Delirium is an acute and transient brain disorder with disturbance of consciousness, attention and concentration defects in all areas of thinking, mood, perception, language, speech, sleep, psychomotor and cognitive domains [1,2]. The incidence of delirium in the Intensive Care Unit (ICU) is 16-80% globally [3]. The mean prevalence of delirium in the intensive care unit in Iran in 2013 has been reported as 44.5% [4].
Delirium is associated with complications including increased length of stay in hospital and ICU, increasing mortality rate from 22% to 72%, negative effect on six months survival and weaning from ventilator, nosocomial pneumonia, and danger of falling, urinary incontinence, skin disorders, permanent disability and lack of improvement in cognitive status [5]. Several factors can cause delirium in hospitalised patients in ICU [6], therefore interventions which modify these factors are effective on delirium [7]. Medicinal treatment is widely used in known cases of delirium [8]; but effectiveness and its impact on treatment outcome is different [9]. These medicines (sedatives, narcotics ...) can even worsen the patient’s psychological status and make delirium duration longer [10,11]. In contrast, non-medicinal interventions such as, soft music [12], family visits [13] massage therapy [14], noise reduction, the use of soft light at night, eye contact, repetitive touching [15] are effective in preventing delirium.
Since nurses are in long-term relations with the patients so their role in prevention, early diagnosis and treatment of delirium as an incompatible behaviour is essential [4,16]. Based on Roy adaptation model patients are able to achieve physiological [17] and psychological compatibility (self-perception, role playing, independence and dependence) [18].
The Roy adaptation Model is a model widely used in the identification of conceptual foundation of nursing. The development of the model began in the late 1960s [19]. Roy defined nursing as a scientific and humanistic profession and emphasised the importance of their specialised knowledge in contributing health needs and well-being of the community [20]. Delirium is one of the most common complications in the ICU [21,22]. Therefore, the evaluation and diagnosis of delirium in the ICU patients by the nurses using Roy adaptation model was necessary. With the following aim the present study was done to evaluate the effect of care plan based on Roy adaptation model on the incidence and severity of delirium in ICU patients.
Materials and Methods
This triple-blind randomised controlled trial was conducted on 100 hospitalised patients in ICU in Besat hospital (government, referral, hospital of Kurdistan University of Medical Sciences) Sanandaj, Iran from March to September 2016. For triple blinding of this study, the second researcher who measured Delirium, the statistician and the patients themselves did not have any information on the type of intervention in the groups. Two intensive care units of hospital were selected using simple random method. Sample allocation to groups and intervention was performed by the first researcher who was not blind to the study.
In relation to ethical considerations written consent to participate in the study was obtained from the subjects or their families. This study has been approved by the Ethics Committee of Kurdistan University of Medical Sciences (IR.MUK.REC.1394/326).
Inclusion criteria included; age over 18 years, GCS >7 and not having mental illness. Exclusion criteria included patient’s death during the study, transfer of patients within 24 hours of admission to other hospital wards, sedative drug injection and unwillingness to continue to participate in the study. Based on the previous studies [17,18], with 95% confidence interval and 10% probability of loss of the sample size of 50 was calculated in each group.
In control group (ICU), routine care was performed by nurses for patients. Routine care consisted of performing physician orders, daily assessment of consciousness, systematic evaluation of the patients, haemodynamic status.
In intervention group, before intervention nurses were trained for two hours in four sessions according to Roy adaptation model. The Roy adaptation model was described by face to face education and pamphlet training by a nurse, specialist in the ICU. Training included methods of identification and classification of main and underlying stimuli that were effective on behaviours physiologically and also detecting the features and symptoms of delirium as maladaptive behaviours of patients. After identifying maladaptive behaviours, the training of evaluating and identifying the main stimulants of delirium was trained to nurses such as water and electrolyte disorders, disturbing factors of sleep and rest, hypoxia, sensory stimuli such as light and sound. Nurses were trying to convert maladaptive behaviour (delirium) to adaptive behaviour in seven physiological dimensions by increasing, decreasing, or adjusting each trigger. These dimensions consisted of fluid and electrolyte balance, nutrition, sleep, activity and mobility, excretion, oxygen and circulation condition and endocrine regulations. The routine care was performed as in the control group and, if necessary, medical procedures as directed by physician and nursing interventions on the basis of patient’s needs without the use of nursing models.
The incidence and severity of delirium in both intervention and control groups were measured for seven days, two times a day in the morning (6-9 AM) and evening (6-9 PM). Data including demographic and clinical data were collected using questionnaire and delirium was measured by the NEECHAM Confusion Scale [Table/Fig-1]. NEECHAM scale was developed to measure the incidence and severity of delirium. It has a sensitivity of 87% and specificity of 95% [23]. In a study which aimed to determine the efficiency and effectiveness of NEECHAM for clinical screening of delirium its reliability was assessed as 0.96 Cronbach’s alpha coefficient and 0.99 Pearson coefficients [24]. NEECHAM for assessment of delirium in patients undergoing open heart surgery has been used in Iran [25]. The score in order to determine the incidence was set at 25. The scores less than 25 were considered as presence of delirium.
NEECHAM Confusion Scale [23,24].
| Subscale I level of responsiveness-information processing |
Attention and alertness (0-4 points) Verbal and motor response (0-5 points) Memory and orientation (0-5 points)
|
| Subscale II level of behaviour |
General behaviour and posture (0-2 points) Sensory motor performance (0-4 points) Verbal responses (0-4 points)
|
| Scores in order to determine the severity: |
0-19 points=moderate to severe confusion 20-24 points=mild or early development of delirium 25-30 points=not confused or normal function
|
Statistical Analysis
Data were analysed with the SPSS software version 21. Summarising and classifying the data was performed using descriptive statistics. Data analysis and hypothesis testing were conducted using statistical tests in order to compare variables between two intervention and control groups included; The Chi-squared was performed for gender, marital status, ventilation, the cause of hospitalisation, underlying diseases and incidence of delirium; the independent T-test for severity of delirium, age; Mann-Whitney test for Glasgow Coma Scale (GCS). The significance level was considered at p<0.05.
Results
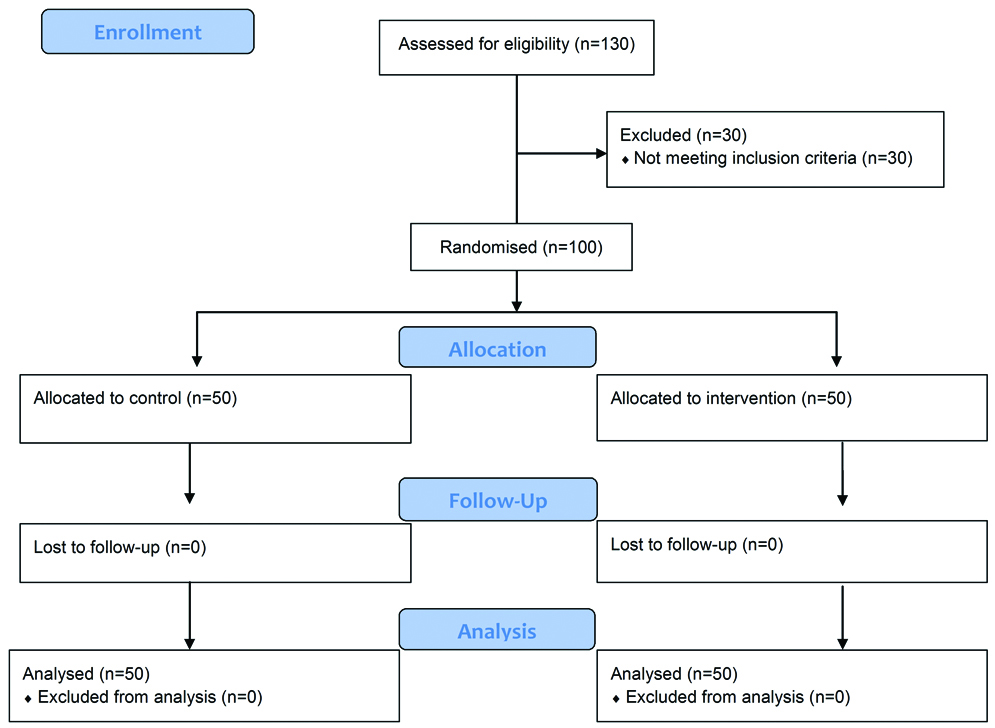
From 130 hospitalised patients in two ICUs 30 patients were excluded from the study as two patients had mental illness and 28 had GCS<7. Finally, total 100 patients were enrolled and in intervention and control group, 50 patients each were allocated [Table/Fig-2].
Flow diagram of the progress through the phases of the trial.
The mean age in control group was 46.6±21.67 (19-94) years and in intervention group was 48.9±23.48 (18-95) years. There was no significant difference between the two groups statistically in terms of age, gender, marital status, underlying disease, consciousness level or GCS (during the first and second days of the study) and being under ventilation [Table/Fig-3].
Comparison of background variables in the two groups.
| Background variables | Intervention group | Control group | p-value | Test |
|---|
| Consciousness level or Glasgow Coma Scale (GCS) | 12.14 | 11.03 | 0.162 | Mann-Whitney |
| The mean age | 48.9±23.48 | 46.6±21.67 | 0.612 | Independent T-test |
| Gender | Male | 38 (76%) | 35 (70%) | 0.449 | Chi-square |
| Female | 12 (24%) | 15 (30%) |
| Marital status | Married | 17 (34%) | 27 (54%) | 0.124 | Chi-square |
| Single | 20 (40%) | 15 (30%) |
| Widow | 13 (26%) | 8 (16%) |
| Ventilation | Yes | 15 (30%) | 15 (30%) | 0.586 | Chi-square |
| No | 35 (70%) | 35 (70%) |
| The cause of hospitalisation | Neurosurgery | 33 (66%) | 40 (80%) | 0.135 | Chi-square |
| SAH1 | 0 (0%) | 1 (2%) |
| Surgery | 16 (32%) | 9 (18%) |
| Other | 1 (2%) | 0 (0%) |
| Underlying diseases | Yes | 21 (42%) | 19 (38%) | 0.419 | Chi-square |
| No | 29 (58%) | 31 (62%) |
1Subarachnoid hemorrhage
Based on Chi-square test, the incidence of delirium from seventh day (p<0.008) and seventh night (p<0.05) in both intervention and control groups was significant, but from the first to sixth times of measurement, the difference was not significant (p>0.05). The incidence of delirium in the intervention group was less than the control group at different times [Table/Fig-4].
Comparison of incidence of delirium in the control and intervention groups (Chi-squared test).
| Day | Shift of Measurement | Group | Incidence of delirium | Level of difference between intervention and control groups |
|---|
| Yes | No |
|---|
| Frequency | Percent | Frequency | Percent | p-value |
|---|
| 1 | Morning | Control | 38 | 76% | 12 | 24% | 0.13 |
| Intervention | 37 | 74% | 13 | 26% |
| Night | Control | 41 | 82% | 9 | 18% | 0.62 |
| Intervention | 41 | 82% | 9 | 18% |
| 2 | Morning | Control | 41 | 82% | 9 | 18% | 0.27 |
| Intervention | 40 | 80% | 10 | 20% |
| Night | Control | 42 | 84% | 8 | 16% | 0.71 |
| Intervention | 41 | 82% | 9 | 18% |
| 3 | Morning | Control | 39 | 79.6% | 11 | 20.4% | 0.61 |
| Intervention | 36 | 73.5% | 14 | 26.5% |
| Night | Control | 42 | 84% | 8 | 16% | 0.59 |
| Intervention | 36 | 76.6% | 14 | 23.4% |
| 4 | Morning | Control | 38 | 79.2% | 12 | 20.8% | 0.31 |
| Intervention | 30 | 66.7% | 20 | 33.3% |
| Night | Control | 40 | 83% | 10 | 17% | 0.71 |
| Intervention | 25 | 50% | 25 | 50% |
| 5 | Morning | Control | 32 | 68.1% | 33 | 31.9% | 0.84 |
| Intervention | 22 | 48.9% | 28 | 51.1% |
| Night | Control | 37 | 77.8% | 13 | 22.2% | 0.55 |
| Intervention | 25 | 50% | 25 | 50% |
| 6 | Morning | Control | 23 | 54.8% | 27 | 45.2% | 0.12 |
| Intervention | 14 | 40% | 36 | 60% |
| Night | Control | 35 | 76.7% | 15 | 23.3% | 0.45 |
| Intervention | 17 | 37.8% | 33 | 62.2% |
| 7 | Morning | Control | 31 | 68.9% | 19 | 31.1% | *0.008 |
| Intervention | 15 | 36.6% | 35 | 63.4% |
| Night | Control | 30 | 61.9% | 20 | 38.1% | *0.05 |
| Intervention | 20 | 42.9% | 30 | 57.1% |
*significant difference
The severity of delirium in seven consecutive days was measured for two times. Based on Independent T-test the mean severity of delirium from fourth day (p=0.02) and fourth night (p=0.001) in both intervention and control groups was significant, but from the first to third day of measurement, difference was not significant (p>0.05). The mean severity of delirium in the intervention group was less than the control group at different times [Table/Fig-5].
Comparison of severity of delirium in the intervention and control groups at different days (Independent T-test).
| Day | Shift of Measurement | Group | Mean | SD | t | p-value |
|---|
| 1 | Morning | Control | 16.14 | ±7.69 | -1.79 | 0.075 |
| Intervention | 18.84 | ±6.92 |
| Night | Control | 15.51 | ±7.42 | -1.84 | 0.068 |
| Intervention | 18.11 | ±6.52 |
| 2 | Morning | Control | 15.75 | ±7.41 | -1.35 | 0.179 |
| Intervention | 17.71 | ±6.53 |
| Night | Control | 15.73 | ±7.21 | -1.256 | 0.212 |
| Intervention | 17.53 | ±6.21 |
| 3 | Morning | Control | 22.75 | ±7.48 | 0.593 | 0.555 |
| Intervention | 19 | ±7.16 |
| Night | Control | 16.89 | ±6.72 | -1.24 | 0.218 |
| Intervention | 18.68 | ±.39 |
| 4 | Morning | Control | 17.40 | ±7.27 | -2.236 | *0.028 |
| Intervention | 20.58 | ±6.23 |
| Night | Control | 16.78 | ±6.93 | -3.306 | *0.001 |
| Intervention | 21.35 | ±6.28 |
| 5 | Morning | Control | 18.17 | ±7.83 | -3.338 | *0.001 |
| Intervention | 22.91 | ±5.74 |
| Night | Control | 17.45 | ±7.88 | -3.707 | *0.000 |
| Intervention | 22.74 | ±5.80 |
| 6 | Morning | Control | 18.47 | ±7.63 | -3.425 | *0.001 |
| Intervention | 23.55 | ±6.22 |
| Night | Control | 18.11 | ±7.59 | -3.463 | *0.001 |
| Intervention | 23.32 | ±6.11 |
| 7 | Morning | Control | 19.56 | ±8.30 | -2.315 | *0.023 |
| Intervention | 23.36 | ±6.08 |
| Night | Control | 18.98 | ±7.94 | -2.686 | *0.004 |
| Intervention | 23.27 | ±6.14 |
*significant difference
Discussion
The present study was done to assess the effect of Roy adaptation model based care by nurses on the incidence and severity of delirium. Based on the results of this study, care plan based on Roy adaptation model managed to reduce the incidence and severity of delirium in intensive care patients in the physiologic aspects. Roy emphasises that the physiological adaptation is one of the factors that reduces the complications of the disease [17]. The goal of nursing is to promote adaptation in the four adaptive modes thus, contributing to health, quality of life, and dying with dignity by assessing behaviours and factors that influence adaptive abilities [19]. The four adaptive modes of Roy’s Adaptation Model are physiologic needs, self-concept, role function, and interdependence [19,22].
The results of other studies also showed that care plan based on Roy adaptation model increased the adaptation of patients. Borzou R et al., showed the effects of Roy’s adaptation model in nursing practice on the quality of life in patients with type II diabetes [26]. In a study by Maghsoudi E et al., the effect of care plan application based on Roy adaptation model on the self-efficacy in elderly people in Urmia nursing homes was evaluated [27]. In a study by Alimohammadi N et al., the Roy adaptation model care plan increased adaptation in patients with stroke in physiological dimension. They recommended that nurses can use this model for increasing patients’ adaptation [17]. The result of the present study was consistent with these studies.
Naeim Hassani S et al., concluded that using an educational program based on Roy adaptation model can be effective on the psychological adaptation and reduction of maladaptive behaviours in patients with heart failure [18]. Moreover, the results of the study carried out by Rogers C et al., on investigating the effect of Roy’s adaptation model on improving physical activities of the elderly showed that performing regular exercises like yoga based on Roy’s adaptation model could result in positive changes in different aspects of the elderly like improvement of physiological conditions, self-concept, independence, and self-efficacy [28], however this study is similar to the present study, but they evaluated the effect of care plan based on the Roy adaptation model to improve psychological adaptation in patients where we evaluated the effect of care plan based on the Roy adaptation model to improve physiological adaptation in patients. This shows the flexibility of Roy adaptation model which can be used according to the patient’s condition and environment and justifies its use in reducing delirium in the ICU.
Although, no study was found that studied the effect of Roy adaptation model on delirium in patients hospitalised in ICU, but several studies had been conducted concerning the use of nursing interventions to prevent or reduce the incidence and severity of delirium [16,21,29,30]. Kalani Z et al., evaluated the impact of multi-factorial interventions on the incidence of delirium in patients hospitalised in ICU in Shiraz, Iran. They showed that interventions had no effect on the incidence of delirium, but because cognitive scores in the intervention group significantly increased compared with control group. They concluded that it is better to consider these interventions as a non-pharmacological and safe method in CCU patients to prevent incidence of delirium [31]. In our study, care plan based on Roy adaptation model reduced the incidence and severity of delirium affect.
In the present study, the highest severity of delirium on different days in the morning and evening, was on the fourth day in both the intervention and control groups and over time the incidence of delirium decreased in both groups on the seventh day. The incidence of delirium in the night shift was less than day shift. Jannati Y et al., reported the highest incidence of delirium in the early days of hospitalisation [25]. In our study, the highest incidence of delirium was on the fourth day. With regard to the Delirium Measurement Tool based on NEECHAM, the higher the scores and the upward movement of the chart, indicate a decrease in delirium and improvement of the patients. These differences reflect the type of disease, type of nursing care, the number of samples and different environmental condition.
The important point in our study was controlling and organising different nursing interventions alongside medical and pharmaceutical interventions in the form of care model, which managed to decrease the incidence and severity of delirium in the ICU.
Limitation
The limitation of the present study was inability to evaluate patients in all aspects of Roy adaptation model that included self-perception, role playing, independence and dependence separately.
Conclusion
The care plan based on Roy adaptation model reduced the incidence and severity of delirium in patients hospitalised in ICU. Given that a set of factors are involved in the occurrence of delirium, therefore to reduce the incidence and severity of delirium an organised and structured nursing care is required. Using Roy adaptation model to modify incompatible behaviours in ICU patients is recommended.
1Subarachnoid hemorrhage
*significant difference
*significant difference