of this rare possibility.
[1]. Brent Mayes G, Chuang VP, Fisher RG, CT of Pseudomyxoma PeritoneiAJR 1981 136:807-08.10.2214/ajr.136.4.8076261564 [Google Scholar] [CrossRef] [PubMed]
[2]. Takeuchi M, Matsuzaki K, Yoshida S, Nishitani H, Uchara H, Imaging findings of urachal mucinous cystadenocarcinoma associated with pseudomyxoma peritoneiActa Radiol 2004 45(3):348-50.10.1080/0284185041000495915239434 [Google Scholar] [CrossRef] [PubMed]
[3]. Ronnett BM, Yan H, Kurman RJ, Shmookler BM, Wu L, Sugarbaker PH, Patients with pseudomyxoma peritonei associated with disseminated peritoneal adenomucinosis have a significantly more favorable prognosis than patients with peritoneal mucinous carcinomatosisCancer 2001 92(1):85-91.10.1002/1097-0142(20010701)92:1<85::AID-CNCR1295>3.0.CO;2-R [Google Scholar] [CrossRef]
[4]. Sohn TA, Yeo CJ, Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Lillemoe KD, Intraductal papillary mucinous neoplasms of the pancreas: an increasingly recognized clinicopathologic entityAnn Surg 2001 234:313-21.10.1097/00000658-200109000-0000511524584 [Google Scholar] [CrossRef] [PubMed]
[5]. Huh S, Lee HK, Lee MH, Yi BH, Kim HK, Jung JC, Pseudomyxoma peritonei caused by ruptured intraductal papillary mucinous neoplasm of the pancreas: a case reportJ Korean Soc Radiol 2014 70(5):359-62.10.3348/jksr.2014.70.5.359 [Google Scholar] [CrossRef]
[6]. Shimizu Y, Imaizumi H, Yamauchi H, Okuwaki K, Miyazawa S, Iwai T, Pancreatic fistula extending into the thigh caused by the rupture of an intraductal papillary mucinous adenoma of the pancreasIntern Med 2017 56:307-13.10.2169/internalmedicine.56.742228154275 [Google Scholar] [CrossRef] [PubMed]
[7]. Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi In patients with a soft pancreas, a thick parenchyma, a small duct, and fatty infiltration are significant risks for pancreatic fistula after pancreaticoduodenectomyJ Gastrointest Surg 2017 21(5):846-54.10.1007/s11605-017-3356-728101719 [Google Scholar] [CrossRef] [PubMed]
[8]. Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreasPancreatology 2006 6:17-32.10.1159/00009002316327281 [Google Scholar] [CrossRef] [PubMed]
[9]. Rosenberger LH, Stein LH, Witkiewicz AK, Kennedy EP, Yeo CJ, Intraductal Papillary Mucinous Neoplasm (IPMN) with extra-pancreatic mucin: a case series and review of the literatureJ Gastrointest Surg 2012 16:762-70.10.1007/s11605-012-1823-822258877 [Google Scholar] [CrossRef] [PubMed]